Published: 07/07/2021 11:15:00 Updated: 07/07/2021
Thrombosis is a complete or partial blockage of the lumen of a vessel by a parietal or mobile thrombus. A thrombus is a dense blood clot that appears as a result of a change in its fluidity. Normally, thrombus formation is a protective mechanism. Damage to the vascular wall leads to a slowdown in blood flow and accumulation of platelets around the damage. The thrombus literally “darns” the wall of the vessel.
The classic causes of thrombosis are described by Vikhrov’s triad: damage to the vascular wall, slowing of blood flow and changes in blood properties [3]. Some blood clots (they are called emboli) are able to move to narrower areas of the vessel, which are completely or partially blocked. Every year, about 25 million people die from thrombosis, and even more face trophic disorders caused by blood clots [3].
Types of vascular thrombosis
The most common thrombosis of the lower extremities, however, the greatest danger is pulmonary embolism - PE - and disseminated intravascular coagulation syndrome - DIC syndrome.
Arterial thrombosis develops when its lumen is blocked by a thrombus or embolus. Clinical signs are determined by the location where the blockage occurs, an organ or tissue that has little or no blood supply. If blockage with impaired vessel patency occurs slowly, “spare” collateral vessels open, which mitigates the clinical symptoms of arterial thrombosis [3]. Arterial thrombosis occurs more often in middle-aged and elderly men [7].
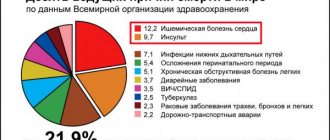
Vein thrombosis varies depending on the location of the lesion into deep or superficial vein thrombosis and pulmonary embolism. Among all cardiovascular pathologies, venous thrombosis ranks third in frequency of occurrence, second only to ischemic heart disease and atherosclerosis. The third place in the structure of causes of mortality is occupied by pulmonary embolism. Starting at age 40, the risk of developing venous thrombosis doubles every 10 years [5].
Two variants of damage to the veins of the lower extremities are described: phlebothrombosis (primary thrombosis, the thrombus is not firmly fixed) and thrombophlebitis (secondary thrombosis due to inflammation of the vessel wall, the thrombus is firmly fixed) [6]. Thrombophlebitis is more often associated with superficial vein thrombosis [2]. The larger the vein affected by thrombosis, the more pronounced its clinical manifestations. The surrounding tissues are compressed by stagnation of blood, since the blood stays at the site of occlusion, but does not move towards the heart. Venous blood clots tend to break off and travel through the bloodstream (thromboemboli). When they enter vital organs, life-threatening conditions develop [3].
How the treatment method works
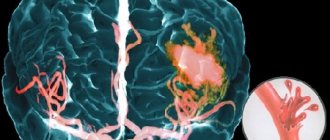
Removal of blood clots in modern clinics is controlled by CT angiography. With its help, you can very accurately determine the location of the blood clot and plan the course of the operation. Recently, percutaneous mechanical thrombectomy is more often used to remove blood clots from the arteries of the brain. A guide catheter is inserted into the femoral artery in the groin and then guided (visually controlled using a CT scan) to the site of the blockage. The catheter carries a special stent, which is folded. Passing through the thrombus, the stent straightens and captures it. The thrombus captured by the stent is removed through a micro-incision in the artery. If thrombectomy is not possible for any reason (for example, if the thrombus is located in an arterial branch), thrombolysis is performed. This method allows you to restore blood supply to brain tissue faster than with anticoagulant therapy.
Risk factors for thrombosis
Internal:
- arterial hypertension [7];
- pregnancy, childbirth, postpartum period [3];
- biochemical changes in blood [2,3,5,7];
- vasculitis [2];
- age over 40 years [5];
- congenital thrombophilia, thrombosis, varicose veins of the lower extremities [3,5];
- congestive heart failure [5, 6];
- malignant neoplasms, radiotherapy and chemotherapy [3];
- strokes [3, 6];
- myeloproliferation [2, 5, 7];
- nephrotic syndrome and renal failure [5, 6, 7];
- obesity (BMI over 30) [3];
- myocardial infarction [6];
- diabetes mellitus [6, 7];
- systemic lupus erythematosus [2];
- chronic pulmonary diseases [3];
- enterocolitis [5].
