Periphlebitis: what is it and what are the causes of the disease?
Periphlebitis (Latin periphlebitis) is an inflammatory process that affects the tissue surrounding the vein. The disease develops when inflammation moves from the soft tissues to the external venous walls.
!
A feature of periphlebitis is that all layers of the vessel are affected.
The first to be affected is the perivascular connective tissue, which is the mechanical support of the vessel. The pathological process causes destruction of tissue fibers. In rare cases there is no external manifestation. But, as a rule, such a process leads to a sharp local reaction in which a compaction can form - an inflammatory infiltrate. Infiltrate is an accumulation of elements of cells, blood or lymph. From this moment, the next structural component of the vascular wall begins to deteriorate - the muscle layer. When the membrane formed by muscle fibers is damaged, inflammation reaches the endothelial cells (the inner layer of the vessel).
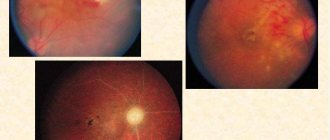
In what cases and who can develop periphlebitis? The inflammatory process can involve perivenous tissues and vessels on the arm or leg. And it can affect the fundus of the eye, causing vascular changes and multiple foci of inflammation of the veins of the retina (Eales disease). In infancy, inflammation of the skin and subcutaneous tissue in the navel area is also possible. Periphlebitis not only has a wide area of distribution of the lesion, but at the same time it is polyetiological. This means that the disease can occur for various reasons. In particular, among them:
- pronounced chemical effects on blood vessels, harmful substances or pharmaceuticals;
- allergic reactions (for example, from insect bites);
- infection and mechanical injury to the vascular wall (for example, after an IV catheter or injection with a blunt needle);
- failure to comply with hygiene rules when treating the umbilical wound of a newborn;
- burn disease;
- artificial termination of pregnancy and postpartum complications;
- slowing down the speed of blood flow.
Allergy from insect bites is a symptom of periphlebitis.
Post-injection periphlebitis is a common complication faced by hospital patients. In most cases, it affects the upper extremities, since injections are most often performed into the veins in the bend of the elbow.
Expert opinion
To avoid the development of periphlebitis as a result of termination of pregnancy, abortion must be performed exclusively in medical institutions designated for this purpose, and manipulations should be carried out only by experienced obstetricians. Remember: criminal abortion can lead to dangerous consequences for health and life!
Vascular surgeon, phlebologist
Osipova Ekaterina Yakovlevna
The reason why foci of inflammatory processes may appear may lie in the course of diseases such as:
- varicose veins and other vascular pathologies;
- increased thrombus formation;
- atherosclerosis (Atherosclerosis);
- diabetes mellitus (Diabetes mellitus);
- oncology, etc.
In addition, any painful condition caused by pathogenic flora can become a provoking factor for the development of periphlebitis:
- otitis (external, internal and middle ear);
- erysipelas;
- acute tonsillitis (Tonsillitis);
- rheumatism of the joints;
- tuberculosis of the lungs;
- osteomyelitis (Osteomyelitis);
- pneumonia (Pneumonia);
- typhus;
- syphilis (Syphilis);
- adnexitis (Adnexitis);
- tracheitis, etc.
Based on the above, it becomes obvious that periphlebitis of the upper and lower extremities and retinal veins is a consequence of current diseases. Therefore, the very fact of the development of periphlebitis means the lack of necessary treatment, its untimeliness or failure, including those related to the quality of medical services.
In this regard, to prevent periphlebitis from becoming a concomitant disease, it is necessary to do everything in our power. Having taken the situation into our own hands, we must be attentive to our own health and the health of our child. And then we will have a fairly good chance of avoiding various diseases, especially their complications.
In this article we will look at superficial periphlebitis of the lower extremities, its symptoms and possible treatment. The first thing you need to start with is the signs of periphlebitis. After all, in order to detect and prevent the acute course of the disease, it is important to know what symptoms are inherent in it.
