5 / 5 ( 1 voice )
Tachysystole is a collective concept used to designate disturbances in heart rhythm in the direction of its acceleration. Tachysystole includes several pathologies accompanied by accelerated contraction of the atria or ventricles. Some of them are relatively mild, while others are life-threatening.
Tachysystole is a type of arrhythmia
Characteristics of the concept
What is tachysystole? This concept comes from two words - “tachy” (quickly) and “systole” (contraction). Thus, tachysystole is an acceleration of heart contractions. The normal heart rate is between 60-80 beats per minute. Anything over 80 is called tachyarrhythmia.
These disorders are quite common in cardiology.
The following forms of tachysystole are distinguished:
- sinus tachycardia;
- atrial tachycardia, fibrillation and fibrillation;
- ventricular tachycardia and fibrillation.
Each condition has its own manifestations.
Normal heart rate
heart function is normal - in sinus rhythm
The concept of normosystole usually also refers to the fact that electrical signals that contribute to the sequential electrical excitation of all parts of the heart are generated in the sinus node, which is normally the first-order pacemaker. In all other cases, they speak of pacemaker migration or non-sinus rhythm. These processes are united by the concept of heart rhythm disturbances, or arrhythmias.
Therefore, usually in the ECG conclusion, in addition to the characteristics of the heart rate (HR), in the first place there is a mention of whether the patient has sinus rhythm or not. If the patient sees the term “normosystole” in the protocol, then most likely this means that he has not only a correct, normal heart rhythm, but also a sinus rhythm - that is, it comes from the sinus node, as it should be normally. (Nevertheless, there are formulations of “normosystole” with an even heart rate, but non-sinus rhythm - more on this at the end of the article).
Sinus tachycardia
This condition is not considered a disease and is not life-threatening. With sinus tachycardia, the heart rate exceeds 100 beats per minute.
There are two types of ST:
- Physiological . Appears with pronounced emotional excitement, physical stress, consumption of large doses of nicotine and caffeine. Physiological tachycardia is observed in young children and athletes.
- Pathological . Caused by certain diseases - anemia, fever, thyrotoxicosis, heart failure.
Symptoms of sinus tachycardia are rarely severe. A person may be bothered by a feeling of rapid heartbeat, interruptions in heart function, dizziness, and shortness of breath.
Sinus tachycardia is diagnosed by auscultation or by electrocardiogram. In the physiological form, it is necessary to avoid provoking factors and take sedatives. In the pathological form, the underlying disease is treated.
Sinus tachycardia is normal for newborns
Normosystole with atrial fibrillation
Of all rhythm disturbances, only this type of arrhythmia, such as fibrillation or atrial flutter, is divided into normo-, tachy- and bradysystolic variants. In this case, the diagnosis “atrial fibrillation, normosystole” indicates a pathology in the form of arrhythmia, but with a normal final heart rate.
normosystolic form of atrial fibrillation - despite the “waves” of atrial flutter/fibrillation, contraction of the ventricles of the heart occurs at a normal frequency
In this case, we are talking about both a permanent form of atrial fibrillation, when a person lives for a long time (months and years) with an irregular or non-sinus rhythm, and a paroxysmal form (paroxysm - attack), when a non-sinus rhythm occurs suddenly and may well recover spontaneously or with the help of medications. Diagnostic criteria are similar to those for normo-, brady- and tachysystole in sinus rhythm - from 60 to 80, less than 60 and more than 80 beats per minute, respectively.
With a permanent form of atrial fibrillation, normosystole is usually more easily tolerated by patients in terms of the sensation of interruptions in the work of the heart, since bradysystole is fraught with a decrease in cardiac output and resulting fainting, and the heart rate during tachysystole sometimes reaches 200 beats per minute, which can lead to severe circulatory disorders.
Supraventricular tachycardia
These conditions are associated with rapid contraction of the atria. There are several forms of pathology.
Table. Characteristics of atrial tachycardias:
| Form | Symptoms | Treatment instructions |
| Paroxysmal tachycardia - regular contractions are observed with a frequency of 150-230 per minute | Starts and stops suddenly. A person complains of an attack of rapid heartbeat and severe weakness. A decrease in pressure may be observed, and with significant hypotension, acute heart failure develops | You can stop the attack by inducing vomiting or coughing, inhaling with straining, and massaging the interclavicular fossa. The drugs used are adenosine or verapamil intravenously |
| Multifocal atrial tachycardia - the appearance of three or more consecutive extrasystoles | Usually not felt sick, numerous extrasystoles can cause weakness and dizziness | Verapamil is used intravenously |
| AV nodal tachycardia - increased frequency of atrial contractions up to 130 per minute | Manifested by dizziness. Usually occurs due to intoxication with glycosides, heart attack, heart surgery | Does not require specific treatment |
These diseases are also not life-threatening. For diagnosis, an electrocardiogram or Holter monitoring is used, where attacks of increased contractions are recorded.
Atrial fibrillation
This is an uncoordinated contraction of the muscle fibers of the atria, in which the heart rate reaches 700 beats per minute.
There are two forms of fibrillation:
- paroxysmal - lasts no more than two days;
- chronic - lasts more than two days.
Atrial fibrillation is registered in 0.5% of the population, but among people over 65 years of age it occurs in 5%.
Causes
30% of the population has an idiopathic form of the disease, that is, it has no apparent cause.
In the rest, the pathology develops against the background of cardiac and extracardiac diseases:
- heart attack;
- pericarditis or myocarditis;
- heart surgery;
- heart defects;
- hypertension;
- cardiomyopathy;
- alcoholism;
- thyrotoxicosis;
- TELA;
- electrical injury;
- pneumonia.
