Risk factors for stroke and heart attack
Planning a preventative treatment regimen is based on addressing risk factors that are largely similar for heart attack and stroke.
Metabolic risk factors include:
- dyslipidemia (impaired lipid metabolism - organic compounds, including fats and fat-like substances);
- arterial hypertension;
- obesity;
- metabolic syndrome;
- diabetes mellitus and other endocrinopathies;
- coagulopathies (diseases that develop as a result of disorders of the blood coagulation and anticoagulation systems).
Common markers of heart attack and stroke are:
- previous cardiovascular diseases;
- peripheral vascular pathology;
- calcium index;
- stress test results;
- hypertrophy (thickening of the wall) of the left ventricle.
Atherosclerotic stenosis of the carotid arteries and brain tumors increase the risk of stroke. The provoking factors of a heart attack are:
- atrial fibrillation;
- dysplasia (developmental disorder) of connective tissue;
- arteritis;
- diabetes.
Although the incidence of stroke is higher in men, it is more severe in women, and about half of deaths from stroke occur in women.
Make an appointment
Swelling of the hands. Causes and treatment of hand swelling
Fluid retention in soft tissues, including in the hands, causing them to swell or swell, can be explained by a number of reasons, in particular: cardiovascular diseases; kidney or liver diseases; diseases of endocrine organs; stagnation; poor diet, consuming large amounts of liquid, salt or sugar. Pregnancy can be a provoking factor for the appearance of edema in women. Treatment of hand swelling, which involves preventing the accumulation of lymphatic fluid, is carried out after a thorough examination and a clear diagnosis. An experienced osteopath can do this even without special equipment. Osteopathic treatment has virtually no contraindications and is therefore suitable for most patients.
Swelling of the hands is the result of a fluid called interstitium that accumulates in the hands. Edema can be unilateral or bilateral, and can develop gradually or suddenly. With immobility, the swelling usually increases, and with exercise or raising your arms, it decreases. The following causes of hand swelling can be identified: allergic reactions, when hand swelling was caused by some allergen; disturbances in the functioning of the central nervous system; with superior vena cava syndrome; with thrombophlebitis, rather painful swelling of the hands occurs; hand injuries can subsequently lead to swelling of the hands; burns; immunological diseases; intoxication that occurs as a result of an attack by a poisonous animal. In order to get rid of hand swelling, you should consult a doctor and follow all his instructions.
Signs of a stroke
To diagnose cerebral blood supply disorders, it is necessary to use stroke recognition techniques:
- When trying to smile, you need to pay attention to the corners of the mouth - in case of a stroke, it can be directed downwards, the smile looks crooked and asymmetrical;
- When trying to speak, it may be difficult to pronounce even the simplest words and sentences;
- When trying to raise both arms, asymmetry is observed;
- The protruding tongue falls to the side.
If at least one of the symptoms is positive, you must immediately call an ambulance. Under no circumstances should you give him water, feed him, lift him, or take him by handy transport to the nearest hospital, as this can cause harm.
Help in the acute period
Which doctors are needed in the treatment of stroke depends on the period of the disease, but in any case, they must be experienced, highly qualified specialists who know how to properly provide assistance in this situation.
When diagnosing an ischemic stroke in a patient, the doctor’s goal is to restore blood supply with subsequent rehabilitation. This may require blood thinning medications or mechanical removal of the clot using a catheter. To remove atherosclerotic plaques, endarterectomy is performed, and to increase the diameter of blood vessels, plastic surgery with stenting is performed.
How long to stay in hospital if you have a stroke
Poor blood circulation in the brain, in other words, stroke, treatment involves three stages:
- prehospital;
- stay in the intensive care unit;
- treatment in a general ward.
The length of stay of a patient in a hospital, according to treatment standards, is 21 days, provided the patient has no violations of vital functions, and 30 days in case of serious violations. When the length of a patient’s stay in a hospital is insufficient, a medical examination is carried out followed by the development of an individual course of rehabilitation.
All patients diagnosed with stroke are subject to hospitalization. The length of stay in intensive care depends on a number of factors, including:
- depression of vital functions;
- degree of damage to brain tissue. With a major stroke, patients stay in intensive care longer;
- the need for constant monitoring if there is a high risk of recurrent stroke;
- severity of the clinical picture;
- level of depression of consciousness and others.
Basic and differentiated therapy
Treatment of a patient in the intensive care unit involves basic and differentiated therapy.
Basic treatment is aimed at:
- fight against cerebral edema;
- restoration of normal functioning of the respiratory system;
- patient nutrition;
- maintaining hemodynamics at an acceptable level.
Differentiated therapy involves:
- normalization of arterial and intracranial pressure, elimination of cerebral edema after hemorrhagic stroke. In the first two days, a decision is made regarding the need for surgery. Neurosurgeons at the Yusupov Hospital daily perform surgical interventions to eliminate the consequences of stroke and save the lives of hundreds of patients. All manipulations are carried out using modern medical equipment using effective proven techniques;
- accelerating metabolic processes, improving blood circulation and increasing the resistance of brain tissue to hypoxia when diagnosed with ischemic stroke. The length of stay in intensive care directly depends on the timely and adequate course of treatment.