Symptoms of periphlebitis of veins
Diagnosis and treatment of superficial (saphenous) vein thrombosis
Thrombosis of the superficial (subcutaneous) veins in clinical practice is referred to as “thrombophlebitis”. In the vast majority of cases, thrombophlebitis is a complication of chronic venous diseases that occur with varicose transformation of the saphenous veins (varicothrombophlebitis). Clinical signs: • pain along the thrombosed veins, limiting limb movements; • a stripe of hyperemia in the projection of the affected vein; • on palpation - a cord-like, dense, sharply painful cord; • local increase in temperature, hyperesthesia of the skin. When examining a patient with suspected thrombophlebitis, it is necessary to examine both lower extremities, since bilateral combined damage to both superficial and deep veins is possible. In addition to identifying symptoms of thrombophlebitis in patients suspected of having this disease, it is necessary to specifically determine the presence of symptoms indicating PE. The value of a physical examination for accurately establishing the extent of thrombosis is low due to the fact that the true prevalence of saphenous vein thrombosis is often 15-20 cm higher than clinically detectable signs of thrombophlebitis. In a significant proportion of patients, the transition of the thrombotic process to the deep venous lines is asymptomatic. The main diagnostic method is compression ultrasound duplex angioscanning. The standard scope of ultrasound angioscanning must necessarily include examination of the superficial and deep veins of not only the affected, but also the contralateral limb to exclude simultaneous thrombosis, which is often asymptomatic. The deep veins of both lower extremities are examined along their entire length, starting from the distal parts of the leg to the level of the inguinal ligament, and if intestinal gas does not interfere, then the vessels of the iliocaval segment are examined.
Indications for hospitalization: localization of acute thrombophlebitis on the thigh; — localization of acute thrombophlebitis in the upper third of the leg with damage to the small saphenous vein. Such patients should be hospitalized in vascular surgery departments. If this is not possible, hospitalization in a general surgical hospital is acceptable. Therapeutic tactics For thrombosis of superficial veins against the background of varicose veins, a more active surgical tactic seems appropriate.
Conservative treatment should include the following main components: 1) active regimen; 2) elastic compression of the lower extremities; 3) local therapeutic effect on the affected limb (cold, drugs containing heparin and/or NSAIDs).
4) systemic pharmacotherapy.
In case of spontaneous thrombosis of the superficial veins of the lower extremities, subcutaneous administration of fondaparinux sodium or prophylactic (or possibly intermediate) 1 dose of LMWH is advisable for at least 1.5 months. New oral anticoagulants (NOACs) (apixaban, dabigatran etexilate, rivaroxaban) should not be used for the treatment of saphenous vein thrombosis due to the current lack of data confirming their effectiveness and safety in this pathology. In addition to anticoagulants, in case of severe pain, it is possible to use non-steroidal anti-inflammatory drugs (NSAIDs) orally for 7-10 days. It should be taken into account that their combination with anticoagulants increases the likelihood of hemorrhagic complications. Intermediate doses include LMWH doses that are 50-75% of the therapeutic dose. It is not advisable to use antibacterial drugs in the complex treatment of superficial vein thrombophlebitis in the absence of signs of a systemic inflammatory reaction. Surgical treatment: 1. Crossectomy (Troyanov-Trendelenburg operation). High (immediately at the deep main) ligation of the large (or small) saphenous vein with mandatory ligation of all estuarine tributaries and excision of the trunk of the saphenous vein within the surgical wound. Indicated when thrombophlebitis spreads to the upper half of the thigh or estuarine tributaries when v. is affected. saphena magna and the upper third of the leg when affected v. saphena parva. The operation is feasible in any category of patients. 2. Thrombectomy from the main deep veins. Performed when thrombosis spreads beyond the sapheno-femoral or sapheno-popliteal ostium. The choice of access and thrombectomy method is determined by the level of location of the proximal part of the thrombus. After the anastomosis is released, a crossectomy is performed. 4. Miniphlebectomy in the pool v. saphena magna and/or v. saphena parva. Provides for the removal of all varicose veins (thrombosed and non-thrombosed) after crossectomy. It can be performed in uncomplicated patients in the first 2 weeks of the disease. At a later date, a dense inflammatory infiltrate in the area of varicothrombosis-lebitis prevents atraumatic removal of the affected veins.
