- At the first menstruation
- Blood color during menstruation: normal
- Why does the color change
- What changes should you be wary of?
- Scarlet blood during menstruation
- Dark color of blood during menstruation
- Pink color of blood
- Black menstrual blood
- Brown color of blood during menstruation
- Orange period blood
- Gray discharge
- When should you see a doctor?
Menstrual blood can have different shades. The color of the discharge depends on the characteristics of the body and a number of other factors. Blood color can change even during menstruation, which is due to hormonal changes and various diseases.
At the first menstruation
Many teenage girls who have not yet experienced menstruation do not know what its color should be and how not to confuse it with other manifestations. On average, menstruation begins between 11 and 14 years of age. Sometimes we also encounter early puberty - a girl matures by the age of 9, and sometimes menstruation can begin at the age of 15-16, which is considered late maturation. The duration of normal menstruation is from 4 to 7 days. Discharge during the first menstruation is brownish or red in color. They are not too abundant and may appear as several small spots.
During the first menstruation, you especially need comfort and maximum protection. Nuage pads are made of hypoallergenic materials to avoid skin irritation. A special distribution layer and protective edges will prevent leaks. Depending on the intensity of the discharge, you can choose the optimal pad option for different days of the cycle.
Varicocele
Diagnosis of varicocele is mandatory if the partner is not pregnant for more than six months or if the quality of sperm is impaired.
If you suspect a varicocele, it is important to exclude other diseases that give similar symptoms. Considering the fact that dilation of the veins of the spermatic cord may be a consequence of tumors of the retroperitoneum and pelvis, additional examination may be required.
Which doctors should I contact?
Varicocele is detected during preventive examinations. When the first symptoms appear, you should contact, but in the future you need to consult an andrologist.
Treatment of varicocele
Stage 1 varicocele does not require treatment. It is enough to eliminate the cause of congestion in the pelvis (chronic constipation, avoidance of heavy physical activity, etc.). If there is discomfort in the scrotum, pain in the testicle caused by varicocele, cold (an ice pack) applied to the affected area and the prescription of vasoconstrictor medications usually help.
Agents that dilate blood vessels and heat, on the contrary, are contraindicated due to the fact that they only worsen the patient's condition. Conservative treatment methods include:
- restriction of physical activity;
- exclusion of active sports, horse riding;
- wearing a suspensor (a bandage used to immobilize the scrotal organs).
Surgery is indicated in later stages of the disease, when pain symptoms are present, there is hemorrhage in the scrotum, a decrease in testicular volume, in case of infertility and a pronounced cosmetic defect.
Today, methods of surgical treatment of varicocele can be divided into three groups: vein excision, testicular lift, and blockage of veins from the inside (embolization). Surgical treatment of varicocele can be performed using open retroperitoneal access (Ivanisevich or Palomo operation), inguinal and subinguinal method (Marmara operation), as well as laparoscopic access.
The most common is the Ivanisevich operation: ligation of the testicular vein at or just above the internal inguinal ring. This is the simplest but least effective surgical technique. Can be performed under local anesthesia. Disadvantages: large skin incision (4-5 cm), high trauma, cosmetic defect, frequent development of complications.
Microsurgery according to Marmar is recognized as the gold standard, as its effectiveness and safety reach 98%. It is performed through a small (3 cm) incision in the groin area; after the operation, the scar is practically invisible. Performed under local anesthesia. Such an intervention is carried out in the presence of an operating microscope. With high precision, all veins of the pampiniform plexus are sequentially ligated and intersected (in this section of the spermatic cord there are, as a rule, from 3 to 6). In this case, the abdominal cavity is not opened, there is no trauma to the lymphatic vessels of the spermatic cord, which significantly reduces the risk of complications and allows you to resume physical and sexual activity in a short time. The use of optical systems minimizes the risk of ligation of arterial vessels and, accordingly, the risk of testicular necrosis. However, the intervention is considered technically challenging.
