Classification of dyscirculatory encephalopathy ICD 10
The "I60-69" group collected cerebrovascular diseases. The International Classification of Diseases, Tenth Revision (ICD10) does not use the term “dyscirculatory encephalopathy.” Codes have been developed to describe various syndromes that occur with damage to blood vessels of various etiologies. Asymptomatic forms are designated "I65-66".
ICD codes for 10 types of dyscirculatory disorders of the brain:
- Chronic cerebral ischemia (I67.8) – develops over a long period of time, accompanied by progressive changes in the blood circulation of the brain;
- Hypertensive encephalopathy (I67.4) – pathology of intracerebral microcirculation in patients with hypertension;
- Vascular leukoencephalopathy (Binswanger syndrome) - pathological changes in the white matter against the background of amyloid angiopathy, arterial hypotension.
Brain MRI, electroencephalography, and Doppler ultrasound help determine the type of blood supply disorder.
Forms of the disease
Taking into account the nature of the course, symptoms, and anatomical damage, experts have identified the following forms of hypertensive encephalopathy:
- Subcortical arteriosclerotic.
- Multi-infarction.
Subcortical arteriosclerotic encephalopathy tends to manifest itself between the ages of 55 and 70, when the atherosclerotic process reaches high activity. The patient is concerned about the following signs:
- slowing down the pace of movements;
- memory loss;
- speech problems;
- inability to walk independently;
- orientation disorder;
- loss of appetite, vomiting;
- dysfunction of the pelvic organs;
- inability to concentrate;
- apathy, lack of emotions.
But most often doctors hear complaints about:
- hand tremors;
- headache;
- insomnia;
- swallowing disorder.
Lack of therapy is dangerous due to the development of mental retardation (dementia) after 5–10 years. Phases of improvement and stabilization of the condition are periodically observed. Various areas of the white matter of the brain are affected. Lacunar infarctions are observed in the optic thalamus, cerebellum, and pons. There is also swelling of the brain tissue.
The course of multi-infarct encephalopathy is more favorable. Patients do not experience complete dementia. Patients with this form of pathology complain of:
- difficulty speaking;
- swallowing disorder (variable);
- visual impairment, hearing impairment;
- muscle cramps;
- inability to perform movements with the hands;
- numbness of different parts of the body;
- weakness of the muscles of the arms and legs;
- headaches, dizziness.
The difference from subcortical encephalopathy is the presence of multiple areas of infarction at different depths of the intracerebral arteries. After such lesions, cavities and multiple cysts with a diameter of 0.1 - 1.5 cm are formed. At the same time, doctors record the most predisposing conditions for hemorrhagic stroke.
Please note: Hypertension is considered the most common disease of the cardiovascular system (it affects about 20 - 30% of adults. With age, the percentage of patients increases, approaching 50 - 65%).
Causes of dyscirculatory encephalopathy
Pathology develops mainly in older people against the background of the following conditions:
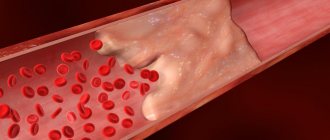
- Deposition of blood clots inside a vein, artery;
- Angiospasm with a significant increase in blood pressure;
- Atherosclerosis of the cerebral arteries;
- Cholesterol plaques inside the vessel wall;
- Damage to the vascular wall by bacterial toxins (botulism, streptococci);
- Degenerative-dystrophic diseases of the cervical spine;
- Vegetative-vascular dystonia (VSD);
- Inflammatory processes of the arterial wall (vasculitis).
To predict clinical symptoms, it is rational to divide etiological factors into five categories:
- Venous;
- Hypertensive;
- Atherosclerotic;
- Neurological (VSD, rheumatism);
- Mixed.
The most common causes of nosology in older people are hypertension, atherosclerosis, and varicose veins.
Clinical picture
Symptoms of the disease appear against the background of high blood pressure numbers (diastolic more than 120 mm Hg). Symptoms of hypertensive encephalopathy arise and develop within several minutes, hours and are manifested by diffuse headache (90%), nausea, vomiting (60–70%). Possible disturbance of consciousness, flickering before the eyes and blurred vision (40%), visual hallucinations. 1/4 of patients may have generalized or partial epileptic seizures, psychomotor agitation. An objective examination of the patient reveals changes in consciousness, cerebral syndrome, convulsive syndrome, photopsia, scotoma, nystagmus, dissociation of tendon reflexes in the upper and lower extremities, and emotional-volitional disorders.
