Hemorrhagic stroke - what is it? Symptoms, treatment and prognosis
Hemorrhagic stroke, acute cerebrovascular accident (ACVA) of the hemorrhagic type is an acute clinical syndrome that is a consequence of damage to cerebral vessels and hemorrhage in the brain. The root cause may be damage to either an artery or a vein. The larger the damaged vessel, the more profuse the bleeding; in severe cases, up to 100 ml of blood is poured into the tissue. The resulting hematoma mechanically compresses and displaces the nervous tissue, and swelling quickly develops in the affected area.
If the victim is not provided with medical assistance within three hours, the chances of survival rapidly decrease and tend to zero. According to statistics, hemorrhagic strokes account for just over 20% of stroke cases.
What it is?
Hemorrhagic stroke is an acute hemorrhage in the brain due to rupture or increased permeability of blood vessels. This cerebrovascular accident differs from classic (ischemic) stroke, which is more common (70% of patients).
The nature of changes in blood vessels during an ischemic stroke is the blockage of their lumen by blood clots, resulting in gradual necrosis of brain cells, and in a hemorrhagic stroke there is a violation of the integrity of the vascular wall, as a result of which the brain tissue is saturated and compressed by the gushing blood.
Hemorrhagic cerebral stroke is a dangerous and insidious disease. It is characterized by:
- High mortality (60–70% of patients die within the first week after the onset of the disease).
- Suddenness (in 60–65% of patients, hemorrhage occurs without any previous symptoms).
- Profound disability of surviving patients - 70–80% of people are bedridden and cannot care for themselves, the remaining 20–30% have a less pronounced neurological deficit (the function of the limbs, walking, speech, vision, intelligence, etc. is impaired)
More than 80% of brain hemorrhages are associated with increased blood pressure (hypertension). By taking antihypertensive drugs (blood-lowering drugs), you can reduce the risk of stroke, the amount of hemorrhage and the severity of brain damage. If patients are admitted to a medical facility within the first 3 hours, this increases the chances of survival. Specialized rehabilitation centers help restore lost brain functions as much as possible after a stroke. Complete cure is rare, but possible.
Prevention
The disease is extremely serious and dangerous. It is much easier to avoid it than to treat it later. Prevention measures include:
Blood pressure control
- proper nutrition;
- monitoring weight changes (especially when you are overweight);
- control of blood pressure, preventing its increase;
- fight against atherosclerotic phenomena;
- getting rid of bad habits - smoking, alcohol;
- If possible, avoid stress and overexertion.
To prevent relapse, restorative and vitamin preparations are prescribed. Constant supervision by a specialist is required.
Classification
It should be noted that a brainstem stroke results in almost instantaneous death. Only in rare cases is it possible to save the patient’s life with such a diagnosis. At the same time, there is no likelihood of returning to a full life.
The brain stem is the center of all body systems and is directly connected to the spinal cord. It serves as a link between the commands of the brain centers and the nerves of the body: it is thanks to it that we are able to move, breathe, swallow, see, hear, and so on. The brain stem also regulates the circulatory system, thermoregulation, and heartbeat. That is why damage to it during a stroke most often leads to death.
Based on their origin, primary and secondary hemorrhagic stroke are distinguished:
| Primary | provoked by a hypertensive crisis or thinning of the walls of arteries and veins due to prolonged stress on them (for example, due to high blood pressure, physical and nervous overload, etc.) |
| Secondary | provoked by the rupture of an aneurysm, hemangioma and other vascular deformations and anomalies (malformations), congenital or formed in the process of life. |
Depending on the localization zone, I distinguish the following types of hemorrhagic stroke:
- Subarachnoid - hemorrhage into the space between the hard, soft and arachnoid membranes of the brain;
- Hemorrhage on the periphery of the brain or in the thickness of its tissue;
- Venticular hemorrhage - localized in the lateral ventricles;
- Combined type: occurs with extensive hemorrhage affecting several areas of the brain.