Endovascular testicular vein embolization is a low-traumatic intervention performed by vascular surgeons. It is performed under local anesthesia. The doctor makes a small incision in the thigh to gain access to the femoral vein. Through a catheter installed under X-ray control in the testicular vein, a special plug (embolus) or sclerosing agent is inserted to stop blood flow through the vessel.
Advantages of embolization:
- low trauma, virtually no blood loss;
- minimal risk of hydrocele (hydroxycele), since the procedure takes place in a vein and does not affect other blood and lymphatic vessels;
- fast rehabilitation.
Flaws:
- radiation exposure - the operation is performed under x-ray control;
- sometimes the doctor is unable to get into the testicular vein due to the anatomical features of the patient’s venous system;
- a relatively high risk (up to 11%) of developing hematomas, bleeding and perforations.
With laparoscopic venectomy, access to the testicular vein is carried out through small punctures of the anterior abdominal wall and only under general anesthesia.
The doctor inserts an endoscope with surgical instruments inside, which crosses the testicular vein. Surgery with laparoscopic access provides the possibility of simultaneous ligation and excision of testicular vessels on both sides in the presence of bilateral varicocele. Laparoscopic surgery is performed through three punctures. The vein is isolated and ligated from the abdominal cavity. The advantage of laparoscopy is that it is less traumatic. However, with this treatment there remains a relatively high risk of relapse and complications. After surgery, infertility resulting from the development of varicocele is cured in most cases.
Complications
The occurrence of varicocele at a young age can lead to testicular hypotrophy or atrophy and infertility. A connection between varicocele and decreased production of the male hormone testosterone, early ejaculation and impaired potency has been described. Men with this pathology are at risk of losing potency in adulthood and old age.
Sometimes varicocele leads to testicular hypotrophy (reduction in size by more than 10%), up to complete atrophy. This happens due to impaired blood circulation.
With timely treatment, blood supply to the testicle is restored. In most cases, the volume of the organ is also restored.
Stagnation of venous blood in the pelvic veins disrupts the blood supply to the organs; the testes reduce the production of sperm and testosterone. A decrease in testosterone levels leads not only to a decrease in libido and potency, but also to a deterioration in general condition. Metabolic processes slow down, the man begins to gain weight. The amount of adipose tissue increases, which in turn accelerates the decline in testosterone. In addition, varicocele provokes the development of adenoma and prostate cancer.
Due to the rupture of dilated venous vessels or their inflammation, causing severe pain, such serious and rare complications as hemorrhages in the scrotum occur.
After surgery for varicocele, the following complications are possible:
- lymphostasis – impaired lymph outflow;
- purulent discharge at the incision site;
- pain syndrome;
- hydrocele (dropsy of the testicle) is an accumulation of fluid in the tissues of the male gonads.
After therapy, varicocele recurrence is possible.
Depending on the chosen surgical treatment method, the frequency of relapses in children varies from 1 to 20%; in adults, varicocele recurs 2 times less often. In this regard, many doctors recommend performing operations after the end of puberty. Prevention of varicocele
There are no effective methods for preventing varicocele, since this disease is often determined by hereditary factors. Elimination of congestion in the pelvic organs, which involves normalizing stool, eliminating prolonged and severe physical stress, avoiding alcohol abuse, regular sex life, etc. for this category of patients are mandatory.
Experts strongly recommend that all young men aged 19-20 years (at the end of puberty) undergo examination by a urologist/andrologist. If no clinical signs of varicocele are detected, in principle, there is no need to worry about this in the future.
Sources:
- Great Medical Encyclopedia (BME), edited by Petrovsky B.V., 3rd edition, volume 4.
- Akhvlediani N.D., Chernushenko A.S., Reva I.A., Pushkar D.Yu. Subclinical varicocele: criteria for diagnosis, role in the development of male infertility, modern approach to treatment // – Obstetrics and Gynecology. – 2020; 11. – pp. 71-76.
- Kogan M.I., Afoko A., Tampuori D. Varicocele: a controversial problem // – Urology and Nephrology. – 2009; 67(6). – pp. 67-71.
- Laurent O.B., Sokolshchik M.M., Gagarina S.V., Stoyko Yu.M., Golitsyn A.V. Choosing a method for surgical correction of varicocele, taking into account the characteristics of venous hemodynamics // – Urology. 2006; 5. – pp. 24-9.