External:
- heroin addiction [2];
- hormonal therapy [3,5];
- dehydration due to vomiting, diarrhea, increased sweating, direct lack of fluid [6];
- immobilization [3];
- travel by plane, bus or in a seated car [3];
- infectious diseases, including COVID-19 [1, 3, 5, 9];
- catheterization of central and peripheral veins [2, 5];
- smoking [6, 7];
- sedentary lifestyle [3];
- operations [3];
- fractures of large bones, other injuries [3];
- taking oral contraceptives [5];
- taking Diazepam, Amiodarone, Vancomycin [2];
- sclerotherapy and thermal ablation [2];
- condition after joint replacement [3];
- holding an awkward position [3].
Symptoms and manifestations of cerebral thrombosis
General cerebral group of symptoms:
- High intensity headache;
- Nausea and vomiting;
- Impaired sensitivity of the limbs, facial skin;
- Asymmetry of facial muscles;
- Decrease in hell;
- Weak pulse filling;
- Convulsions;
- Increased intracranial pressure;
- Paralysis and paresis;
- Photophobia.
Focal symptoms that manifest differently in certain areas:
- Double vision;
- Narrowing of the field of vision, reducing its acuity;
- Skin cyanosis;
- Difficulty moving the eyeballs, their protrusion.
Symptoms caused by intoxication of the body:
- Hyperthermia;
- Chills, aching joints;
- Weakness, lethargy;
- Drowsiness.
With thrombosis of the venous sinuses caused by an infected blood clot, the patient is diagnosed with confusion, fever, excessive sweating, and sallow skin color.
Thrombosis Clinic
Symptoms of thrombosis can be general, regardless of location, or specific.
Common symptoms include pain with movement and at rest, limited mobility, and decreased function of the affected organ or tissue. Symptoms of arterial obstruction (acute thrombosis, or gradual obstruction of vessel patency):
- asymmetry of blood pressure when measured on both arms [7];
- pallor of the skin, turning into cyanosis [7];
- pain at rest at night [7];
- pain when moving in the thigh, buttock, lower leg, foot, shooting or aching [7];
- sleep disorders [7];
- numbness, coldness of the limb [7];
- absence of peripheral pulsation [7];
- necrosis (necrosis) of affected tissues, trophic ulcers, gangrene [7];
- intermittent claudication [7].
Symptoms of venous thrombosis:
- pain [6];
- swelling, soft and asymmetrical [6];
- blue discoloration of the skin (skin cyanosis) [6];
- increased skin temperature of the extremities [6];
- increased sensitivity and compaction in the projection of the superficial veins [2];
- post-inflammatory hyperpigmentation [2];
- dilated saphenous veins [6];
- erythema [2].
Sometimes the only symptom of venous thrombosis is PE [6].
How is pulmonary embolism diagnosed?
As a result of pulmonary embolism, cardiac function, pulmonary blood flow and gas exchange are disrupted. This condition is accompanied by characteristic symptoms, primarily a rapid heartbeat. There may also be a stabbing pain in the chest that gets worse while breathing. Patients may experience severe shortness of breath, and the respiratory rate may increase to 30-40 per minute. In addition, cyanosis or pallor of the skin, decreased blood pressure, cough, and hemoptysis may be observed.
“In the case of pulmonary embolism, difficulty breathing and chest pain may occur. In people with a disease of the vascular-cardiac system, for example, atrial fibrillation, pulmonary embolism can occur quite often,” says Shpachenko.