In most cases, young people recover much faster than older patients.
It is possible to transfer a victim from the intensive care unit to a general ward after meeting a number of criteria:
- the patient can breathe independently, without the support of devices;
- the patient is able to call a nurse or doctor for help;
- there is a stable level of heart rate and blood pressure;
- the possibility of bleeding is excluded.
Only after the patient's condition has stabilized can the doctor transfer the patient to the ward. In a hospital setting, various rehabilitation procedures are prescribed to quickly restore lost functions.
In the neurology department of the Yusupov Hospital, patients are not only developed an individual course of rehabilitation therapy, but also given psychological support.
If necessary, psychologists work with loved ones and relatives of the patient to teach them the basics of caring for a person who has suffered a stroke.
Treatment of patients who have had a stroke
During the first month, according to various authors, 15-30% of patients with ischemic stroke and 30-70% of patients with hemorrhagic stroke die, so after a month, on average, 65-80% of stroke patients remain alive [3]. Based on this, the number of patients who have had a stroke (or survived the first month of the disease) is about 300 thousand people in Russia every year. In the treatment of patients who have suffered a stroke, two main directions can be distinguished:
• treatment of stroke consequences,
• prevention of recurrent stroke and other diseases of the cardiovascular system.
Motor impairment is one of the most common and severe consequences of stroke. Recovery of lost movements is maximum within two to three months after the stroke, it continues throughout the year and is most significant in the first six months. A year after the onset of a stroke, a decrease in the degree of paresis is unlikely, but it is possible to improve motor functions and reduce disability by training balance and walking, using special devices for movement, and reducing increased muscle tone (spasticity) in paretic limbs. Restoration of the ability to move independently is observed even in patients in whom a stroke leads to a complete absence of movement in the limbs on one side (hemiplegia). With adequate physical therapy, most of these patients begin to stand and walk independently at least 3-6 months after the disease, which is one of the main goals of rehabilitation for severe motor disorders [3]. The absence of independent walking 3-6 months after a stroke may be caused by the loss of deep sensitivity in paretic limbs and (or) low motivation of the patient for rehabilitation, which is often observed when the non-dominant (right in right-handed people) hemisphere of the brain is damaged and is combined with an underestimation of the severity of the disease or ignoring it (anosognosia).
The leading importance in case of movement disorders is therapeutic exercises, which in the form of passive movements in paralyzed limbs should be carried out already in the first days after the stroke after stabilization of neurological disorders and in the absence of contraindications to physical activity (for example, myocardial infarction or cerebral artery aneurysm). Passive movements in paralyzed limbs should be carried out for several (10-20) minutes at least three times a day, special attention should be paid to the joints (shoulder, elbow, hip and ankle), in which early and significant development of contracture and periarteritis is possible. Active movements in paretic limbs must be trained immediately after their appearance, gradually increasing the load. In the absence of contraindications, patients should sit up in bed 2-3 days after the development of an ischemic stroke and one to two weeks after the occurrence of intracerebral hemorrhage. Then, if they sit confidently in bed, patients can sit in a chair or chair and learn to stand and use a wheelchair. In the future, patients should be taught to walk, using first special devices and then a stick. When conducting physical therapy, a gradual increase in physical activity is necessary. If the patient has a concomitant cardiac pathology (for example, arrhythmia or angina), then the rehabilitation program is coordinated with a cardiologist.
In the absence of significant restoration of motor functions in the arm, the patient is recommended to wear a fixation scarf, preventing free hanging of the arm, which can lead to subluxation in the shoulder joint and the development of periarteritis. To prevent contracture and deformation of the wrist and/or ankle joints, as well as during their development, you can use an orthopedic device for the lower leg and a special splint that holds the wrist joint and hand in the correct position.
Most patients after a stroke experience an increase in muscle tone similar to spasticity in paretic limbs. In many cases, spasticity impairs motor functions, because paresis is often caused not only by muscle weakness, but also by increased tone of antagonist muscles [3,4]. Spasticity is often accompanied by painful muscle spasms in paretic limbs, contributes to the development of contracture and deformation of the limb, and makes it difficult to care for an immobilized patient. In such cases, reducing spasticity can improve motor functions, prevent or reduce contractures and deformities of the limbs, and facilitate patient care.
Oral antispastic agents can be used to treat spasticity in stroke patients. Treatment begins with a minimum dose of the drug, then gradually increases it until the effect is achieved. Baclofen is used at 10-50 mg/day, tizanidine at 6-30 mg/day and tolperisone at 150-300 mg/day. Antispastic drugs in most cases reduce muscle tone in paretic limbs and relieve painful muscle spasms, facilitating physical therapy and preventing the development of contractures. However, increasing the dose of antispastic agents required to significantly reduce spasticity often leads to significant muscle weakness and sedation, which limits their use in many ambulatory patients. These side effects are not so significant for bedridden patients, therefore, in them, antispastic drugs more often than in walking patients bring a significant effect, facilitating their care, preventing or eliminating contractures, muscle spasms and cosmetic defects in paretic limbs.