Peripheral hemorrhage is much less dangerous than intracerebral hemorrhage, which inevitably provokes the formation of hematomas, edema and subsequent death of brain tissue. Hematomas are also distinguished by location:
- Lobar - the hematoma is localized within one lobe of the brain, without going beyond the cerebral cortex.
- Medial - hemorrhage damages the thalamus.
- Lateral – damage to the subcortical nuclei localized in the white matter of the hemispheres (fence, amygdala, caudate, lenticular nuclei).
- Mixed - hematomas affecting several areas of the brain at once are most common.
Clinical manifestations
Symptoms of hemorrhagic stroke are varied and are divided into two large groups: general cerebral and focal. Also, the symptoms strongly depend on the location of the hemorrhage, its size, the somatic condition of the patient and many other factors.
General cerebral symptoms of hemorrhagic stroke include the following:
- Impaired consciousness (stunning, stupor, coma). The larger the focus, the lower the level of consciousness. However, with damage to the brain stem, even a small focus of hemorrhage leads to severe depression of consciousness.
- Dizziness.
- Nausea, vomiting.
- Headache.
- General weakness.
- Breathing disorders.
- Hemodynamic disorders.
Predominantly focal symptoms include the following:
- Paresis or plegia in the limbs, hemiparesis is more common.
- Paresis of facial muscles.
- Speech disorders develop mainly with damage to the left temporal lobe.
- Visual impairment (including the development of anisocoria).
- Hearing impairment.
A stroke should be suspected if the patient has any type of speech impairment, weakness in the arm and leg on one side, the development of epileptic seizures without provoking factors (for example, such factors include alcohol consumption), impaired consciousness up to coma. In any suspicious cases, it is better to play it safe and call an ambulance. Behavior and assessment of the situation when a stroke is suspected should be considered in a separate article.
Precursor symptoms
The preceding signs or so-called aura do not always develop. This is rather an exception to the rule, since in most cases the opposite is observed.
Hemorrhage occurs suddenly. If we talk about manifestations that will indicate the approach of an emergency condition, they can be as follows:
- Intense heat in the chest, flushing of the face. A sudden sensation that comes out of the blue. As a rule, there are no objective reasons.
- Numbness of half the face. In addition, tingling may occur. Paresthesias indicate sudden, acute ischemia. This is a very alarming sign, even if nothing followed after it. You need to pay close attention to such “calls” and urgently run to the doctor.
- Problems with speech perception. The native language that a person has spoken for many years suddenly turns out to be incomprehensible. This is the first sign of a malnutrition of the temporal lobes of the brain, into which blood may bleed.
- Problems with coordination of movements. Acute dizziness. May result in a fall and injury.
Attention:
Aura or precursors of a pathological process occur in only 5-10% of the total number of cases. Much more often, the disorder debuts directly from the main clinic.
All possible symptoms of pre-stroke in women are described in detail here.
Coma due to hemorrhagic stroke
Approximately 90% of patients with GI in a state of stupor or coma die in the first five days, despite intensive therapy. Disorders of consciousness are characteristic of many pathologies, manifested by inhibition of the functions of the reticular formation of the brain.
Brain dysfunctions develop under the influence of:
- Endo- and exotoxins – derivatives of the end products of metabolism;
- Oxygen and energy starvation of the brain;
- Metabolic disorders in brain structures;
- Expansion of the volume of brain matter.
The most important factors in the development of coma are acidosis, cerebral edema, increased intracranial pressure, and impaired microcirculation of brain fluids and blood.
The state of coma affects the functioning of the respiratory system, excretion (kidneys) and digestion (liver, intestines). It is impossible to recover from a coma at home, and it is very difficult even in intensive care conditions.
The clinical definition of coma is carried out using the GCS (Glasgow Coma Scale), and some other methods that are important for clinicians are used. There are precoma and four stages of coma. The easiest is the first, and the hopeless state of the patient corresponds to the fourth stage of coma.