If thromboembolism is suspected, urgent hospitalization is required. To confirm the diagnosis, the hospital will order electrocardiography, chest x-ray and echocardiography. A radionuclide scan of the lungs, probing of the right side of the heart, and computed tomography with contrast of the pulmonary arteries can also be performed.
Diagnosis of thrombosis
Primary diagnosis is based on a detailed history and anthropometry (calf or thigh circumference).
The Wells scale is used to diagnose acute thrombosis and diagnose pulmonary embolism [8,9]. Instrumental diagnostics include compression or duplex scanning of veins, Doppler ultrasound with compression of veins, impedance plethysmography, pulmonary angiography, radiocontrast or MRI venography [6,9], CT and MRI angiography [7,9].
To diagnose arterial thrombosis, physical tests are used (6-minute walk test, treadmill test), determination of pulsation of superficial arteries (arteries of the dorsum of the foot), duplex scanning of the arteries of the extremities, angiography (X-ray of a vessel filled with a radiopaque substance) and measurement of transcutaneous oxygen tension [ 7].
Diagnostics
Blockage of a cerebral vessel by a blood clot is an emergency condition that requires urgent diagnosis. There is a rapid test that allows you to assume the presence of pathology before instrumental examination.
What is suggested for the patient to do:
- Show tongue. Due to impaired blood circulation in the brain, the patient’s tongue will bend and fall to one side.
- Smile. A symmetrical smile with ischemia will be impossible; it will turn out to be one-sided.
- Raise your hands up. A patient with thrombosis will not be able to do this.
- Say a short sentence of a few words like “we are going to the store to buy bread.” Impaired blood supply to the brain will make speech slow and slurred.
Diagnostic methods:
- Ultrasound with Doppler sonography;
- Angiography;
- Rheoencephalography;
- MRI.
Tests for thrombosis
Laboratory indicators play a significant role in the timely diagnosis of thrombosis.
Thus, guidelines for the management of patients with a new coronavirus infection provide for stratification of the risk of coagulopathy in patients with COVID-19 based on simple laboratory tests: D-dimer, prothrombin time, platelet count, fibrinogen level [1,9]. A clinical blood test can detect inflammation. It also determines the level of platelets, that is, the very substrate of thrombosis.
Additionally, the level of inflammation in the blood and the risk of thrombosis is indicated by an increased level of C-reactive protein.
Biochemical analysis primarily demonstrates blood glucose levels. It can be used to judge the presence of diabetes, one of the most serious risk factors for thrombosis.
Also, a biochemical analysis can determine the level of protein C, which also characterizes the severity of the risk of thrombosis.
Elevated levels of homocysteine in the blood are also a currently proven risk of thrombosis, leading to miscarriage and cardiovascular events (heart attacks and strokes).
D-dimer is a laboratory marker of fibrin formation [8]. It also indicates the presence of inflammation, just like C-reactive protein. The level of D-dimer is a control indicator of COVID-19 and its complications, including those associated with thrombosis.
You can take tests under the comprehensive Thrombosis program, which includes determining the levels of Antithrombin-III, D-dimer and genetic factors of cardiac diseases and platelet levels. This program allows you to determine the fact of thrombosis occurring somewhere in the body, as well as determine the genetic predisposition to it. This program, like other tests, is offered by the CITILAB network of clinics.
Additional determination of homocysteine and C-reactive protein levels will help determine the biochemical risk of thrombosis.
Stray thrombus: a health hazard
21.10.2019
If you believe the statistics, wandering blood clots cause the death of more than 9 million people every year. The reason for the appearance of these “killers” in the body is often people themselves. There are bad habits that accelerate their formation. It is necessary to get rid of them so as not to become a victim of a blood clot .
Fatty food
A diet high in fat increases the amount of cholesterol in the blood . It sticks to the walls of blood vessels in the form of cholesterol plaques and blood clots. At any moment they can break off and rush through the bloodstream. This is dangerous for human life. Therefore, it is useful to eat fresh vegetables along with fatty foods. They will reduce the harmful effects of fat.