In recent years, in the treatment of spasticity in patients who have suffered a stroke, intramuscular injection of botulinum toxin type A has been used. Local administration of the drug causes partial blockade of the neuromuscular synapse and muscle relaxation for 3-6 months, which provides opportunities for successful physiotherapy [4]. The use of botulinum toxin is recommended if spasticity of one muscle or group of muscles leads to impaired motor function, is accompanied by painful muscle spasms, or complicates patient care [4,5]. In patients who have suffered a stroke, a decrease in muscle tone and improvement in the motor functions of the limbs have been established after the injection of botulinum toxin into the posterior group of muscles of the leg of the paretic leg and the flexors of the forearm, hand and fingers [4,5].
5-10% of patients with post-stroke hemiparesis develop pain and swelling in the paretic arm or, less commonly, in the leg, which is usually caused by joint damage and/or peripheral vascular disorders [6]. If movements in the joints of a paretic limb are accompanied by pain, then active and passive movements in the joint are recommended, causing only minimal pain, gradually increasing their volume. To reduce pain before gymnastics, you can use local anesthetic ointments or compresses with novocaine and dimexide, massage and reflexology. For prolonged and severe pain, courses of non-steroidal analgesics are used, combining them with antidepressants in small doses (for example, amitriptyline 25-75 mg at night or 2-3 times a day) and/or anticonvulsants (for example, carbamazepine 200-600 mg /day or clonazepam 0.5-2 mg/day). To reduce swelling of a paretic limb, positional treatment (periodic elevation of the arm or leg) is recommended, and pneumatic gloves or socks are used.
Pain in paretic limbs after a stroke can also have a central origin due to damage to sensory conductors and centers of the brain, most often the visual thalamus. Central pain occurs in 1 case out of 15 thousand strokes and more often appears some time after the development of the disease [7]. They are usually constant, intensify with emotional stress, and are combined with an altered perception of sensitivity (dysesthesia) in the affected parts of the body. Relief from severe central pain is achieved by administering a solution of sodium thiopental in a dose of 75-300 mg [7]. Sometimes antidepressants (for example, 25-75 mg of amitriptyline at night), anticonvulsants (for example, clonazepam 0.5-2 mg per day) and reflexology are helpful.
If a patient has speech disorders (aphasia, dysarthria) after a stroke, speech therapy classes are recommended. The patient must hear the speech of other people, radio, television and be able to communicate with others. It is necessary to encourage the patient to speak independently, even with a severe degree of impairment. Reading aloud, writing, drawing and other activities that stimulate speech functions are of great importance. The effectiveness of restoration of speech functions is largely determined by the patient’s motivation and his active participation in the rehabilitation process, therefore positive comments from the doctor and people around the patient about his success in classes are of great importance [6].
Impaired cognitive functions, decreased memory and intelligence are observed in a significant proportion of patients after a stroke. Cerebrovascular diseases account for about 20% of all causes of dementia in old age [7]. In order to improve speech and cognitive functions in patients who have suffered a stroke, you can use drugs that increase metabolic processes and blood supply to the brain. Both one of the neurotropic drugs and a combination of several drugs are used, but a combination of two or more vasoactive drugs is not recommended. Treatment is often carried out in courses over one month, 2-4 times a year [1]. Cerebrolysin is recommended in large doses (20-50 ml/day), administered in 100-200 ml of physiological solution intravenously (over 60-90 minutes) for 10-15 days.
Piracetam is used orally at 1.2-4.8 g/day. Gammalon is used 20 ml of a 5% solution per 300 ml of physiological solution intravenously for 10-15 days. Gliatilin is prescribed orally at 0.8-2.4 g/day. Nimodipine is prescribed orally at a dose of 30-60 mg 3-4 times a day. Vinpocetine is administered orally at a dose of 5 mg 3 times a day. Nicergoline is used orally at a dose of 5 mg 3-4 times a day. Cinnarizine is prescribed orally at a dose of 25 mg 3-4 times a day. Instenon is used 2-4 ml intravenously (over 3 hours) for 3-5 days. Nicardipine is used orally at a dose of 20 mg 2 times a day.
Depression occurs in more than half of patients after a stroke [6]. It significantly complicates the process of rehabilitation of the patient, complicates his care and his contact with other people. Depression can manifest itself as headaches and other neurological disorders, which are sometimes mistakenly regarded as the progression of vascular damage to the brain in a patient who has suffered a stroke. To treat depressive syndrome, psychotherapy and (or) antidepressants are used, for example, amitriptyline 25-75 mg/day at night or 2-3 times a day, tianeptine 25-37.5 mg/day or fluoxetine 20 mg once a day. day. It is advisable to tell the patient that many people who suffered a stroke were able to gradually restore lost abilities, everyday skills, and even return to their previous professional activities.
The development of epileptic seizures is more often observed after lobar intracerebral hemorrhage, subarachnoid hemorrhage or cortical ischemic stroke [2]. In these cases, anticonvulsants are prescribed, as for other causes of epileptic seizures [1,2,8]. It is recommended to start treatment with carbamazepine 600 mg/day or phenytoin 300 mg/day [2].