Treatment
Stroke therapy in the acute period may include:
- Pain relief, correction of body temperature (paracetamol, efferalgan, naproxen, diclofenac, often opiates, propafol). Aspizol, dantrolene are given intravenously, and magnesium sulfate is given by drip.
- Reducing blood pressure, which helps stop bleeding in the brain. For this purpose, drugs are administered intravenously: labetalol, nicardipine, esmolol, hydralazine. However, a sharp decrease in pressure in the first days is not allowed. Next, tablet drugs are prescribed - captopril, enalapril, capoten (as basic therapy orally or through a tube).
- Diuretics for persistent high blood pressure (chlorothiazide, andapamide, Lasix), calcium antagonists (nimotop, nifedipine).
- In case of severe hypotension, vasopressors are prescribed by drip (norepinephrine, mesaton, dopamine).
- Often, a continuous intravenous infusion is used to administer the above drugs, monitoring the pressure level every 15 minutes.
- To reduce cerebral edema, dexamethasone is recommended for 3 days (intravenously). If the swelling progresses, glycerin, mannitol, albumin, and refortan are injected dripwise.
- Often, a continuous intravenous infusion is used to administer the above drugs, monitoring the pressure level every 15 minutes.
- Drugs for the correction of neurological symptoms (sedatives - diazepam, muscle relaxants - vecuronium).
- Local therapy is aimed at eliminating bedsores and includes treating the skin with camphor alcohol and sprinkling with talcum powder.
- Symptomatic therapy - anticonvulsants (lorazepam, thiopental or anesthesia for 1-2 hours), medications for vomiting and nausea (metoclopramide, torecan), against psychomotor agitation (haloperidol). For pneumonia and urological infections, a course of antibacterial treatment is carried out.
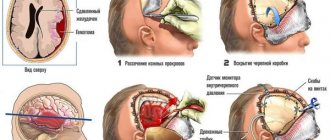
In the presence of large hematomas (more than 50 ml), surgical intervention is performed. Excision of the hemorrhage site can be carried out if it is localized in an accessible part of the brain, and also if the patient is not in a comatose state. Most often, clipping of the aneurysm neck, puncture-aspiration elimination of the hematoma, its direct removal, as well as ventricular drainage are used.
Publications in the media
Acute traumatic subdural hematoma is an accumulation of blood in the space between the inner layer of the dura mater and the arachnoid membrane of the brain. Patients with acute traumatic subdural hematoma typically exhibit significantly greater primary brain damage than patients with epidural hematoma, and therefore treatment outcomes for this group of patients are significantly poorer.
Etiology and pathogenesis • Accumulation of blood around the source of bleeding in the area of the brain crush (usually the pole of the frontal and temporal lobes). In this case, there is significant primary damage to the entire brain, there is no “bright gap”, general cerebral symptoms dominate in the form of a gross disturbance of consciousness • Rupture of the “bridge” veins as a result of a sudden movement of the head during acceleration/deceleration. Primary brain damage is smaller and there may be a “bright period” followed by rapid deterioration. It should be remembered that in patients receiving anticoagulants, the risk of developing a subdural hematoma is significantly higher (7 times in men and 26 times in women compared with the general population). In such patients, even a minor injury can lead to a life-threatening hematoma.
The clinical picture is nonspecific and reflects the severity of primary TBI; sometimes a variant of the course with a “light” interval is observed (see Epidural hematoma).
Diagnostics. CT scan reveals a crescent-shaped space-occupying formation located between the convexital surface of the brain and the inner plate of the bones of the calvarium. Depending on the age of the hematoma, the signal intensity varies greatly
• 1–3 days (acute hematoma): the density on CT is high.
• From 4 days to 2–3 weeks (subacute hematoma): density similar to that of brain tissue.
• From 3 weeks to 3 months (chronic hematoma): low density (approaching the density of cerebrospinal fluid).
• More than 3 months: may take the form of a lens (like an epidural hematoma), the density is higher than that of cerebrospinal fluid, but lower than that of fresh blood.
