Haptoglobin is a blood plasma protein produced by the liver. Its function is to bind hemoglobin and participate in inflammatory reactions.
Hemoglobin is an iron-containing protein that is found in red blood cells and ensures the transport of oxygen to the tissues and cells of the body. Over time, red blood cells break down—usually their life cycle is about 120 days—and free hemoglobin enters the blood, where it is bound by haptoglobin and processed in the spleen.
If binding does not occur, free hemoglobin enters the kidneys and can cause kidney damage. Such situations arise when the body's consumption of haptoglobin is faster than its production by the liver, for example, when a large number of red blood cells are destroyed (hemolysis), or in liver diseases, in which hemoglobin production is reduced.
The causes of hemolysis can be both hereditary and acquired - among them are incompatibility of blood groups and Rh factor during transfusion, drug and toxic effects, mechanical damage, hemodialysis, infections - malaria, hemolytic streptococcus, gas gangrene. In these cases, hemolytic anemia develops, in which weakness, pallor or yellowness of the skin and mucous membranes, darkening of urine and renal failure are observed.
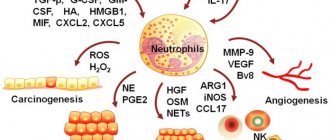
Another important function of haptoglobin is participation in the acute phase reaction, which develops in response to infection, damage, and tumor process. Haptoglobin acts as an antioxidant, reduces cell damage, slows down the growth of bacteria, inhibits the production of prostaglandins, and participates in the regulation of the immune system. In the presence of inflammatory processes in the body, the level of haptoglobin in the blood increases.
general characteristics
Haptoglobin is a protein of the acute phase of inflammation, synthesized mainly in the liver, as well as in adipose tissue, lungs and binds free hemoglobin released from red blood cells. It is stimulated by inflammatory mediators, with a peak increase observed on days 4–6 and normalizes within 2 weeks after removal of the stimulating factors. With hemolysis of erythrocytes, the level of plasma haptoglobin decreases rapidly, which, in the absence of other causes, is a sensitive marker of intravascular hemolysis. Normally, about 1% of red blood cells are destroyed and removed from circulation per day. An increase in this amount to 2% leads to the complete disappearance of haptoglobin. The haptoglobin-hemoglobin complex is quickly taken up from the circulating blood by reticuloendothelial cells, thereby preventing or minimizing the removal of hemoglobin and iron from the body. Haptoglobin prevents kidney damage, since free hemoglobin is excreted in the urine and toxic concentrations of iron cause renal dysfunction. Haptoglobin plays an important role in the control of local inflammatory processes and is a natural bacteriostatic agent in infections with Fe-dependent bacteria (for example, Escherichia coli). Low levels of haptoglobin are observed during pregnancy and in newborns, as well as during estrogen therapy, including oral contraceptives.
Indications for the study
The test is prescribed if the patient has symptoms of hemolytic anemia. These include the appearance of a yellowish tint to the skin, pallor, darkening of urine, and general weakness. It is also carried out when there is a possibility of hemolysis (for example, in patients with an artificial heart valve, in case of damage to a number of toxic substances, during blood transfusion, hemodialysis). The study is carried out when examining patients with liver pathologies, reduced hemoglobin or the number of red blood cells.
The study is used for:
- establishing the cause of anemia;
- monitoring patients with artificial heart valves;
- diagnosis of intravascular hemolysis;
- liver function assessment;
- identifying acute phase reactions;
- monitoring patients after blood transfusion.
Most often, the test results are used to diagnose hemolytic anemia, and also to assess the degree of their severity.
Interpretation:
- Acute infectious diseases, trauma, necrosis, surgery, sepsis, corticosteroid therapy, biliary obstruction, nephrotic syndrome, malignant tumors, plasmacytoma, diabetes mellitus, collagenosis, Hodgkin's disease, fasting.
- Congenital ahaptoglobulinemia, hereditary spherocytosis, hemolytic disease, autoimmune hemolytic anemia; ineffective erythropoiesis, pregnancy, neonatal period, liver disease (cirrhosis), artificial heart valves, intense sports.