One of the important areas of treatment for patients who have suffered a stroke is the prevention of recurrent stroke, the risk of which is 10-16% during the first year, which is 15 times higher than in the general population of the same sex and age [8]. After one year, the risk of another stroke drops to 5% per year for the next four years. The risk of recurrent stroke is increased in the presence of arterial hypertension, arrhythmia, heart valve pathology, congestive heart failure, and diabetes mellitus.
Prevention of recurrent stroke should begin as soon as possible and continue for at least 4 years [8]. It is based on elucidating the etiology and pathogenesis of primary stroke and is aimed at correctable risk factors for its development. If a specific cause of ischemic stroke (eg, infective endocarditis) or hemorrhagic stroke (eg, saccular aneurysm) is determined, then appropriate treatment is given. Maintaining a healthy lifestyle is important, which includes quitting smoking or reducing the number of cigarettes you smoke, avoiding drug use and alcohol abuse, adequate physical activity, and losing excess weight. It is advisable to reduce the consumption of foods containing large amounts of cholesterol (butter, eggs, fatty cottage cheese, etc.) and increase the amount of fresh vegetables and fruits in the diet. Women who have had a stroke are not recommended to use oral contraceptives. It is important to prevent the development of situations that provoke a recurrent stroke: hypoxia and low blood pressure during surgical operations; a sharp decrease in blood pressure during antihypertensive therapy; taking large doses of tranquilizers and neuroleptics, causing severe sedation and deep sleep; systemic arterial hypotension, anemia, thrombocythemia; rapid forced diuresis [3].
Arterial hypertension is the most important correctable risk factor for stroke. Antihypertensive drugs reduce the risk of developing a first stroke by an average of 38% one year after starting regular therapy [9].
The effectiveness of antihypertensive therapy in secondary stroke prevention is less studied [9]. In the first days of ischemic stroke, antihypertensive therapy is not recommended, which is associated with the risk of reducing perfusion pressure in the brain tissue and increasing the size of the ischemic focus [3,6,8]. The exceptions are cases of high blood pressure (200/120 mm Hg and above), combined myocardial infarction, and pulmonary edema. In case of intracerebral hemorrhage, antihypertensive therapy is recommended already in the first days of the development of the disease, but blood pressure should not be sharply reduced due to the risk of ischemic complications [2,8]. One to two weeks after the onset of stroke, autoregulation of cerebral circulation, impaired due to stroke, is expected to normalize; therefore, if elevated blood pressure persists, long-term antihypertensive therapy is necessary for the purpose of secondary prevention of stroke [8].
Patients who have had a stroke and have arterial hypertension may be advised to reduce their dietary salt intake, as this can lower blood pressure and therefore reduce the dose of antihypertensive drugs, which can cause unwanted side effects. If the patient is overweight, then it is recommended to achieve and maintain ideal body weight, which requires reducing the total calorie content of food and regular physical activity (therapeutic exercises, walking), the intensity of which is individual.
In patients who have suffered a stroke, antihypertensive therapy should be carried out with caution to avoid a significant decrease in blood pressure and cerebral hypoperfusion, especially in elderly patients with occlusive lesions of the cerebral and precerebral arteries. Before using antihypertensive drugs, it is advisable to examine the precerebral and cerebral arteries using duplex scanning and transcranial Doppler sonography in order to establish the presence and extent of an occlusive lesion and, based on this, assess the risk of cerebral complications of antihypertensive therapy. Repeated studies of cerebral hemodynamics while taking antihypertensive drugs make it possible to determine the optimal level of blood pressure reduction, which in patients who have had a stroke with prolonged arterial hypertension can be significantly higher than the usual normal blood pressure values. However, in general, antihypertensive therapy is recommended even for elderly patients if their blood pressure increases 1-2 weeks after an ischemic and especially hemorrhagic stroke [8]. As antihypertensive therapy, beta-blockers (nebivolol, atenolol, metoprolol, labetalol, etc.), angiotensin-converting enzyme inhibitors (captopril, perindopril, enalapril, etc.), calcium channel blockers (amlodipine, verapamil, etc.) and other antihypertensive drugs can be used. means taking into account individual indications and contraindications for their use. Perindopril has been shown to be safe when taken long-term for secondary prevention of stroke [10].
To prevent a recurrent stroke, patients who have suffered an ischemic stroke are recommended to take antiplatelet agents for 1-2 years or continuously: acetylsalicylic acid, dipyridamole, ticlopidine or clopidogrel. Acetylsalicylic acid is usually used in small doses (80-300 mg/day), which is considered preferable due to the lower risk of complications from the gastrointestinal tract and the lack of inhibition of vascular wall prostacyclins, which have an antithrombotic effect. To reduce the irritating effect of the drug on the stomach, a form of acetylsalicylic acid that does not dissolve in the stomach is used.
Ticlopidine is prescribed 250 mg 2 times under the control of a complete blood count (every 2 weeks during the first 3 months of treatment) due to the risk of leukopenia. Clopidogrel is used at 75 mg/day and has fewer side effects than acetylsalicylic acid and ticlopidine.
In patients with atrial fibrillation, intraventricular thrombus, artificial heart valve and other pathologies dangerous for the recurrence of cardiac embolism, the use of indirect anticoagulants (warfarin 5 mg/day, phenylin 60-90 mg/day) is more effective than antiplatelet agents, but this requires regular monitoring of prothrombin (increasing the international normalizing coefficient to 3.0-4.0 or reducing the prothrombin index to 50-60%), which is often difficult.