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment. In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor.
Blood color during menstruation: normal
The normal duration of menstruation is 3-5 days. During this period, their shade may differ. This should not be a cause for concern as this is normal in most cases.
Normally, a woman loses 20-40 ml of blood during menstruation. Menstruation most often begins with discomfort in the lower abdomen in nulliparous women and minor bloody discharge, which gradually increases. This is due to the rejection of the functional layer of the uterus (endometrium) and individual genetic characteristics. In women who have given birth, menstruation begins without pain and the blood has a clear dark red color.
During the middle days of menstruation, the blood is red, ranging from bright to dark shades. This most often depends on the volume of blood: with scanty discharge the shade is darkish, with abundant discharge it is red or burgundy. Mucus and blood clots may be present. During the first three days, menstrual blood may have a rich scarlet color, and this is not considered a deviation from the norm.
The last days of menstruation are accompanied by dark and thick spotting. After this period ends, brown smears may appear. This is due to the complete cleansing of the uterus. During this period, it is enough to use panty liners.
Blood test - What you need to know before donating blood for tests
Category: Information for patients.
A blood test is one of the main methods for laboratory diagnosis of a person’s health condition. The information it contains will help the doctor make or clarify a diagnosis and draw conclusions about the presence of pathological processes in the body. A blood test is prescribed when making a diagnosis, if it is necessary to clarify existing data, during preventive examinations and in many other situations. To obtain an objective picture, two most important conditions must be observed: the correct preparation of the patient for donating blood for analysis and strict adherence to the methodology for collecting material for research.
Preparing for analysis
The day before a scheduled blood test, it is necessary to limit physical activity, exclude sports and excessive exercise. The last meal should be no later than 12 hours before the test. The blood test is performed on an empty stomach; you should not drink tea or coffee in the morning, which can affect the accuracy of the result. It is also necessary to avoid smoking immediately before the study.
As a rule, samples are accepted in diagnostic laboratories from 8 to 10-11 am. To donate blood for testing, you should come early: firstly, so as not to create a rush queue at the end of the work of the medical staff, and secondly, so as not to distort the results of the study. Indeed, to obtain correct results, immediately before the analysis you need to warm up and rest for 15-20 minutes.
Capillary blood examination
The standard method of blood testing, which most patients have been accustomed to since childhood, is the analysis of capillary blood, which comes from a small puncture on the finger. This test is called a general blood test. With its help, you can identify the body's first reaction to inflammation caused by bacteria, viruses and parasites, determine the presence of allergies, and also diagnose severe conditions of the hematopoietic system, such as anemia or leukemia. Such information is important for correct diagnosis and treatment for many diseases.
Of course, deciphering the data from a general blood test and making a diagnosis is a matter for the doctor. However, patients themselves should also have an understanding of what information the study contains. An increased or, conversely, low level of hemoglobin, leukocytes, erythrocytes and other components in the blood is also an indicator of the presence or absence of inflammatory processes, various infectious or chronic diseases. However, the task of deciphering the analysis by a doctor will be significantly more complicated if, in the process of taking diagnostic material in the laboratory, the analysis methodology was violated. Unfortunately, the capillary method of taking blood does not always make it possible to obtain a high-quality sample for research.
This is due, first of all, to the composition of the material itself. Thus, capillary blood has a lower concentration of calcium, potassium and total protein, but a higher concentration of glucose and hemoglobin. Also, the blood may be diluted with excess interstitial fluid, which may cause inaccurate test results. Microclumps may appear in the material under study, reducing the reliability of the data. When taking capillary blood, residual antiseptic (alcohol) and tissue fluid may also get into the sample, which significantly reduces the quality of the sample and affects the accuracy of the laboratory test. In this case, a repeat analysis will be required.