Sedentary lifestyle
If a person moves little, gets to work by car, or takes an elevator to the floor, then cholesterol settles faster of blood vessels To prevent cholesterol plaques from settling, you will have to move for at least 40 minutes 3 times a week. Evening walks, swimming and skiing are useful.
Smoking
Smoking is dangerous to life, especially after a meal. When eating food, the blood , and nicotine activates the process of their deposition on the walls of blood vessels . If a person cannot help but smoke, then he must at least refrain from the bad habit in the first hour after eating.
High heels
Women love high-heeled shoes. However, they provoke varicose veins. This, in turn, activates the growth of blood clots. Heels higher than 4 cm should not be worn.
Danger of blood clots
When cholesterol plaques form in the vessels clot adheres to them . When it grows large, it breaks off and “travels” through the circulatory system. When a blood clot clogs a blood vessel in the brain , a stroke occurs. If heart vessel in a heart attack . If a blood clot blocks an artery in the lungs, the person dies. Doctors use an ultrasound to detect an enlarged blood clot , from which the blood clot . Then the person will be saved by surgery . The cardiovascular surgeon inserts a filter into the vessel , which intercepts the dangerous clot.
Useful products for blood vessels
To strengthen blood vessels, it is wise to include the following foods in your diet:
- you need food containing vitamin E. It increases the firmness and elasticity of the walls of blood vessels , preventing cholesterol plaques from settling on them. This vitamin is sufficient in eggs, green onions, liver , lettuce, peas and beans;
- You also need to eat more foods with vitamin C. It strengthens capillaries, thins the blood , and blood promotes thrombus formation. To enrich the body with this useful element, you will have to drink tea with rose hips and lemon, eat cabbage, sweet peppers, garlic, oranges and grapefruits;
- It is necessary to include products with bioflavonoids in the menu. These substances can dissolve intravenous blood clots. To replenish the supply of this unique substance, you need to eat berries and red fruits every day. These are apples, lingonberries, cranberries and cherries.
Many people love to enjoy fried potatoes. If you don’t have the strength to give it up, then you need to at least add less salt.
Who is at risk for a wandering blood clot?
- If a person consumes a lot of fried and smoked food, then the occurrence of a blood clot increases sharply.
- When a woman suffers from varicose veins and uses contraceptives for several years, her risk of developing a blood clot increases.
- Smoking more than 5 cigarettes a day and bone also provoke the formation of blood clots.
Daily walks, eating vegetables and fruits, the absence of varicose veins and smoking cigarettes will exclude a person from among the victims of a wandering blood clot .
Published in Cardiology Premium Clinic
Treatment and prevention of thrombosis
Treatment of thrombosis includes anticoagulant and antiplatelet therapy, thrombolytic therapy, installation of an inferior vena cava cava filter, and surgical removal of the thrombus [5].
Complications of anticoagulant therapy must be kept in mind: major bleeding, heparin-induced thrombocytopenia and warfarin-induced skin necrosis [5]. To reduce the risk of continued thrombus formation, NSAIDs are used [2]. For the purpose of secondary prevention, small doses of heparin are prescribed. Non-drug treatment methods are also prescribed - elastic bandaging, compression hosiery, local hypothermia and exercise therapy [2, 4].
Prevention of thrombosis includes a number of measures used in situations of increased risk of thrombosis.
Primary prevention of atherothrombosis:
- systematic physical activity in the form of walking or morning exercises;
- blood pressure control, maintaining working blood pressure below 140/90 mmHg;
- control of blood sugar levels (less than 6 Mmol/l), early detection and treatment of diabetes mellitus;
- weight loss, body mass index less than 25 kg per m2;
- a diet limited in cholesterol and high-density fat (total cholesterol less than 5 mmol/l), fruits and vegetables;
- smoking cessation [3,7].