Symptoms of dyscirculatory encephalopathy
Let us describe the main symptoms of all forms of DEP:
- Disorders of the functioning of the cerebellum - fluency of speech, walking disorders, instability during movements;
- Affective disorders;
- Vascular dementia;
- Pyramidal spasticity;
- Pseudobulbar problems;
- Slow speech;
- Autonomic vestibular disorders;
- Instability of blood pressure;
- Smoothness and slowness of speech.
It is difficult to unambiguously determine the symptoms of dyscirculatory encephalopathy, since the manifestations are based on functional disorders of cerebral circulation.
The main signs of alcoholic encephalopathy:
- Decreased memory for short-term events;
- Mental and emotional disorders;
- Apathy, lack of interest in favorite activities;
- Severe headaches;
- Weakness and dizziness;
- Vomiting reflex;
- Dizziness;
- Multiple sclerosis;
- Neurological focal symptoms.
Discirculatory encephalopathy is characterized by the appearance of symptoms closer to the night. In the first degree, initial symptoms occur after heavy physical activity:
- Unsteady walking;
- Decreased memory;
- Pathology of attention;
- Fall of self-criticism;
- Depressive syndrome;
- Dementia;
- Muscle tremors;
- Urinary incontinence;
- Pseudobulbar syndrome;
- Irritability;
- Ataxia.
The appearance of any sign requires MRI or CT angiography to verify changes in cerebral circulation.
Arterial hypertension (AH) occupies one of the leading places in the structure of morbidity and mortality. According to WHO, hypertension affects from 20 to 40% of the population of developed countries. Russia is one of the countries with a very high prevalence of hypertension: in the mid-1990s. this figure was 39.9% among men and 41.1% among women [1]. The results of monitoring the epidemiological situation with hypertension, carried out within the framework of the targeted federal program “Prevention, diagnosis and treatment of hypertension in Russia”, showed that over the past 10 years the situation has remained virtually unchanged: in 2004, the prevalence of hypertension was still 36.9% among men and 42% among women [2]. In addition, the results of the work demonstrate an increase in the prevalence of hypertension with age: after 60 years it reaches 60%, and after 80 it approaches 80%. In 95% of cases we are talking about essential hypertension, while symptomatic hypertension is detected only in 5% of patients. Factors influencing the development of hypertension are presented in the table.
. Factors influencing the development of hypertension.
Considering the external and internal factors responsible for the development of hypertension, it is possible to formulate directions for preventive and therapeutic effects on both hypertension and its complications. Impact on external factors is possible only if the patient is motivated to fight hypertension. Unfortunately, the ability and desire of patients, especially men, to change their lifestyle to eliminate the main external factors influencing hypertension is extremely low [3]. Both in Russia and in the world, the number of patients who control blood pressure (BP) is small: but if in France, Greece, Germany, Spain and the USA the target blood pressure level is achieved in 30.0–35.7% of patients with hypertension, then in In Canada, the Czech Republic, Poland, India and Russia, this value does not exceed 9–16% [4].
There are many reasons for low adherence of patients to antihypertensive therapy: • poor tolerability of antihypertensive drugs; • low discipline of patients; • high cost of medicines; • psychological factors (reluctance to take medications for life); • lack of awareness about the complications of hypertension and the purposes of taking medications; • existing cognitive deficit – memory loss (patients forget to take medication), absent-mindedness (irregularity of taking medications), decreased criticism of their condition; • antihypertensive drugs do not eliminate many neurological symptoms (dizziness, headache, unsteadiness when walking, anxiety, irritability) characteristic of brain damage in hypertension.
Systematic violations of antihypertensive therapy or refusal of it lead to a decrease in the effectiveness of treatment and worsening hypertension with the development of complications from target organs [5].