If a patient who has suffered an ischemic stroke has hyperlipidemia (increased levels of total cholesterol more than 6.5 mmol/l, triglycerides more than 2 mmol/l and phospholipids more than 3 mmol/l, decreased levels of high-density lipoproteins less than 0.9 mmol/l) , a low-cholesterol diet is recommended to prevent the progression of atherosclerosis. If diet cannot significantly reduce hyperlipidemia, then it is recommended to take lipid-lowering drugs (lovastatin, simvastatin, pravastatin, etc.) in the absence of contraindications to their use.
Carotid endarterectomy is considered when identifying internal carotid artery stenosis to prevent recurrent stroke. Currently, carotid endarterectomy is recommended for severe (narrowing 70-99% of the diameter) stenosis of the internal carotid artery in patients who have suffered a transient ischemic attack or minor stroke. It can also be performed in cases of moderate degree (narrowing of 30-69% of diameter) stenosis of the internal carotid artery in patients with minor stroke, as well as in cases of severe or moderate degree of stenosis in patients with mild or moderate neurological deficit after a stroke, but the effectiveness of surgical treatment in these cases it is debatable [3,6,8]. When choosing surgical or conservative tactics for managing a patient who has suffered a stroke and has stenosis of the internal carotid artery, one should take into account damage to other carotid and cerebral arteries, the severity of coronary artery pathology and the presence of other somatic diseases [3].
Patients who have had a stroke have twice the risk of death than the general population of the same age. This is caused not only by the high probability of a recurrent fatal stroke, but also by the risk of somatic diseases (myocardial infarction, pneumonia, kidney disease, etc.) that occur in patients after a stroke due to the presence of arterial hypertension, pathology of the coronary arteries, and heart rhythm disturbances. , diabetes mellitus. The development of somatic diseases more often leads to the death of the patient than a recurrent stroke, so their prevention and treatment is no less important in the management of patients who have suffered a stroke [6,8]. Treatment of somatic diseases can significantly improve the quality of life of patients and reduce the risk of various diseases of the cardiovascular system.
Vinpocetine –
Vinpocetine-Acree (trade name)
(Akrikhin)
Literature:
1. Vilensky B.S. Stroke: prevention, diagnosis and treatment. St. Petersburg, 1999 -336 p.
2. Gusev E.I., Gekht A.B., Gaptov V.B., Tikhopoy E.V. Rehabilitation in neurology. M., 2000-52.
3. Adams RM, Victor M, Ropper AH Principles of Neurology. New York. 1997, 777-873.
4. Dressier D. Botulinum Toxin Therapy. NY, 2000 - 192.
5. Simpson DM Muscle & Nerve 1997 Suppl.6:169-176.
6. Vibers D.O., Feigin V.L. Brown R.D. Guide to Cerebrovascular Diseases. Per. from English M., 1999 - 672 p.
7. Diseases of the nervous system. Guide for doctors // Ed. Yakhno N.N., Shtulman D.R., Melnichuk P.V.. M., 1995, vol. I - 656 p.
8. Warlow C.P., Dennis M.S., J. van Geyn Stroke. Practical guide for the management of patients. Per. from English St. Petersburg, 1998 - 629 p.
9. Mac Mahon S, Rodgers A. Hypertens Res 1994, 17 (Suppi I): 23-32.
10. Chalmers J, MacMahon S, Anderson C et al. Clinician's manual on blood pressure and stroke prevention. Second ed. - London, 2000. - 129
Recovery period
The rehabilitation period is aimed at restoring lost functions and improving the quality of life of patients who have suffered a stroke. The doctor develops a rehabilitation program individually for each patient, taking into account the scale of the vascular accident, age, comorbid pathology, etc.
In case of strokes, doctors assign a special role to the prevention of recurrent strokes, which includes proper nutrition, giving up bad habits, eliminating excess weight, and regular monitoring by a doctor.
Is full recovery possible after a stroke?
The patient’s relatives play a significant role in the rehabilitation of a patient after a stroke. It depends on their attention, care, patience and correct actions whether the patient’s lost functions can return.
The recovery process after a stroke is a difficult period, both for the patient himself and for his loved ones. The rehabilitation time depends, first of all, on the degree of damage to brain tissue. Patients may have impaired coordination of movements, mobility of limbs, speech, memory, hearing, and vision.
The patient’s persistence and positive attitude can speed up the recovery time of lost functions.
An experienced team of doctors will speed up the rehabilitation process thanks to a well-designed individual treatment program.
Levels of recovery after stroke
After hemorrhagic and ischemic strokes, there are three levels of recovery:
- the first is the highest. We are talking about the complete restoration of lost functions to their original state. This option is possible in the absence of complete death of nerve cells in a region of the brain;
- the second level is compensation. The early stage of recovery, usually in the first six months after a stroke. Lost functions are compensated by the involvement of new structures and functional restructuring.