Blood from a vein
A more accurate diagnostic method today is a venous blood test. It is indispensable, for example, when conducting a biochemical blood test, showing whether the cardiovascular system, liver, kidneys, pancreas, and muscles are functioning properly. Thus, the first indicator of blood biochemistry is albumin protein - it is determined for the diagnosis of renal, rheumatic, oncological diseases, and liver pathologies. The term “total protein” refers to the total content of albumin and globulins in the blood serum - this indicator is a key indicator of protein metabolism in the body. This is important information for a diagnostician - as is known, with an excess of cholesterol, plaques form on the walls of blood vessels and the risk of developing cardiovascular diseases increases. Blood biochemistry also allows you to find out the glucose level - a parameter indicating the possible presence of diabetes mellitus. Typically, about 30 parameters are examined in a biochemical blood test, and the resulting detailed information makes this analysis one of the most objective criteria of human health. This is why it is so important to correctly take and store material for analysis.
Venous blood analysis is carried out in two main ways - open and closed. Traditionally, Russian healthcare facilities use an open method, in which a nurse draws blood from a vein with a syringe, hollow needle, or gravity flow into a test tube. This technique is outdated: with open blood collection technology, the risk of destruction of blood cells when it is transferred to a test tube increases. The optimal option for obtaining blood for research today is the so-called closed method using vacuum systems consisting of a vacuum tube, holder and needle. The test tube allows you to collect the required volume of blood, and the needle with a special silicone coating easily penetrates the skin without causing pain. This procedure is safe for both the patient and the medical professional collecting blood for testing.
After this procedure, the blood will be securely stored in a test tube, specially dosed with the required amount of reagent, which increases the chance of obtaining the most accurate test result. It is also worth remembering that, for preventive purposes, it is recommended to conduct a blood test at intervals once a year: in this case, the attending physician will have the opportunity to notice changes in the patient’s health status in time and prescribe treatment at an early stage of the disease.
- Back
What changes should you be wary of?
The first thing you should pay attention to is the color change from cycle to cycle. The shade of the discharge should not change. For example, if a woman has always had red periods, and then they become very dark, almost black, this is a reason to be examined by a gynecologist.
Alarming symptoms when color changes are:
- intense pain in the lower abdomen;
- pain when emptying the bladder;
- frequent urination;
- violation of cycle duration;
- burning and itching;
- unpleasant (putrid) odor;
- pain radiating to the anus;
- fever, chills, weakness, dizziness.
The above symptoms may indicate the presence of an inflammatory process. Also, the reason for consulting a doctor is the appearance of discharge between periods, regardless of its shade.
Scarlet blood during menstruation
The onset of menstruation may be accompanied by bright red discharge. This indicates an increased rate of discharge. The shade may not change during menstruation or become darker towards the end. The reason for this manifestation may be:
- infection. Infectious diseases provoke discharge between menstruation. They may have a scarlet color as they are caused by bleeding. In this case, you should urgently seek advice from a gynecologist;
- pregnancy. Scarlet smears during pregnancy (as well as smears of other colors) pose a serious health threat. This may indicate a threat of miscarriage. Require immediate medical attention;
- fibroids, polyps. Non-cancerous formations in the uterus provoke scarlet discharge both during menstruation and during other periods. Characteristic symptoms are pain and a feeling of pressure.
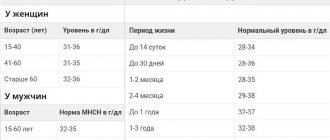
Detailed description of the study
An extended blood test is a primary study that is used to assess the general condition of the body, identify a wide range of diseases and monitor their treatment.
The main indicators that are included in the extended clinical blood test:
Erythrocytes are cells also called red blood cells. The main function of red blood cells is to transport oxygen to tissues and remove carbon dioxide (CO2) from them.
Hemoglobin is the main protein in red blood cells. It directly allows for gas exchange in tissues by combining with oxygen, or CO2. Insufficiency of hemoglobin in the body, along with a decrease in red blood cells, serves as the basis for the development of anemia.
Hematocrit is the ratio of all formed elements of blood (mainly red blood cells) to the liquid component of blood. Allows you to judge the excess or deficiency of red blood cells, dehydration or overhydration of the body.