As a result of hypertension, damage occurs to the heart, blood vessels, kidneys, and brain. One of the most dangerous complications of hypertension is acute cerebrovascular accident. Both new and repeated strokes are the direct cause of death of the patient in 57% of cases in the early stages and in 14% in the long-term period [6]. Also very acute in modern neurology is the issue of chronic brain damage due to hypertension, in particular hypertensive encephalopathy (HE). This term dates back to the late 1950s. by the staff of the Institute of Neurology G.A. Maksudov. and Schmidt E.V. and is defined as a steadily progressive lesion of the brain substance, which is associated with a poorly controlled increase in blood pressure, leading to chronic cerebral ischemia.
Among the risk factors for the development of GE are the following: uncontrolled hypertension, hypertensive crises, high blood pressure variability, high nocturnal hypertension, excessive decrease in blood pressure, including iatrogenic ones [7].
Three stages can be distinguished during GE. At stage I, the clinic is dominated by subjective disorders in the form of general weakness and fatigue, emotional lability, sleep disturbances, decreased memory and attention, and headaches. Neurological symptoms are not formed by distinct neurological syndromes, but are represented by anisoreflexia, discoordination, and symptoms of oral automatism. Violations of memory, praxis and gnosis can, as a rule, be identified only when special tests are carried out.
At stage II, there are more subjective complaints, and neurological symptoms can already be divided into distinct syndromes (pyramidal, discoordination, amyostatic, dysmnestic), with one neurological syndrome usually dominating. Professional and social adaptation of patients decreases. At stage III, neurological symptoms increase, a distinct pseudobulbar syndrome appears, and sometimes paroxysmal conditions (including epileptic seizures); Severe cognitive impairment leads to disruption of social and everyday adaptation and complete loss of working capacity. Thus, GE ultimately leads to the formation of vascular dementia, and its subcortical variant is often formed [18].
In stages II and III of GE, diffuse changes in the brain substance are usually combined with focal lesions in the form of lacunar infarcts - small cavities ranging in size from 0.1 to 1.0 cm, formed in areas of cerebral ischemia. In the structure of cerebrovascular diseases, there is an increase in the proportion of lacunar strokes: among all cases of stroke in hypertension they account for 15%. It is possible either asymptomatic development of lacunar infarction, if the foci are located in functionally silent areas, or the formation of a transient ischemic attack, stroke. Lacunar infarcts are localized in the basal ganglia, internal capsule, thalamus, pons, cerebellum and white matter of the hemispheres. The formation of multiple small-focal brain lesions - lacunar state - significantly worsens the prognosis of the course of GE and reduces the possibility of drug improvement of the patient's condition - even when good control of hypertension is achieved. In addition, lacunar strokes are risk factors for the development of hemorrhagic stroke and vascular dementia [19].
With hypertension, the following pathomorphological changes occur in the vessels of the brain: plasmatic and hemorrhagic impregnation, necrosis of the vascular wall with its subsequent thinning, adaptive thickening of the walls of extracerebral vessels. In GE, early damage to the predominantly white matter of the brain is observed, which is the destruction of the myelin of the central conductors, which has a typical picture in computed tomography (decreased signal intensity) and magnetic resonance imaging (increased signal intensity) [8]. Characteristic changes are usually detected in areas of the terminal blood supply that are particularly sensitive to fluctuations in blood pressure, i.e., in the periventricular areas of the brain, and are called leukoaraiosis [9, 10]. With uncontrolled hypertension, the described processes in the white matter progress, the phenomenon of corticocortical disconnection develops (conductive fibers are localized in the white matter), intellectual-mnestic functions are disrupted, and ultimately vascular dementia is formed (“subcortical arteriolosclerotic encephalopathy”, or Binswanger’s disease). The ARIC study showed that such changes in the white matter of the brain occur in the group of patients with hypertension 2 times more often than in normotensive patients, and in patients with uncontrolled hypertension compared to patients with adequate control of hypertension - 1.5 times more often. Often such changes occur without clinical symptoms. The duration of the asymptomatic phase may vary and is determined by the presence of other risk factors [11].