Treatment. In most cases, acute subdural hematoma requires emergency surgical intervention - craniotomy, removal of the hematoma. The absolute indication for surgery is a hematoma more than 1 cm thick according to CT data. In the postoperative period, intensive therapy is required to support vital functions and control the level of ICP (should be less than 25 mm Hg) - mannitol, ventricular drainage, barbiturates, hyperventilation.
Forecast. The mortality rate is 50–90%, but it should be borne in mind that it is primarily due to the primary traumatic brain injury and not to the hematoma itself. In elderly patients (over 60 years of age) and in patients receiving anticoagulants, mortality approaches 90–100%. Recently, factors influencing the prognosis of acute traumatic subdural hematoma have been intensively studied. Independent factors that reliably influence the prognosis: • Mechanism of injury: the worst prognosis for a motorcycle injury: without a helmet, mortality is 100%, with a helmet - 33% • Age over 65 years significantly worsens the prognosis (mortality 82%, “functional” survival 5%) • Postoperative ICP level: less than 20 mm Hg. — mortality 40%, more than 45 mm Hg. — almost 100% • Neurological status at the time of admission to a specialized hospital.
Mortality and “functional” survival (i.e., with preservation of at least the ability to self-care) depending on the severity of TBI • 3 points on the Glasgow scale (mortality 90%, “functional” survival 5%) • 4 points on the Glasgow scale (mortality 76%, “functional” survival 10%) • Glasgow score 5 (mortality 62%, “functional” survival 18%) • Glasgow score 6–7 (mortality 51%, “functional” survival 44%)
Chronic subdural hematoma, despite its external similarity with acute subdural hematoma, has a number of significant differences.
Chronic subdural hematoma
Epidemiology. Chronic subdural hematoma usually occurs in older people (average age 63 years). In less than 50% of them, a history of TBI can be identified. In 20–25% of cases, chronic subdural hematoma is bilateral.
Risk factors • Alcoholism • Epilepsy • Shunt surgery for hydrocephalus • Coagulopathy.
Etiology and pathogenesis. It is believed that a chronic subdural hematoma forms from an undetected (most likely minor) acute subdural hematoma. Blood entering the subdural space causes an inflammatory reaction, fibrin falls out and a hematoma capsule is formed. Subsequently, vascularization of the capsule, fibrinolysis and “liquefaction” of the blood clot in the center of the hematoma occur. The course of the hematoma is determined by the ratio of the processes of plasma filtration from the capsule and microhemorrhages into the cavity on the one hand and reabsorption of the contents of the hematoma on the other.
The clinical picture is very variable: from minimal manifestations (prolonged headaches, increasing dementia and behavioral disorders) and symptoms reminiscent of transient ischemic attacks, to the development of seizures, hemiplegia and coma (an extremely unfavorable course). In many cases, it is not possible to make a correct diagnosis until a brain CT scan is performed.
Diagnosis: CT or MRI of the brain. In some cases, MRI is more informative (for example, in patients with so-called “isodensity” bilateral hematomas, when the hematoma is indistinguishable in density from the brain parenchyma, and there is no dislocation of the midline structures.
Treatment. All symptomatic hematomas and asymptomatic hematomas larger than 1 cm are subject to surgical treatment. The purpose of the operation is to remove the liquid component of the hematoma (a minor operation through a burr hole that can be performed under local anesthesia). Removal of the capsule is not indicated in most cases, because significantly increases surgical trauma and may cause additional gross neurological deficits. Before surgery, a study of the hemostasis system is required and any violations identified are corrected. The advisability of prophylactic administration of anticonvulsants is debatable, because this does not affect the risk of developing “late” seizures.