The color indicator reflects how adequately the saturation of erythrocytes with hemoglobin is, helps the specialist to establish anemia and differentiate it into normochromic, hypochromic or hyperchromic.
MCH (Mean Cell Hemoglobin) - an indicator reflecting the average hemoglobin content in red blood cells, is a modern and more accurate analogue of the color indicator.
MCV (Mean Cell volume) determines the average volume of a red blood cell. Used in conjunction with MCH to identify anemia and its causes.
RDW (Red cell Distribution Width) reflects the heterogeneity of red blood cells by volume. The indicator is also important in the diagnosis of anemia; it depends on the mean erythrocyte volume (MCV), therefore, when MCV increases or decreases, its increase is observed, which indicates that there are cells of different volumes in the blood.
MCHC (Mean Cell Hemoglobin Concentration) helps estimate the mean hemoglobin concentration in red blood cells. Changes in the indicator are observed in cases of impaired hemoglobin synthesis, hypochromic and hyperchromic anemia.
Platelets also belong to the formed elements of blood; they play a key role in the processes of hemostasis and ensure timely blood clotting in case of vascular damage. Changes in this indicator may be associated with impaired cell production in the bone marrow or their accelerated destruction.
Leukocytes are called white blood cells. They participate in various immune processes and protect the body from infection. There are several types of leukocytes: eosinophils, neutrophils, lymphocytes, basophils, monocytes. Their percentage ratio allows you to evaluate the leukocyte formula to understand the current state of the immune system, identify and determine the severity of inflammatory and allergic processes in the body.
Neutrophils , the largest population of white blood cells, are aimed at fighting foreign microorganisms - including bacterial infections - in the body.
Lymphocytes play an important role in recognizing pathogenic microorganisms and forming and regulating immunity to various infections by releasing antibodies and destroying infected cells.
Monocytes are white blood cells that can differentiate into macrophages and dendritic cells after they migrate to peripheral tissues. Viral and bacterial particles are absorbed, then target proteins appear on the surface of the cell to recognize the infectious agent by the immune system. This helps in fighting pathogens and building adaptive immunity. Monocytes also take part in cleansing the body of dead cells and tissue healing.
Basophils and eosinophils are actively involved in the development of allergic reactions. They contain many granules with bioactive molecules that cause allergy symptoms. Eosinophils also play a role in protecting the body from parasites.
Reticulocytes serve as precursors of red blood cells. Their number reflects erythropoiesis - the rate of formation of red blood cells in the bone marrow. This indicator is important when assessing the effectiveness of anemia therapy. Additionally, the percentage of reticulocytes, the content of their immature forms and the production index of these cells are determined. Taken together, these data are used to manage patients with hematopoietic disorders.
Taken together, the indicators of an extended clinical blood test are necessary for the doctor as a stage of primary laboratory diagnosis of a wide range of diseases. The test can also be used to assess general health.
Pink color of blood
This shade is characteristic of the beginning or end of menstrual bleeding. Most often they occur in women, who often experience spotting symptoms. Light pink smears may indicate a combination of cervical fluid and blood. Discoloration can also be caused by:
- decreased estrogen. This hormone is responsible for normalizing the mucous membrane of the female genital organs. With a lack of estrogen, particles of the mucous membrane mix with the blood and change color. Its level is affected by taking hormonal drugs and menopause;
- ovulation. Bloody smears may occur in the middle of the cycle.
Interpretation of the analysis for determining blood sugar levels
Murzaeva Irina Yurievna
Endocrinologist, Preventive Medicine Doctor
July 19, 2011
It seems like nothing special, just an ordinary analysis, you say. But its interpretation has many nuances, I will describe everything in order.
The first thing that matters is where the analysis comes from
- from a vein (this is plasma sugar level)
- from a finger (capillary blood)
- glucometer (can show both the venous rate and the capillary rate).
In a vein, the sugar rate is always higher, by 11%, approximately, than from a finger. For example, the norm of fasting blood sugar in a vein is from 3.1 mmol/l to 6.1 mmol . This indicator may also depend on the reagent that the laboratory purchased (that is, the norm may be 6.2 mmol, 6.4 mmol). And the norm of capillary blood on an empty stomach is up to 5.6 mmol .