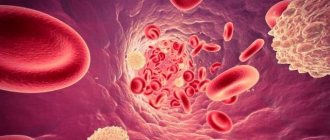
With hypertension, atherosclerosis rapidly progresses. The structural and functional properties of erythrocytes and platelets are disrupted - their ability to deform worsens, hematocrit increases, blood viscosity increases, which in turn leads to disruption of microcirculation. Pathomorphological, as well as isolated clinical studies of the cerebral venous system in hypertension indicate severe disturbances, including obliteration of the cerebral venous sinuses. In this case, they speak of encephalopathy of mixed origin: hypertensive and atherosclerotic [12, 13].
An important consequence of changes in the structure of the vascular wall is a violation of the autoregulation of cerebral circulation - the ability to maintain stable blood flow when the average systemic blood pressure fluctuates from 60 to 150-170 mm Hg. Art. [14]. Experimental data indicate that autoregulation disorders are primarily observed in the white matter of the brain and, to a lesser extent, in the cerebral cortex [15]. As a result, hypoxia develops, caused by a discrepancy between the tissue need for oxygen and its delivery.
At the initial stage of oxygen starvation in mitochondria, the rate of aerobic oxidation and oxidative phosphorylation decreases, which leads to a decrease in protein synthesis and gene expression, a decrease in the amount of adenosine triphosphate (ATP), and an increase in the content of adenosine diphosphate (ADP) and adenosine monophosphate. With a further decrease in cerebral blood flow, the enzyme phosphofructokinase is activated, anaerobic glycolysis is enhanced, and then the final transition to anaerobic respiration occurs, which adapts the cell to hypoxia, but glycogen reserves are depleted. This, in turn, entails the accumulation of under-oxidized lactate with the development of lactic acidosis. At the same time, the activity of lactate dehydrogenase increases and the activity of succinate dehydrogenase, which supplies electrons to the respiratory chain of mitochondria, decreases, which indicates a disruption in the processes of energy formation in the ischemic brain. Under such conditions, anaerobic glycolysis does not occur, which leads to severe energy deficiency. Ultimately, destabilization of cell membranes occurs, disruption of ion channels, damage to the potassium-sodium pump, which leads to cell hyperhydration, cloudy swelling, and then to balloon degeneration. The most important role in this process belongs to glutamate receptors.
Oxidative stress, closely associated with the ischemic cascade, occurs when glutamate receptors are excited and consists of excessive accumulation of free radicals, activation of lipid peroxidation and excessive intracellular accumulation of their products. The reactions of oxidative stress and the ischemic cascade interact and potentiate each other.
Free radicals are highly reactive forms of oxygen, hydrogen peroxide, and aldehydes formed under hypoxic conditions. Under their influence, the functional properties of a number of enzymes, carbohydrates, proteins, including DNA and RNA, change; as a result, the cell loses its functions, abnormal proteins appear and secondary destructive processes are stimulated [16–18].
Along with the processes of free radical oxidation, stable antioxidant radicals or antioxidants are produced in biological objects. The mechanism of their action is based on inhibition of free radical processes in tissues, which inhibits the development of destructive changes and inactivates oxidative stress reactions. Changes in the structure and function of substrates under conditions of ischemia and stress depend on the ratio of the activity of free radicals and antioxidants.
The body has a physiological antioxidant system that maintains oxidative-antioxidant balance both in liquid media (blood, lymph, intracellular and intercellular fluid) and in the structural elements of the cell (plasmic, endoplasmic, mitochondrial, cell membranes). Enzymatic antioxidants include: superoxide dismutase, catalase, glutathione dehydroascorbate reductase, and some other peroxidases.
Non-enzymatic antioxidants include vitamins C, E, K, glucose, ubiquinones, phenylalanine, transferrin, haptoglobin, tryptophan, ceruloplasmin, carotenoids. Biological and chemically synthesized antioxidants are divided into fat- and water-soluble. The former are localized where the target substrates for attack by free radicals and peroxides are located, the biological structures most vulnerable to peroxidation processes, which include primarily biological membranes and blood lipoproteins (their main targets are unsaturated fatty acids). The most significant fat-soluble antioxidant is α-tocopherol. Among the water-soluble antioxidants, the most important are glutathione and the ascorbic acid system, which are especially significant for the antioxidant protection of the brain [21, 22].