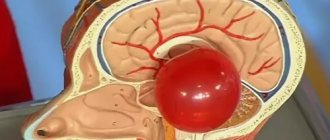
More often, the pathology develops against the background of heart disease. Many foci appear in the cardiac tissue that generate electrical impulses (photo). As a result, excitation and contraction of individual areas of the myocardium occur.
Mechanism of development of atrial fibrillation
Manifestations
Patients with atrial fibrillation complain of increased fatigue, dizziness, a feeling of rapid heartbeat, shortness of breath, and attacks of loss of consciousness. In some patients with underlying heart disease, signs of heart failure increase. Less commonly, there are no complaints - the asymptomatic form.
The examination reveals characteristic signs of the underlying disease. On auscultation, a rapid heartbeat is recorded.
Diagnostics
The diagnosis is confirmed after instrumental studies:
- ECG . There is an absence of P waves (normal atrial contractions); instead, specific f waves appear. There is an irregular heart rhythm.
- Holter monitoring . It is carried out to determine the number of attacks of fibrillation per day.
- Ultrasound of the heart . Detects heart disease, assesses ventricular function, and detects intracardiac blood clots.
To exclude thyrotoxicosis as a cause of fibrillation, the content of thyroid hormones in the blood is examined.
Therapeutic measures
Treatment goals for atrial fibrillation:
- restoration of normal rhythm;
- prevention of paroxysms of fibrillation;
- prevention of complications, primarily thromboembolic.
If the rhythm is severely disrupted, emergency defibrillation is performed.
Restoring a normal rhythm helps improve the patient’s overall well-being and reduces the risk of thromboembolic complications. For this purpose, first class antiarrhythmic drugs are used - Propafenone or Amiodarone. The drugs are administered orally or intravenously. In case of chronic fibrillation, anticoagulants are prescribed on a regular basis.
Surgical treatment is indicated when conservative methods are ineffective. It consists of destroying the AV connection with a radio knife and installing an artificial pacemaker.
Atrial flutter
This is a regular contraction of the atrium muscle with a frequency of 250-300 per minute. It is rarely observed, as it is an unstable condition that quickly turns into a normal rhythm or fibrillation. It can be paroxysmal or chronic.
The causes and symptoms of flutter are no different from those of fibrillation. The ECG shows sawtooth F waves at the site of the P waves.
Treatment is similar to fibrillation.
F waves in atrial flutter
Prevention of tachysystole
Prevention of attacks of tachysystole has problems in the context of ischemic cardiomyopathy, since it is very difficult to predict in advance the effectiveness of a particular drug. During long-term use of the drug, one must take into account its side effects. It is because of this that those drugs with minimal side effects are preferred.
The most promising drug for the prevention of attacks of tachysystole is Ethmozin. Since with its long-term use it has practically no side effects and at the same time success with its use is achieved in 50% of all identified cases. Also, in a number of cases, a convincing effect was obtained from “Ri and Isotin”.
If you have been diagnosed with this by a qualified specialist, then you first need to follow all his recommendations to improve your health. In addition, you should not self-medicate, because traditional medicine can only worsen your health condition. After diagnosing tachysystole, constant supervision by the attending physician is necessary. If new symptoms appear, you should seek advice from a medical institution to avoid a sharp deterioration in health.
Paroxysmal ventricular tachycardia
This is a condition that occurs as a result of the appearance of three or more ventricular extrasystoles following each other.
Causes
There is an idiopathic form that occurs for no apparent reason. In other cases, ventricular tachycardia develops against the background of any heart disease. An ectopic focus forming in the ventricle causes its extraordinary contractions.
Symptoms
The clinical picture of paroxysmal tachycardia is poor. The patient complains of dizziness, clouding of consciousness. A decrease in pressure is objectively determined.
Diagnostics
Ventricular tachycardia is determined using an electrocardiogram. There is a deformation of the QRS complex (contraction of the ventricle), overlapping of the atrial and ventricular complexes.
Treatment
In most cases, the condition does not require specific treatment. A persistent attack of VT is treated with intravenous lidocaine. Signs of hemodynamic compromise require defibrillation.
Ventricular fibrillation and flutter
These rhythm disturbances are characterized by uncoordinated contraction of the ventricles at a rate of 250-300 per minute. On the ECG it is recorded as a sinusoidal curve. Leads to cardiac arrest and clinical death.
Emergency defibrillation is required and resuscitation measures are taken. To prevent this condition, patients have a cardioverter-defibrillator installed in the heart area.
Tachysystolic heart rhythm disturbances are a large group of conditions characterized by various types of increased heart rate. Some of them are safe for life and do not cause any clinical manifestations. Some arrhythmias are life-threatening and require urgent treatment.
Common deviations from the norm (brady- and tachysystole)
Sometimes the ECG conclusion may include a combination of normosystole and irregular sinus rhythm - “normosystole, irregular rhythm.” The latter can occur, for example, with respiratory or sinus arrhythmia. In this case, the rhythm comes from the sinus node (as it should be normally), but there are minor functional fluctuations in the heart rate due to the phases of inhalation and exhalation (normally, when inhaling, the heartbeat speeds up slightly, and when exhaling, it slows down slightly). Therefore, if a patient sees a conclusion about normosystole with an irregular but sinus rhythm, there is no point in panicking.
When a patient experiences an increase or decrease in heart rate, the doctor describes this as tachycardia or bradycardia. But sometimes he may write about tachysystole or bradysystole, which literally means frequent or rare heartbeats, respectively. In this context (assuming sinus ri and “systole” are synonymous.
Again, tachysystole and bradysystole can occur both in a completely healthy person and in various diseases of the heart or other organs. Here everything depends on other nuances obtained from the ECG. But if a person has a sinus rhythm with a slightly slow heart rate (at least 50 per minute) or increased heart rate (90-100) - especially from excitement, then we can talk about normal indicators.