The glucometer rate always depends on the type of glucometer, pay attention! read the instructions, where you will find a link to the standards for your device.
The glucometer is not used in people with anemia (anemia), the indicator will initially be incorrect.
Secondly, when was the analysis taken?
On an empty stomach (on an empty stomach), an hour after a meal, 2 hours after a meal, and so on. As a standard, blood sugar is taken on an empty stomach and, if necessary, 2 hours after a meal (and not after 1 hour, 15 minutes, etc.  ).
).
When testing with 75 gr. glucose (sugar curve) - the test is taken on an empty stomach, after 1 hour and after 2 hours, the doctor will warn you about this in advance.
Third, how was the analysis taken?
On an empty stomach - this is after an 8-hour fast (and not when you ate at 2 o’clock at night and took the test at 7 am). It is not advisable if the test is taken after drinking alcohol, feasting, against the background of fever, taking prednisolone and its analogues, or intense physical activity.
Pregnant women and newborns have their own blood sugar standards, while for others they are the same. (does not mean patients with different types of diabetes!).
Glucometers often include a table for calculating sugar levels, like in Oun Tuch Ultra).
In Russia, blood sugar standards are calculated based on capillary indicators. This is why “imported glucometers” are not very suitable for us.
In addition, there is a difference between the concepts of determining blood sugar and blood glucose, but in Russia these concepts are inseparable.
Important! Message from the site administration about questions on the blog:
Dear readers! By creating this blog, we set ourselves the goal of giving people information on endocrine problems, diagnostic methods and treatment. And also on related issues: nutrition, physical activity, lifestyle. Its main function is educational.
Within the framework of the blog, in answering questions, we cannot provide full-fledged medical consultations; this is due to both the lack of information about the patient and the doctor’s time spent in order to study each case. But we understand that not everywhere it is possible to consult with an endocrinologist at your place of residence; sometimes it is important to get another medical opinion. For such situations, when a deeper dive and study of medical documents is needed, at our center we have a format for paid correspondence consultations on medical documentation.
How to do it? Our center’s price list includes a correspondence consultation on medical documentation, costing 1,000 rubles. you can send scans of medical documents, a video recording, a detailed description, everything that you consider necessary regarding your problem and questions to which you want answers. The doctor will see if the information provided can give a full conclusion and recommendations. If yes, we will send the details, you will pay, and the doctor will send a report. If, based on the documents provided, it is impossible to give an answer that could be considered as a doctor’s consultation, we will send a letter stating that in this case, absentee recommendations or conclusions are impossible, and, of course, we will not take payment.
Sincerely, Administration of the Medical
Brown color of blood during menstruation
If red-brown discharge occurs in the first and last days of menstruation, this is normal. The blood mixes with vaginal secretions and comes out slowly, having time to oxidize. Brown drops can be noticed for several days after menstruation. If brown discharge is present throughout menstruation or occurs on other days of the cycle, this may indicate:
- hormonal imbalance;
- diseases of the endocrine system;
- metabolic failure;
- weak immunity;
- recovery after childbirth or abortion;
- stress.
References
- Nazarenko, G.I., Kishkun, A.A. Clinical evaluation of laboratory results. - M.: Medicine, 2006. - 544 p.
- Tatkov, O.V., Stupin, F.P. General blood analysis. Information collection. - M.: Publishing solutions, 2021. - 72 p.
- Fauci, A., Braunwald, E., Kasper, D. et al. Harrison's principles of internal medicine, 17th edition, 2009.
- Pagana, K., Pagana, T., Pagana, Th. Mosby's Diagnostic and Laboratory Test Reference. 14th Edition. Elsevier Publishing Hall, 2019. - 1094 p.
Orange period blood
The likely cause of such changes is mixing of blood with cervical fluid. In addition, such changes can cause:
- implantation. During the implantation period (approximately the second week after conception), spotting may be observed, and not all pregnant women experience orange discharge;
- infection. Abnormally colored discharge during menstruation may be caused by sexually transmitted infections.