At all stages of GE, to the treatment of the underlying disease - hypertension - it is necessary to add drugs that improve cerebral blood flow and metabolism of nervous tissue, as well as those acting on internal factors that can affect the progression of encephalopathy. In order to prevent the increase in the atherosclerotic process, it is necessary to normalize fat metabolism: reducing body mass index, low-fat diet, prescribing statins (simvastatin, pravastatin). In order to improve the rheological properties of blood, antiplatelet agents (acetylsalicylic acid, ticlopedine, clopidogrel, dipyridamole) are indicated. The CAPRIE and ESPS-2 studies showed that the use of acetylsalicylic acid, clopidogrel and dipyridamole reduces the risk of developing cerebral ischemia [20]. At all stages of GE, the use of drugs that act on the vascular wall, improve the metabolism of brain tissue and have neuroprotective properties is mandatory.
Based on the pathogenetic role of hypoxia and oxidative stress, the use of antioxidants, which are specific correctors of brain energy metabolism, is considered as one of the most promising methods of treating chronic forms of cerebral circulatory disorders, including HE.
Currently, α-tocopherol, ascorbic acid, methionine, cerulloplasmin, carotene, ubiquinone, and emoxypine are used in clinical practice. However, the disadvantage of these drugs is the need for long-term use (several weeks) to ultimately achieve weak antioxidant and antihypoxic effects. This provided the prerequisites for the creation of more effective drugs with antioxidant properties, among which Mexidol® occupies a prominent place [19].
Mexidol is a derivative of 3-hydroxypyridine, which belongs to the water-soluble antioxidants of the biogenic type and is a structural analogue of compounds of the vitamin B6 group. An important property of this drug is its ability to penetrate the blood-brain barrier. The drug Mexidol (2-ethyl6-methyl-3-hydroxypyridine succinate) was created on the basis of emoxypine with the inclusion of succinic acid in its molecule.
In recent years, the effect of succinic acid, its salts and esters, which are universal intracellular metabolites, has been widely studied. Succinic acid is found in all tissues and organs. Performing a catalytic function in relation to the Krebs cycle, this compound reduces the concentration of other products of the cycle in the blood - lactate, pyruvate, citrate, produced and accumulated in the early stages of hypoxia, and is thereby included in energy metabolism, directing the oxidation process along the most economical path. The Roberts cycle functions in nervous tissue, during which succinic acid is formed from γ-aminobutyric acid (GABA) through the intermediate stage of succinic aldehyde. The formation of succinic acid is also possible under conditions of hypoxia and oxidative stress in the reaction of oxidative deamination of α-ketaglutaric acid in the liver. The antioxidant effect of succinic acid is associated with its effect on the transport of mediator amino acids, as well as with an increase in the content of aminobutyric acid in the brain due to the Roberts shunt. Succinic acid in the body normalizes the content of inflammatory mediators histamine and serotonin, increases microcirculation in organs and tissues, primarily in the brain, without affecting blood pressure and heart function. The antihypoxic effect of succinic acid is associated with the activation of succinate dehydrogenase oxidation and restoration of the activity of cytochrome oxidase, the key redox enzyme of the respiratory chain.
Accordingly, based on the chemical formula, Mexidol is an antioxidant, membrane protector, antihypoxant with direct energizing action, inhibiting free radicals, reducing the activation of lipid peroxidation, increasing the activity of its own physiological antioxidant system, activating the energy-synthesizing functions of mitochondria and improving energy metabolism in the cell. Mexidol has a modulating effect on membrane-bound enzymes, ion channels, receptor complexes, including GABA and acetylcholine, improves synaptic transmission in brain structures, correcting disorders in microcirculatory systems. Mexidol acts under conditions of ischemia and hypoxia as a specific trap of free radicals, reducing their damaging effect on cerebral structures [23]. The drug is prescribed in doses of 200 to 500 mg 2-4 times a day intravenously in a stream or drip with saline or intramuscularly. The maximum daily dose is 1200 mg. Then it is possible to switch to the tablet form of administration. Mexidol tablet contains 125 mg of ethylmethylhydroxypyridine succinate; The drug is prescribed orally at 125–250 mg 3 times a day. Treatment begins with a dose of 125–250 mg 1–2 times a day with a gradual increase until a therapeutic effect is obtained. The duration of treatment is usually 2–6 weeks. Treatment is stopped gradually, reducing the dose over 2-3 days.