- The third level involves readaptation, that is, adaptation to the emerging defect. The patient’s relatives and friends play a significant role in this process. They are the ones who help the patient learn to live with the emerging defect.
Specialists at the Yusupov Hospital, if necessary, work with the patient’s relatives, teaching them the specifics of care, as well as providing them with psychological support.
Prognosis for recovery after stroke
Favorable factors for recovery after a stroke include:
- timely early start of rehabilitation therapy;
- spontaneous early recovery of lost functions.
Among the unfavorable factors of recovery after a stroke are:
- advanced age of the patient;
- large area of brain tissue damage;
- poor blood circulation around the affected brain tissue;
- damage to cells in functionally important areas of the brain.
Basics of Stroke Recovery
In the process of rehabilitation, the positive attitude of the patient himself and his desire to return to independent life are important. Psychological support and assistance from the patient’s relatives plays a huge role. You can make an appointment with a neurologist by phone.
Memory recovery after stroke
Treatment of patients after a stroke takes place in the neurological department. Memory restoration depends on many factors: the size of the area of brain damage, the location of the damage, and the timeliness of medical care. The faster blood circulation in the brain is restored, the greater the chance of memory recovery after a stroke.
Memory restoration after a stroke is possible with the participation of several specialists - a neurophysiologist, psychologist, neuropsychologist, neuropsychiatrist. Help for a patient after a stroke is provided at the rehabilitation clinic of the Yusupov Hospital. In the hospital, the patient is treated according to an individual recovery program; many specialists take part in the development of such a program. When developing the program, the patient’s health condition, the severity of brain damage, and memory impairment are taken into account.
In some cases, it takes several years to restore memory and speech; during recovery, the doctor prescribes medication, a special diet, various trainings - color therapy, rhythm therapy, music therapy and others. Memory restoration at home is not always successful due to the lack of a training program and knowledge in the field of rehabilitation of patients after a stroke.
You can make an appointment with a neurologist at the Yusupov Hospital by phone. Consultation with a specialist, full patient care, rehabilitation using innovative equipment, massages and exercises will help the patient regain full memory.
Restoring a hand after a stroke
A positive attitude and support from family have an impact on rapid recovery from illness. Partial paralysis of the arm is a common occurrence after a stroke and is characterized by stiffness of movement and limited motor ability of the arm. Functional paresis (partial paralysis) refers to neurological syndromes, caused by disruption of the nervous system, damage to the nervous system pathway due to damage to the cerebral cortex after a stroke. Paralysis of the arm is the complete absence of voluntary movements of the limb.
Recovery from a stroke may involve the hand or the entire limb. With partial paralysis, the ability to move the arm or hand freely is impaired; the person cannot fully care for himself or perform basic actions. To restore motor ability, the patient must perform daily exercises for finger motor skills and limb motor skills.
The rehabilitation process of restoring motor activity of the limbs requires patience from the patient and a lot of work - this will allow you to return to a full life after a stroke. You can make an appointment with a neurologist by phone. The rehabilitation doctor will develop individual exercises for the patient, the patient will be under constant medical supervision and receive qualified assistance from specialists.
Swelling of the hands
Swelling in the hands can occur in people of any age, from the young to the very old. They often appear due to minor disorders in the body and go away on their own, but sometimes they can be signs of serious diseases. You should be especially wary if the swelling of the hands is asymmetrical: it occurs only on one hand or is much more pronounced on one hand than on the other.
Causes of swelling of the hands and distinctive features of pathologies accompanied by swelling of the hands
Swelling of the hands can appear with superior vena cava syndrome (compression of this large vessel). With this syndrome, swelling may occur in the face, neck, upper torso and arms. The skin of these sections is bluish; the bluishness intensifies even more when the body bends forward. There may also be dilatation of the superficial veins of the neck, torso, and arms. Some patients develop “spider veins” on their chest and back as a result of dilated capillaries. Due to increased blood pressure in the venous system, some patients may complain of bleeding from the nose, throat (esophagus), and headaches. decreased vision, rushes of blood to the head when bending, auditory hallucinations. Swelling of the vocal cords may develop, accompanied by hoarseness.
Neurological diseases can cause swelling in the hands. In patients who have suffered a stroke complicated by paralysis of the upper limbs, capillary permeability increases. In this case, moderate swelling of the paralyzed limbs appears, the nutrition of the skin is quickly disrupted, it becomes thinner, and purulent infections can occur. The same swelling can occur in patients with syringomyelia and polio.
Unilateral swelling of the arms can also occur due to acute thrombosis of the subclavian vein. This pathology may be preceded by a long period of chronic venous insufficiency. It manifests itself as increased fatigue, cyanosis of the hand, and a feeling of heaviness in the hand after physical activity. As a rule, this disease occurs in young men involved in sports and physical labor. Strong physical activity provokes the development of acute thrombosis. And thrombosis itself can be suspected by the rapidly occurring dense swelling of the arm from the shoulder to the hand. Patients feel a feeling of fullness, heaviness and burning in the affected limb. The arm is cyanotic, its circumference is much larger than that of a healthy one. When pressing with a finger on the area of edema, the hole does not remain. Over time, the swelling may subside, and the disease becomes chronic. However, periodically physical activity can provoke exacerbations of the disease and a return of symptoms.