5. Puncture thrombectomy from thrombosed nodes of the saphenous veins. Performed against the background of severe periphlebitis. Removal of blood clots from the affected veins under conditions of adequate postoperative elastic compression leads to a rapid reduction in pain and aseptic inflammation. Surgical treatment must be combined with the appropriate use of anticoagulants. Diagnosis and treatment of post-injection thrombosis of the saphenous veins of the upper extremities Clinical manifestations are similar to those of thrombosis of the saphenous veins of the lower extremities: - pain along the thrombosed veins; - a stripe of hyperemia in the projection of the affected vein; - on palpation - a cord-like, dense, sharply painful cord; - local increase in temperature. No special diagnostic methods are required.
Therapeutic tactics - only conservative treatment: - local therapeutic effect on the affected limb (cold, drugs containing heparin and/or NSAIDs); - in case of severe pain, it is possible to use NSAIDs orally for 7-10 days; — the use of anticoagulants is advisable only when the thrombotic process progresses and there is a threat of its spread to the subclavian vein. Diagnosis of DVT The formation of a blood clot can begin in any part of the venous system, but most often in the deep veins of the leg. There are occlusive and non-occlusive thrombus. Among non-occlusive thrombi, floating thrombi, which can cause pulmonary embolism, are of greatest practical interest. The degree of embolism of venous thrombosis is determined by the characteristics of the clinical situation. The decision about the degree of potential threat to the patient’s life is made by the attending physician based on a comprehensive assessment of the patient’s somatic status, characteristics of the thrombotic process and ultrasound angioscanning data. In this case, one should take into account the time of occurrence and localization of the thrombus, its nature (mobility in the lumen of the vein), the volume of the moving part and the diameter of the base. Embolic-dangerous thrombi are located in the femoral, iliac and inferior vena cava, the length of their moving part is usually at least 7 cm. However, in patients with low cardiopulmonary reserve due to concomitant pathology or previous pulmonary embolism, there is a real threat of life-threatening embolism. pain may represent floating thrombi of smaller sizes. Clinical manifestations depend on the localization of thrombosis, the prevalence and nature of damage to the venous bed, as well as the duration of the disease. In the initial period, with non-occlusive forms, clinical symptoms are not expressed or are completely absent. Sometimes the first sign of DVT may be symptoms of pulmonary embolism. A typical range of symptoms includes: • swelling of the entire limb or part of it; • cyanosis of the skin and increased pattern of subcutaneous veins; • bursting pain in the limb; • pain along the neurovascular bundle. For clinical diagnosis, the Wells index (Table 4) can be used, reflecting the likelihood that the patient has DVT of the lower extremities. Based on the sum of points scored, patients are divided into groups with low, medium and high probability of having venous thrombosis. Deep vein thrombosis in the superior vena cava system is characterized by: • edema of the upper limb; • swelling of the face, neck; • cyanosis of the skin and increased pattern of the saphenous veins; • bursting pain in the limb. Since clinical data do not allow us to judge with certainty the presence or absence of DVT, the diagnostic search should include subsequent laboratory and instrumental examination. Laboratory diagnostics Determination of the level of D-dimer in the blood. An increased level of D-dimer in the blood indicates actively occurring thrombus formation processes, but does not allow one to judge the location of the thrombus. The highest sensitivity (more than 95%) is provided by quantitative methods based on enzyme-linked immunosorbent assay (ELISA) or immunofluorescent assay (ELFA). After the development of thrombosis, the D-dimer gradually decreases and after 1-2 weeks can return to normal. Along with high sensitivity, the test has low specificity. Elevated levels of D-dimer are detected in many conditions, including tumors, inflammation, infection, necrosis, after surgery, during pregnancy, as well as in the elderly and patients in hospital. The upper limit of normal for D-dimer, determined by enzyme-linked immunosorbent methods, in persons under 50 years of age is 500 μg/l; in older age groups it is recommended to calculate it using the formula: age × 10 µg/l.
In connection with the described features, the following algorithm for using the D-dimer indicator for diagnosing DVT is proposed:
- patients without any clinical signs suggesting the presence of DVT should not have their D-dimer level determined for screening purposes; — patients with clinical symptoms and anamnesis that leave no doubt about the presence of DVT should not have their D-dimer level determined; — patients with clinical signs that suggest DVT, if it is not possible to perform compression ultrasound angioscanning in the next few hours, should determine the D-dimer level.