In patients with HE, long-term planned therapy with antioxidants significantly improves the quality of life and helps prevent the progression of functional-morphological cerebral disorders. Early therapy with antioxidants is currently considered as a pathogenetically determined method for correcting cerebral metabolism in hypertensive encephalopathy.
GE is a severe progressive disease that forms a variety of neurological syndromes, threatens the development of strokes and leads to vascular dementia. Timely treatment can preserve the patient’s professional, social and everyday adaptation for many years, and improves the prognosis for the patient’s life expectancy.
Degrees of dyscirculatory encephalopathy
The stages of DEP determine the clinical picture of the disease:
- First (I) degree – memory loss appears;
- Second (II) degree – personality changes occur, self-criticism decreases;
- Third (III) degree – several syndromes exist simultaneously, the ability to self-care is lost.
Stage 1 DEP is common among the population. Medical sources claim that every second resident has a nosology. Cerebral circulation disorders (dyscirculation) develop due to constant stress and air pollution.
Discirculatory encephalopathy of the 2nd degree occurs in old age. The development of nosology provokes cerebral infarctions and strokes. Depending on the symptoms, several clinical variants of the nosology are formed:
- Social maladjustment;
- Movement disorders;
- Polyneuropathy.
One of the common types of the disease is atherosclerotic dyscirculation. An imbalance of fat metabolism causes disturbances in the patency of cerebral arteries due to the presence of atherosclerotic plaques inside the lumen.
Venous discirculatory encephalopathy occurs due to stagnation of venous blood in the body. Congestion of the veins ensures the formation of blood clots. Migration of blood clots from the primary focus into the cerebral vessels provokes a stroke.
Classification
The disease is characterized by a gradual worsening of degenerative processes and progression of manifestations. Severity matters when determining optimal treatment methods, therefore in clinical practice there are 3 stages of pathology:
- First. It is characterized by a predominance of nonspecific subjective complaints of cephalgia, inattention, increased fatigue, and memory impairment. During a special examination, a slight decrease in cognitive functions is determined.
- Second. Subcortical, dysmnestic, ataxic, pyramidal and vestibular symptoms are revealed. As a rule, there is a predominance of one, or less often, two syndromes. Cognitive abilities are moderately impaired. Problems arise in social adaptation and professional activity.
- Third. Neurological symptoms increase and become more diverse. Sometimes secondary parkinsonism, symptomatic epilepsy, and pseudobulbar syndrome are detected. Cognitive disorders worsen, reaching the level of dementia. The ability to work is lost, the ability to self-care is limited.
Diagnosis of dyscirculatory encephalopathy
Primary assessment of the structure of the brain parenchyma and the nature of blood flow is carried out by clinical and instrumental methods:
- Computed tomography (CT with contrast);
- Positron emission tomography (PET);
- Magnetic resonance imaging (MRI);
- Electroencephalography (EEG);
- X-ray of the cervical spine;
- Blood chemistry.
The degree of dyscirculatory encephalopathy is determined by analyzing the symptoms. It is necessary to take into account the lack of self-criticism in the second and third forms of the disease.
Neuropsychological counseling is required for patients with suspected mental disorders.
Treatment
Efficacy largely depends on successful normalization of blood pressure. As part of symptomatic treatment, measures are taken to improve intracerebral circulation, stimulate local metabolism, and restore brain functions. Pharmacological support includes:
- Vasodilators. Phosphodiesterase inhibitors and calcium channel blockers eliminate arteriolar spasm.
- Means for improving microcirculation. Pentoxifylline and long courses of anticoagulants are recommended.
- Neuroprotectors. Glycine, gamma-aminobutyric acid and antioxidants increase cell resistance to hypoxia and lack of nutritional compounds.
- Other medicines. They are selected taking into account current symptoms and laboratory test data. It may be necessary to prescribe statins, nootropics, tranquilizers, antidepressants, and anticonvulsants.