Forecast. An improvement in the neurological status is observed in almost all patients immediately after drainage, and there is a pattern: the higher the pressure in the hematoma, the more pronounced the clinical effect will be. Mortality, according to various authors, ranges from 0 to 8% and is determined primarily by the general condition of the patient, and not by the fact of hematoma drainage itself. On control CT scans performed on the 10th day after surgery, remnants of the hematoma are detected in 78% of cases, after 1.5 months - in 15%. Indications for repeated drainage are an increase in the volume of hematoma remnants and deterioration of the patient’s neurological status.
ICD-10. I61 Intracerebral hemorrhage
Consequences
If patients can be saved, they experience neurological deficits—symptoms caused by damage to the area of the brain where the hemorrhage occurred.
These may be consequences of a hemorrhagic stroke:
- paresis and paralysis - impaired movement of the limbs on one half of the body, since they are constantly in a half-bent position and it is impossible to straighten them;
- speech impairment and its complete absence;
- mental disorders and irritability;
- constant headaches;
- movement coordination disorders;
- inability to walk or even sit independently;
- visual impairment up to complete blindness;
- facial distortion;
- vegetative state - the absence of any signs of brain activity (consciousness, memory, speech, movements) with preserved breathing and heartbeat.
Symptoms of the disease and their duration depend on the location of the hemorrhage and its volume. The first 3 days are the most dangerous, since during this time severe disorders occur in the brain. Most deaths (80–90%) occur during this period. The remaining 10–20% of patients die within one to two weeks. Patients who survive recover gradually from a few weeks to 9–10 months.
Symptoms of cerebral hemorrhage
When a person has a cerebral hemorrhage, one should not hesitate under any circumstances! Of course, he won’t help himself, but if you notice the symptoms presented below in a loved one, you need to urgently go to the hospital.
- Partial loss of consciousness, confusion;
- Severe nausea and vomiting lasting several days or more;
- A sharp headache that is strong enough to knock a person off his feet;
- Visual impairment, which is accompanied by “flickering pictures, floating objects.” Focusing on the subject does not occur;
- Pupil size varies;
- Complete loss of balance and coordination;
- Partial paralysis, loss of sensitivity of the limbs.
- Hemorrhagic cerebral stroke: what it is, symptoms and consequences
If you notice 2-3 symptoms or more in yourself or another person, consult a doctor immediately. When you get to him, you will need to go through the following diagnostic stages:
- Survey. The patient will be interviewed and asked about his condition and well-being. If he cannot answer the questions, then the answers should be given by relatives or accompanying people;
- Conducting a reflex test. If there are deviations, the diagnosis will be continued further. If not, then it will also be continued further, but in a more simplified form;
- Checking pulse and blood pressure. Taking an ECG on the machine;
- Checking the presence of erythrocytes in the sample after lumbar puncture;
- MRI;
- Study of the vascular network - angiography.
Left-hand side
If the left side is affected, the consequences are characterized by disruption of the right side of the body. The patient experiences complete or partial paralysis, and not only the leg and arm are affected, but also half of the tongue and larynx. Such patients develop gait disturbances and a characteristic posture of the right hand (folded in a boat).
The victim experiences deterioration in memory and speech, and the ability to clearly express thoughts is impaired. Damage to the left hemisphere of the brain is characterized by problems with recognizing time sequences; it cannot decompose complex elements into components. Impairments in written and oral speech appear.
Right side
If the right side is affected, the most dangerous consequence is damage to the brain stem, in which a person's chances of survival are close to zero. This department is responsible for the functioning of the heart and respiratory system.
Diagnosing a hemorrhagic stroke on the right is quite difficult, since the centers of orientation in space and sensitivity are located in this part. This lesion is determined by speech impairment in right-handed people (in left-handed people the speech center is located in the left hemisphere). In addition, there is a clear relationship: if the functionality of the right half of the brain is impaired, the left side suffers and vice versa.
How long do they live after a hemorrhagic stroke?
The prognosis of hemorrhagic stroke is unfavorable. It depends on the location and extent of the lesion. Hemorrhage into the brainstem is dangerous, which is accompanied by respiratory failure and a sharp, poorly corrected by drugs, decrease in blood pressure to critical levels. Hemorrhage into the ventricles with their breakthrough is severe and often ends in death.