An increase in the indicator indicates the need for an ultrasound examination. If the medical institution does not have ultrasound equipment, the patient should be referred to another clinic with appropriate capabilities. In cases where the level of D-dimer in the blood is not elevated, the diagnosis of DVT can be rejected with a high degree of probability.
Instrumental diagnostics Ultrasound compression duplex angioscanning is the main method of examination for suspected venous thrombosis. The mandatory scope of the study includes examination of the saphenous and deep veins of both lower extremities, since there is a possibility of contralateral thrombosis, which often occurs asymptomatically. If the patient has symptoms of pulmonary embolism and there are no ultrasound signs of DVT in the main veins of the extremities, pelvis, and IVC, the gonadal, hepatic, and renal veins should be examined. An active search for DVT using ultrasound angioscanning seems appropriate in the preoperative period in patients at high risk of VTEC, as well as in cancer patients. In these same patients, it is advisable to conduct ultrasound angioscanning for screening purposes after surgery. When thrombosis spreads to the iliocaval segment, if it is impossible to determine its proximal border and nature according to duplex ultrasound scanning, radiopaque retrograde iliocavography or spiral computed tomography (CT) is indicated. During angiography, a number of therapeutic manipulations are possible: implantation of a vena cava filter, catheter thrombectomy, etc.
Periphlebitis: symptoms
There are two types of acute inflammation of the venous vessels: acute superficial thrombophlebitis and periphlebitis. The second type differs from the first in that the wall of even the largest superficial vessel is affected by the inflammatory process from the outside.
The clinical picture of superficial periphlebitis is variable, but at the same time, pronounced. Therefore, its course is unnoticeable in extremely rare cases.
!
The first sign of periphlebitis will be a change in body temperature.
In this case, it will be an atypical or so-called “wrong” fever. It is characterized by the fact that daily temperature fluctuations do not have any patterns. This type of fever occurs in patients with influenza, ARVI, pneumonia, rheumatism, etc.
Against the background of fever, the patient develops venous insufficiency and an increase in the spread of inflammation. Initially, pastiness is formed in the area affected by the pathology. The area of skin above which becomes pale and doughy. Skin turgor decreases. Subsequently, mild swelling of the skin and subcutaneous tissue is replaced by obvious swelling with a spotty rash or even extensive hemorrhages. And the pallor of the skin is reddened, with a clearly visible vascular pattern of various shades from crimson to bright purple. When palpating this area, prolonged pain occurs.
With the development of periphlebitis, the symptoms become more visible. The venous wall expands and thickens. In the superficial layers of the dermis, the accumulation of serous fluid and purulent exudate is provoked. The patient's situation is aggravated by a decrease in hemoglobin and the development of iron deficiency anemia. As a result, hematomas and bruises appear on the skin. The destructive process of necrosis of blood vessels begins.
Even at the very initial stage, periphlebitis is a direct threat to thrombus formation. Pathogenic microflora contributes to the appearance of infected blood clots and the development of general pyemic phenomena. This condition is extremely dangerous for humans due to the high risk of developing sepsis and blockage of blood vessels in the brain, heart or lungs.
In cases where periphlebitis is chronic, purulent intoxication of the body occurs. It aggravates the patient’s serious condition, manifested by endless migraines, vomiting, weakness, lack of appetite, excessive sweating, etc. In this situation, the development of liver and kidney failure is not uncommon.
If you notice the above symptoms, you should immediately consult a doctor. This is necessary to differentiate the disease and then promptly prescribe a treatment regimen that is adequate to the patient’s condition.
Expert opinion
In no case should the symptoms of periphlebitis be ignored, since if left untreated, this disease can lead to blood clots and the development of trophic ulcers.
Vascular surgeon, phlebologist
Osipova Ekaterina Yakovlevna
Diagnosis of periphlebitis - visiting a doctor
Periphlebitis is an inflammation of the periphlebitis surrounding the vein.
Etiology and pathogenesis
Periphlebitis occurs as a result of the transition of the inflammatory process to a vein from the surrounding tissues with an abscess, burn wound, panaritium, phlegmon, tuberculosis, etc. With non-specific In the bedroom, the outer wall of the vein is swollen and infiltrated. Then swelling and infiltration spread to the middle part of the vein wall, destroying the muscle layer, and to the endothelium. A wall thrombus forms and thrombophlebitis develops. If the process ends successfully, then phlebosclerosis is formed.