In older people, the most common cause of unilateral swelling of the arms may be compression of the subclavian vein by a tumor. Compared to acute thrombosis of the subclavian vein, the swelling is less pronounced, increases gradually, and, as a rule, there is no pain in the affected arm. Simultaneously with compression of the subclavian vein by the tumor process, compression of the innominate vein may also occur. This is manifested by swelling and cyanosis of half the face and neck.
The cause of swelling of the hands may be inflammatory damage to the lymphatic vessels (lymphangitis). As a rule, it is a complication of a purulent-inflammatory disease of the hand. This pathology is manifested by general symptoms in the form of fever, malaise and local swelling of the arm, redness, and local increase in body temperature. Along the course of the lymphatic vessels, painful compaction-strands are felt. With lymphangitis, there is always regional enlargement of the lymph nodes.
Swelling of the arm in women may occur after breast removal. The main reason for this is impaired lymphatic drainage.
Middle-aged women may experience causeless swelling of the arms and legs. They are more pronounced in hot weather. On the hands and eyelids, such swelling occurs in the morning, and on the legs it is more pronounced in the evening. At the same time, all analyzes and results of instrumental research methods will remain within normal limits.
Taking certain medications - estrogens, mineralocorticoids, vasodilators - can provoke the appearance of hand swelling.
Sometimes swelling in the arms can occur along with swelling in the legs during pregnancy and premenstrual syndrome.
Swelling of the hands can be combined with swelling of the legs, face, and torso and occur as a result of cardiovascular, endocrine, and renal pathologies.
Treatment of hand swelling
You can independently reduce the severity of swelling of both hands with the help of diuretics (for example, veroshpiron). Diuretics such as Lasix and furosemide should not be used (especially for a long time), as they promote the removal of potassium from the body, and this can negatively affect the functioning of the cardiovascular system.
You can also resort to the help of folk diuretics - drinking watermelon pulp, green tea, burdock root decoction, infusion of cornflower flowers, decoction of lingonberry leaves. If possible, it is necessary to limit fluid intake so that it does not accumulate in the tissues of the hands.
If you have swelling on one arm, then you should not self-medicate. It is necessary to immediately consult a doctor to determine the cause of this disorder and select treatment.
Comments 1
From May 22 to June 3, Dr. Komarovsky will be in Finland!
SDK: Viral croup.
Meeting with a pediatric neurosurgeon - cephalohematoma. Choosing slings and carriers for children. Preparing “orange” cauliflower.
Factors influencing the speed and quality of rehabilitation
There are many factors that influence the speed of recovery after a stroke, so predicting the duration of rehabilitation and likely results is quite difficult.
How long rehabilitation after a stroke will last depends on the individual parameters for each person, as well as on other factors:
- volume of damage: an extensive stroke significantly worsens the severity of the patient’s condition, and also causes many neurological complications that adversely affect the timing of recovery and its quality;
- patient’s age: the older the victim, the longer the recovery;
- localization of damage: circulatory disorders of deep structures are difficult to treat;
- type of stroke: hemorrhagic strokes are less common, but occur in a more aggressive form, and also have a high mortality rate, although the prognosis for rehabilitation is more favorable than for ischemic stroke;
- caused by disorders: the presence of multiple cerebral symptoms, comatose states, severe paralysis and sensory disturbances give an unfavorable prognosis for recovery;
- timeliness of therapy: the most positive results of therapy can be achieved by starting treatment measures in the first 4 hours after the onset of the first symptoms; seeking help at a later time worsens the prognosis;
- compliance with medical recommendations: after the patient is discharged from the medical institution, the patient is given recommendations that can improve the quality of life, prevent the formation of relapse and negative complications.
The severity of the lesion has the greatest impact on the likelihood of restoration of lost functions and the timing of rehabilitation. With extensive strokes, violations of the most important functions are observed, even if the prescribed rehabilitation program is followed, the prognosis is rather disappointing. The greatest difficulties arise with the complete return of speech and motor functions. Close relatives who will devote a lot of time to special activities with the patient can positively influence the situation.
Symptoms of hemorrhagic stroke
With hemorrhoidal stroke, symptoms most often appear suddenly, mainly during the daytime and during very heavy physical activity. The following symptoms are typical:
- convulsions;
- Strong headache;
- sudden loss of consciousness;
- nausea and vomiting;
- serious depression of a person's consciousness, similar to or leading to a coma
In addition, general symptoms of a stroke appear:
- decreased facial expressions and muscle strength affecting any part of the body;
- the occurrence of speech disorders and problems with visual perception;
- loss of coordination of movement with impaired ability to move.
During an attack, the patient's skin becomes cold and sometimes acquires a purplish-bluish tint. Breathing becomes more frequent, noisy, with wheezing. Sometimes, on the affected side, the pupil dilates, diverges, or chaotic movements of the eyeballs occur.
An important indicator of the severity of the patient’s current condition is comatose status with loss of consciousness, which can last several days. This makes the prognosis very unfavorable.