Primary prevention of venous thrombosis:
- compression underwear;
- bandaging with elastic bandages;
- drinking plenty of fluids, especially after surgery;
- regular exercise, walking, especially when traveling;
- prohibition of taking alcohol and sleeping pills in large doses;
- prohibition of the use of compressive shoes and clothing [2,5,6].
Sometimes, during periods of particular risk, anticoagulants are prescribed several days before the flight. There is no point in taking aspirin in such cases [5].
Briefly about the treatment method
For ischemic stroke, the most effective and reliable method of removing blood clots from the arteries of the brain is thrombectomy. There are several options for the procedure: - Aspiration thrombectomy. During the operation, a micro-incision is made through which a special catheter is inserted. Through it, saline solution flows under pressure into the affected vessel. Under the influence of the solution and salt, the thrombus softens, is divided into pieces and aspirated (suctioned out) using a syringe. Thanks to this method, the number of injuries to the internal walls of blood vessels is reduced. — Percutaneous mechanical thrombectomy. A catheter with a stent is inserted through a large artery. With the help of a stent, the clot is captured and removed through an incision in the vessel. This method is most often used in the treatment of stroke caused by blockage of blood vessels in the brain.
Bibliography
- Consensus position of experts of the Eurasian Association of Therapists on some new mechanisms of the pathogenesis of COVID-19: focus on hemostasis, issues of blood transfusion and the blood gas transport system / G.P. Arutyunov, N.A. Koziolova, E.I. Tarlovskaya, A.G. Arutyunov, N.Yu Grigorieva, etc. // Cardiology. 2020;60(6). DOI: 10.18087/cardio.2020.5.n1132.
- Thrombophlebitis (thrombosis of superficial veins): modern standards of diagnosis and treatment / V.Yu. Bogachev, B.V. Boldin, O.V. Jenina, V.N. Lobanov//Hospital-substituting technologies: Outpatient surgery. 2016.- 3-4 (63-64)- P.16-23.
- Modern problems of thrombosis of arteries and veins / I.N. Bokarev, L.V. Popova // Practical Medicine, 2014. - No. 6 (82) – P13-17.
- Treatment of thrombophlebitis. Current recommendations and clinical practice / P.F. Kravtsov, K.V. Mazaishvili, S.M. Markin, H.M. Kurginyan // Thrombosis, hemostasis and rheology, 2020 No. 2 – P 68-72.
- Venous thrombosis: modern treatment / P.S. Laguta // Atherothrombosis, 2015 - No. 2 - P. 7-16.
- Deep vein thrombosis of the lower extremities / A.K. Lebedev, O.Yu. Kuznetsova // Russian family doctor, 2015.
- National recommendations for the diagnosis and treatment of diseases of the arteries of the lower extremities, Association of Cardiovascular Surgeons of Russia, Russian Society of Angiologists and Vascular Surgeons, Russian Society of Surgeons, Russian Society of Cardiology, Russian Association of Endocrinologists, M, 2021.
- Diagnosis and pharmacotherapy of acute venous thrombosis / N.V. Sturov, G.N. Kobylyanu// Difficult Patient, 2013., No. 12., T. 11. –P.19-22.
- Principles of management of patients with venous thromboembolism during the COVID-19 pandemic // V.Ya. Khryshchanovich // Surgery News, 2021.- t28 No. 3 – P329-338.
Provocateurs of hemorrhagic stroke
The trigger for the appearance of HI can be quite a variety of factors that have a negative impact on intracranial hemodynamics and the condition of the cerebral vessels:
- persistent arterial hypertension (in 50% of cases);
- cerebral amyloid angiopathy (12%);
- oral administration of drugs from the anticoagulant spectrum (10%);
- intracranial neoplasms (8%);
- other causes are arteriovenous and cavernous malformations, thrombosis of the cerebral sinuses, aneurysms, vasculitis of intracranial vessels, etc. (20%).