Causes of periphlebitis
The most common reason why various types of phlebitis occur, including periphlebitis - varicose veins. It is also possible to develop periphlebitis as a result of an allergic reaction (allergic phlebitis) or as a complication after childbirth (painful phlebitis). In some cases, the disease may occur against the background of an infectious lesion or injury to the vein (violation of the integrity of the vascular wall).
Symptoms of periphlebitis
The disease is characterized by pain in the lower extremities; upon examination, redness is detected along the affected vein; Some compaction is detected by touch.
The main clinical symptoms - pain and hyperemia of the skin along the vein - are observed only in the initial stage of the disease and when the saphenous veins are affected. Upon palpation along the course of the affected vein, a dense, painful cord or infiltrate is detected, indicating the involvement of significant areas of subcutaneous tissue in the inflammatory process.
Treatment of periphlebitis
Treatment of periphlebitis is mainly conservative. Ointments and gels with heparin, troxevasin, as well as thermal physiotherapeutic procedures are prescribed. Anti-inflammatory therapy with NSAIDs is carried out, drugs are used that improve the rheological properties of blood and the trophism of the venous wall.
In physiotherapy, magnetotherapy is indicated first. The action of the magnetic field accelerates tissue regeneration, has anti-inflammatory, decongestant and immunomodulatory effects, reduces blood clotting, reducing the risk of parietal prevents thrombus formation, improves blood and lymph circulation, and causes an antispastic effect.
A new drug, the medicinal patch VAZOPLAST, has shown good effectiveness in the treatment of periphlebitis.
Treatment of periphlebitis with medicinal plaster VAZOPLAST (vasoplast)
The therapeutic plaster VAZOPLAST is intended for the treatment of diseases of the venous system.
The patch has analgesic, anti-inflammatory and muscle-relaxing effects, reduces swelling in the affected area, relieves fatigue and a feeling of heaviness in the legs, improves blood and lymph circulation This, especially venous and lymphatic outflow, improves the rheological properties of blood in the inflammation zone.
The VAZOPLAST patch helps improve vascular permeability, reduce thrombus formation and venous stagnation in the affected area, improves the condition of capillaries, increases elasticity veins and tone, has an angioprotective and venotonic effect.
More details about VAZOPLAST
Superficial periphlebitis of the lower extremities: diagnosis
The first step on the path to healthy legs and improvement of general condition will be a consultation with specialists such as a therapist, vascular surgeon, angiosurgeon or phlebologist. The specialist will collect an anamnesis of the disease, clarify the patient’s complaints and the time of onset of the first symptoms, examine the limb, palpate it and inquire about the presence of concomitant diseases. This will give the doctor the opportunity to make a preliminary diagnosis and prescribe a series of diagnostic tests. What might they include?
First of all, these are general clinical tests. A general blood and urine test is a mandatory diagnostic procedure that allows you to assess the condition of the patient’s body as a whole. This will be followed by instrumental studies. This may be Doppler ultrasound or duplex angioscanning. As a rule, the latest diagnostic method has been used recently. It is the most informative, since the scan determines the speed of blood flow, the presence and size of blood clots, as well as their location. The procedure is painless and safe, however, it has contraindications. In particular, ultrasound cannot be performed in case of violations of the integrity of the skin.
Expert opinion
If a blood test reveals a pathologically low content of total protein, an increase in ESR, a decreased level of hemoglobin and a decrease in the number of red blood cells, then this is an indirect sign of anemia, intoxication of the body, the course of an infectious-inflammatory process of an acute or chronic nature.
Vascular surgeon, phlebologist
Osipova Ekaterina Yakovlevna
The result of a urine test will also give the specialist an understanding of the state of the body. If in a patient it is characterized by protein loss, an increased number of leukocytes and erythrocytes, then with a fairly high degree of probability we can talk about periphlebitis. After reviewing the conclusion of instrumental vein diagnostics, the doctor will make a final diagnosis and select an individual treatment regimen that takes into account all the patient’s characteristics.
Treatment of periphlebitis: basic methods