Sample result (PDF)
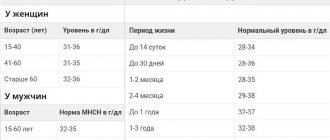
About the normal level of haptoglobin in the blood
Normally, haptoglobin successfully performs its assigned functions. The table shows the age norms for this protein.
| Age | Norm, mg/l |
| Infants up to six months of age | 50 – 480 |
| Children from 6 months and teenagers up to 16 years | 250 – 1380 |
| Adults from 16 to 60 years old | 150 – 2000 |
| People over 60 years old | 350 — 1750 |
The specialized medical literature may provide other normal ranges for haptoglobin. this is because each laboratory has its own reference values. To determine the concentration of haptoglobin, blood serum taken on an empty stomach is analyzed using the immunoturbidimetric method. To identify this glycoprotein, modern high-precision biochemical analyzers are used.
Fecal occult blood test (ColonView)
Rapid test for the qualitative detection of hemoglobin (Hb) and hemoglobin-haptoglobin complex (Hb/Hp) in stool, used for screening of precancerous diseases and colon cancer.
Synonyms Russian
- Immunochemical fecal occult blood test
- Analysis for hemoglobin and hemoglobin-haptoglobin complex in stool
English synonyms
- Hb and Hb/Hp Stool Test
- Fecal Immunochemical Test
Research method
Immunochromatography.
What biomaterial can be used for research?
Cal.
How to properly prepare for research?
- The study is carried out before performing sigmoidoscopy and other diagnostic procedures in the intestines and stomach.
General information about the study
Colon cancer ranks second in the structure of female cancer morbidity, second only to breast cancer, and third in the structure of male morbidity after prostate and lung cancer in Russia. Various methods may be used to screen for precancerous lesions and colon cancer, including:
- direct visualization methods: colonoscopy, flexible sigmoidoscopy;
- indirect imaging methods: computed tomography (CT), magnetic resonance imaging (MRI), capsule endoscopy, double-contrast barium enema;
- stool examination: stool occult blood test (guaiac test and immunochemical tests), DNA test in stool.
Each of these methods has its own advantages and disadvantages. For example, imaging techniques require special bowel preparation, which is often uncomfortable and potentially dangerous for the patient. In comparison, fecal occult blood testing is a painless and much more convenient method for the patient. On the other hand, it is enough to carry out a colonoscopy once every 10 years, while a stool test must be taken every year. In general, we can say that the choice of a screening test is determined by the patient's preferences, the availability of the medical center and the doctor's awareness of new methods. One such new colon cancer screening method is the ColonView occult blood test. This test has several advantages over the traditional guaiac test.
The guaiac occult blood test is the most common method of screening for colon cancer today. It allows you to detect hemoglobin based on the pseudoperoxidase activity of heme in hemoglobin. Thus, the guaiac test detects blood by the presence of heme. A significant disadvantage of the method is:
- low specificity and the need to follow a diet; when consuming foods containing heme or other components that exhibit peroxidase activity (red meat, broccoli, horseradish, turnips, radishes, etc.), the test result may be false positive; this simple test thus requires quite complex preparation;
- low sensitivity (20-50%); Due to the low sensitivity of a single test, it is usually recommended to test 3 stool samples.
The ColonView study is one of the immunochemical methods for determining occult blood in feces (FIT, from the English fecal immunochemical test). Unlike the traditional guaiac test, FIT tests use antibodies specific to human globin. We can thus say that FITs detect blood by the presence of globin. Due to this, immunochemical tests for occult blood are more specific than the traditional guaiac test and do not require diet in preparation for the test.
A feature of the ColonView study that distinguishes it from all other FITs is the use of antibodies to both hemoglobin and the hemoglobin-haptoglobin Hb/Hp complex. When red blood cells are destroyed, hemoglobin or its protein components (alpha and beta globins) bind to a special protein, haptoglobin, which prevents their further oxidation. The Hb/Hp complex is more resistant to acid and proteolytic enzymes during passage through the gastrointestinal tract, which makes the ColonView assay even more sensitive.
Thanks to the improved sensitivity of the ColonView assay, one or two stool samples may be sufficient for analysis. It should be noted, however, that 100% sensitivity will be achieved by analyzing three stool samples.
Like other fecal occult blood tests, ColonView should be repeated once a year. Some doctors recommend a combination of screening tests for their patients, such as a flexible sigmoidoscopy every 5 years combined with one of the immunochemical stool occult blood tests (ColonView) every 3 years.