Many of the patients with a history of hemorrhagic stroke have diabetes mellitus. It is a proven fact that diabetics, like hypertensive patients, are at risk. In long-term diabetes mellitus, blood vessels, including cerebral ones, are destroyed due to modification of blood chemistry with a predominance of glucose. If, against the background of elevated blood sugar, there is a tendency to constant increases in blood pressure, the likelihood of a hemorrhagic stroke increases by 2.5 times.
Pathogenetically, a hemorrhagic effect can develop as a result of rupture of a vessel (the predominant mechanism) or the leakage of blood elements into the surrounding brain tissue through the walls of capillaries due to their impaired tone and permeability. In the second option, there is no rupture and, as such, profuse hemorrhage. Just a small vessel allows blood to pass through pointwise. But even small-point hemorrhages, merging, can turn into very extensive foci, with no less fatal consequences than after a rupture of an artery or vein.
Bleeding in the brain (hemorrhagic stroke)
2. The second clinical stage of cerebral hemorrhage is characterized by hemiplegia, i.e. paralysis of both limbs, facial and hypoglossal nerves on one side of the body.
First of all, it should be noted that hemiplegia almost always exists already during the period of loss of consciousness. Indeed, already at this time one can notice mostly asymmetry on the face, which is expressed in the fact that on one side the forehead and nasolabial fold are smoothed, the corner of the mouth is lowered and the mouth is slanted; on the same side, the cheek passively inflates with each exhalation. If you alternately lift the upper and lower limbs on the corresponding side and then release them, they fall heavily, “like a whip,” while on the opposite side of the limb, being raised, they fall more slowly, due to the fact that the muscles in them have relatively retained their tone. As consciousness begins to recover, the hemiplegia becomes more and more noticeable; while the patient is already able to move his healthy arm and leg, the paralyzed limbs remain completely motionless.
When consciousness has fully recovered, you can begin a more detailed study. At the same time, the asymmetry of the face is very clearly noticeable, especially if you make the patient smile; Whistling and blowing out the candle are impossible. Often there is also a speech disorder in the form of dysarthria; the patient pronounces words very poorly due to the fact that the movements of the tongue and lips are difficult. This speech disorder should not be confused with aphasia, in which it is not the pronunciation of words that is impaired, but the ability to express one's thoughts in appropriate words and understand the thoughts of others. When protruding, the tongue deviates to the painful side, due to the fact that m takes over. genioglossus healthy side.
As for facial paralysis in particular, with it the upper branch of the facial nerve is always more or less captured; on the diseased side, the eyes, especially at first, are more open than on the healthy side, and the corresponding eyebrow is lowered. If you force the patient to raise his eyebrows, you will see that on the healthy side the eyebrow rises faster and higher than on the paralyzed side. Thus, the preservation of the function of the upper branch of the facial nerve turns out to be only relative and is explained by the fact that with any hemiplegia, the muscles for associated movements (such as the muscles of the larynx, abdomen, chest) are affected to a much lesser extent than muscles that do not act together.
For the most part, facial paralysis is observed on the same side on which the upper and lower limbs are paralyzed. Sometimes there is hemiplegia alternans, i.e. paralysis of the facial nerve on one side and paralysis of the limbs on the other side of the body. In this case, we are dealing with hemorrhage not in the cerebral hemisphere, but in the pons or in the cerebral peduncle.
If the hemorrhage was insignificant and especially if it only caused compression of the pyramidal tract, then little by little movements can be completely restored, first in the lower, then in the upper limb. But for the most part this is not observed, and after a few weeks the disease enters the third period. This is indicated by the following two important phenomena, which are often noticed just a few days after the development of hemiplegia: 1) an increase in tendon reflexes on the affected side, which is all the more striking because before the reflexes could have been lost or at least weakened; 2) foot clonus. Once these phenomena are somewhat clearly expressed, we must wait for the imminent onset of the third period or the period of contracture.