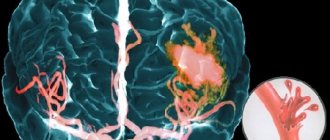
Subarachnoid hemorrhage most often results from rupture of a cerebral aneurysm. As a result, the patient experiences severe headaches localized in the back of the head and forehead. Then it spreads to the rest of the head. Later, other symptoms of hemorrhagic stroke appear.
In case of extensive cerebral hemorrhage, neurosurgical microtechnical operations are performed. In this case, removal of the hematoma leads to a decrease in pressure on the brain tissue and prevents the development of brain edema. But surgery is performed strictly for medical reasons.
In case of an aneurysm, surgery is performed to stop bleeding, and the patient is prescribed hemostatic drugs. Often with subarachnoid lesions, narrowing of the vessel occurs and the development of ischemic stroke. In this case, calcium channel blockers are necessarily prescribed to prevent narrowing and spasm of the vascular walls.
In the first 3 weeks after the attack, the patient’s condition remains the most severe due to progressive cerebral edema, as well as a gradual increase in cerebral symptoms. If there are any chronic pathologies in the body, aggravated by a hemorrhagic stroke, the patient may die. A month later, the patient begins to experience regression of cerebral symptoms and blood pressure stabilizes.
This is interesting! It is recommended to always have glycine in your home medicine cabinet. Many qualified doctors classify this drug as a neuroprotector or a substance that protects brain tissue.
If unpleasant weakness in the limbs or speech disorder occurs, you should immediately put 5 glycine tablets under your tongue. To some extent, such prevention can prevent acute brain damage and the development of hemorrhagic lesions.
Many people are interested in the difference between ischemic and hemorrhagic stroke. Two such lesions have almost identical symptoms, but have different reasons for the development of such a serious pathology. With ischemic stroke, the prognosis is favorable and mainly depends on the degree of brain damage that has occurred.
The following symptoms are characteristic of each type of this disease:
- suppression of speech ability;
- partial or complete paralysis of the body and limbs;
- impairment of visual sensitivity or its complete loss;
- impaired coordination of movements;
- complete loss of hearing in a hemorrhagic condition;
- • serious inhibition of the functions of the cerebral cortex;
- • increased blood pressure.
The consequences of a stroke mainly depend on the location and extent of the existing lesion. A hemorrhagic attack has an acute onset and progresses rapidly. The onset of coma in this case is possible within the first few minutes or hours. With ischemic stroke, the symptoms are less severe.
Damage to the left hemisphere leads to paralysis of the right side of the body. Hemorrhage in the cerebellar area deprives the patient of sensitivity, the ability to swallow, see and speak. Often the consequence of a hemorrhagic stroke is the gradual development of dementia or dementia.
Stroke Prevention
Prevention of heart attack and stroke in women and men are links in one chain of measures that prevent disability and death in people suffering from cardiovascular diseases.
Cardiologists and neurologists at the Yusupov Hospital use modern diagnostic methods to examine patients, allowing them to identify risk factors for vascular diseases and take measures aimed at preventing diseases. Medicines for the prevention of stroke and heart attack allow you to control the course of the disease, reduce the incidence of acute cardiovascular crises, and the likelihood of complications.
Chance of full recovery after stroke
The rehabilitation period is individual; for some, a few months are enough; for others, it will take years to achieve a positive result. The earlier restoration procedures are started, the more favorable the prognosis. At the same time, the patient’s attitude and focus on results is important; The greater a person’s desire to return to a full life, the more effective the classes and exercises.
At the Yusupov Hospital, a well-coordinated team of professionals (neurologists, rehabilitation specialists, therapists, cardiologists, speech therapists, psychologists) takes part in the rehabilitation of patients after a stroke. Doctors create an individual program for each patient, aimed at the best possible result, observing the following principles:
- early start of restorative procedures;
- systematicity and duration of events;
- complexity of procedures;
- multidisciplinarity of classes;
- compliance of procedures with the patient’s condition;
- active interaction between doctors and the patient and his family.
You can make an appointment with the doctors at the Yusupov Hospital and find out how much rehabilitation after a stroke costs by calling.
Causes of stroke
A stroke can be caused by several reasons. The most important risk factors for this condition are smoking, a sedentary lifestyle, alcohol abuse, obesity, and genetic predisposition (cases of strokes in close relatives can be considered an indirect sign). The cause may vary depending on the type of stroke. The two most common types are described below:
A hemorrhagic stroke occurs due to internal bleeding when a blood vessel inside the brain ruptures. Other names for hemorrhagic stroke are cerebral hemorrhage or intracranial hemorrhage. Among the causes of hemorrhagic stroke are:
- inactive lifestyle;
- increased stress levels;
- alcohol abuse;
- obesity;
- smoking.
Hemorrhagic stroke can also be caused by abnormal formation of blood vessels or rupture of dilated vessels (a complication of cerebral venous insufficiency).
Ischemic stroke occurs due to circulatory problems. A typical case is a blood clot blocking the lumen of a vessel. The cause of ischemic stroke can be:
- diabetes;
- excessive alcohol consumption;
- obesity;
- high cholesterol (causing cerebral atherosclerosis);
- smoking;
- arterial hypertension.
Atrial fibrillation, a type of irregular heartbeat, is another cause of ischemic stroke.