How long do people live with hemorrhagic stroke? This pathology is fatal in 50-90% of cases. Death may occur on the very first day - against the background of generalized convulsions, when breathing is impaired. More often, death occurs later, by 2 weeks. This is due to a cascade of biochemical reactions triggered by the outpouring of blood into the cranial cavity and leading to the death of brain cells. If there is no displacement of the brain, no herniation (entry into a bone hole), no breakthrough of blood into the ventricles, and the compensatory capabilities of the brain are sufficiently large (this is more typical for children and young people), then the person has a great chance of survival.
At 1-2 weeks, in addition to neurological disorders, complications associated with the immobility of the patient, exacerbation of his chronic diseases or connecting him to an artificial respiration apparatus (pneumonia, bedsores, liver, kidney, cardiovascular failure) occur. And if they do not lead to death, then by the end of 2-3 weeks the cerebral edema will stop. By week 3, it becomes clear what the consequences of a hemorrhagic stroke are in this case.
Diagnostics
There is not much time for examination. It is necessary to urgently take the person to the hospital, study his general condition and begin action.
The emergency list of activities is as follows:
- Blood pressure measurement.
- Quickly interview the patient if he is conscious.
- Listening to heart sounds.
- Basic neurological examination. Checking reflexes.
Next, primary measures are taken to restore the functional activity of the body. Once the condition becomes stable, there is time to study the situation in more detail.
Special examinations are prescribed:
- Anamnesis collection.
- Doppler ultrasound of the brain. Duplex scanning of vessels of cerebral structures. To assess the quality of local blood flow.
- REG. In order to identify the electrical activity of nerve tissue.
- MRI. To assess the extent of damage and prospects for recovery. Develop treatment tactics.
- Hormone analysis, as well as blood biochemistry with an expanded picture of the lipid spectrum.
Diagnosis is carried out under the supervision of a neurologist. A cardiologist, neurosurgeon, and endocrinologist are also involved, if necessary.
Time is running out. The first few days and even months there is a real risk of relapse. No one survives a second hemorrhagic stroke.
Read the full algorithm for providing first aid for a stroke here.
Recovery after a stroke
The rehabilitation period after a hemorrhagic stroke is long, especially in old age. It depends on the lost functions and does not guarantee their complete rehabilitation. Lost abilities are restored most quickly in the first year after a stroke, then this process is slower. The neurological deficit that remains after three years will most likely remain for life.
Neurologists and rehabilitation specialists are ready to help restore lost functions as much as possible. For this:
- classes are held with a psychologist or psychotherapist;
- if reading/writing skills are lost, classes are held to restore them;
- hydrotherapy is carried out (massage in the pool, light exercises in the water);
- classes on special simulators;
- if speech reproduction is impaired, the person will have to work with a speech therapist; for paresis or paralysis, physiotherapy is carried out (for example, on the Myoton apparatus), massage and exercise therapy are performed with an instructor;
- drugs are prescribed that will help restore lost neural connections (“Cerakson”, “Somazina”), reduce high blood pressure (“Enalapril”, “Nifedipine”), antidepressants and sedatives;
- color therapy - treatment with visual images.
The prognosis for recovery depends on how large the area was covered by the hemorrhage, as well as on how qualified the actions of doctors and rehabilitation specialists were. Hemorrhagic stroke is a very complex pathology, the consequences of which are unlikely to be completely eliminated. Maintenance treatment and rehabilitation continue for a very long time.
Period of return to normal life
Rehabilitation after hemorrhagic stroke is carried out according to plan in medical institutions of various specialties:
- For 1 month, patients are treated in the neurological or neurovascular department of the hospital.
- Then they receive rehabilitation treatment in the rehabilitation department for another 1 month.
After this, doctors evaluate how successful the treatment was. Depending on the preliminary results, the patient is offered different programs for further recovery.