Some limitations of the ColonView study should be noted:
- Although some investigators have attempted to use this test to diagnose small bowel bleeding, ColonView is currently only approved for the detection of occult lower GI bleeding;
- The test is intended to screen patients at average risk for colon cancer; it does not replace or change the algorithm for diagnosing colon cancer in patients at high risk.
Some features of interpreting the result of a ColonView study:
- a positive test result does not always indicate the presence of precancerous diseases or colon cancer; with other sources of bleeding (diseases: hemorrhoids, angiodysplasia, anal fissure; use of medications: aspirin, warfarin, any means for use per rectum; menstrual bleeding), the test result can also be positive (false positive);
- a negative test result does not completely exclude precancerous diseases or colon cancer; This is because some tumors bleed intermittently rather than continuously, and because the blood may not be evenly distributed in the stool sample.
Given these features, the result of the analysis should be interpreted taking into account additional clinical, laboratory and instrumental data.
What is the research used for?
- For screening of precancerous diseases (adenomas) and colon cancer.
When is the study scheduled?
- Every year, starting from the age of 50, during a preventive examination of the patient;
- every 3 years starting at age 50 when combined with flexible sigmoidoscopy.
What do the results mean?
Reference values: negative.
Positive result:
- the presence of hemoglobin or hemoglobin-haptoglobin complex in the stool (with colon cancer and other sources of bleeding from the lower digestive tract).
Negative result:
- norm;
- false negative result (in the presence of neoplasms that bleed periodically, with uneven distribution of blood in the stool sample).
What can influence the result?
- The nature of bleeding from neoplasms
- Presence of menstrual blood
- Taking certain blood thinners (aspirin, warfarin)
Important Notes
- The test is intended only to detect occult bleeding from the lower digestive tract.
- A positive test result does not always indicate the presence of precancerous lesions or colon cancer.
- A negative test result does not completely rule out precancerous lesions or colon cancer.
Also recommended
- Fecal occult blood test
- Coprogram
- Cytological examination of material obtained during endoscopy (FGDS, bronchoscopy, laryngoscopy, cystoscopy, sigmoidoscopy, colonoscopy)
- Laboratory markers of colon cancer
Who orders the study?
General practitioner, therapist, gastroenterologist, oncologist.
Features of haptoglobin
The behavior of haptoglobin sometimes differs from the functioning of similar acute phase proteins. Since it is produced by the liver parenchyma, its hepatocytes contribute to an increase in HPT in the blood. But a blood biochemistry test does not always confirm the fact of an increase in haptoglobin concentration.
With hemolysis accompanying acute inflammatory reactions, the amount of hemoglobin in the blood is very high. It requires the creation of heavily dispersed complexes and their transportation into the macrophage system. In this case, the concentration of Haptoglobin should decrease. To obtain an objective picture without taking into account the effect of hemolysis, it is important to compare the results obtained with similar tests obtained when diagnosing other proteins from the category of acute-phase proteins.
Author of the article:
Shutov Maxim Evgenievich |
Hematologist Education: Graduated from Kursk State Medical University in 2013 and received a diploma in General Medicine. After 2 years, he completed his residency in the specialty “Oncology”. In 2021, she completed postgraduate studies at the National Medical and Surgical Center named after N.I. Pirogov. Our authors
Haptoglobin in the human circulatory system
Haptoglobin is produced by liver parenchyma cells. In the blood it is represented by three hereditary phenotypes: HPT 1-1, HPT 2-1, HPT 2-2. Constantly present in the blood plasma, Haptoglobin takes up 1.4% of the total protein.
HPT Metabolism Stages:
- The protein binds to hemoglobin released from destroyed blood cells.
- In connection with it, it creates a dispersed complex Hp-Hb , which is sent to the system of macrophages that process waste biomaterial.
- Under the action of macrophages, iron molecules are released.
- The released iron enters the circulatory system, where it combines with the protein transferrin and, together with it, enters the bone marrow to participate in the formation of new red blood cells.
The functioning of haptoglobin is aimed at the intermediate stage of iron metabolism, preventing the valuable element from leaving the body through the urinary system.
Since Haptoglobin has high peroxidase activity, it, in addition to binding hemoglobin, inhibits the oxidative processes of lipids.