Biomaterial: Feces
Completion time (in the laboratory): 1 working day.
* The website indicates the maximum possible period for completing the study. It reflects the time it takes to complete the study in the laboratory and does not include the time for delivery of the biomaterial to the laboratory. The information provided is for reference only and is not a public offer. For up-to-date information, contact the Contractor's medical center or call center.
Nomenclature of the Ministry of Health of the Russian Federation (Order No. 804n): A09.19.001.001 “Rapid examination of feces for occult blood using the immunochromatographic method”
Description
A stool examination aimed at identifying hidden bleeding from parts of the gastrointestinal tract can also be used to screen for colorectal cancer.
Allows you to detect the presence of hemoglobin and haptohemoglobin complex in stool even in cases where visually the color of stool is unchanged, and red blood cells are not detected during microscopic examination of stool. Bleeding from the gastrointestinal tract is one of the common problems faced by practicing physicians of all specialties, but the greatest danger is posed by small “hidden” bleedings that cannot be detected without a special study, and often these small bleedings are markers of including intestinal cancer in apparently healthy people.
The ColonView study is carried out using an immunochemical method, which significantly increases sensitivity, and unlike other tests (gavaiac and benzidine), which is specific exclusively to human hemoglobin, which means it does not require adherence to a strict diet, refusal of meat products, some vegetables and fruits that contain large amounts of ascorbic acid, catalase and peroxidase (for example, cucumbers, cauliflower, use of horseradish seasonings).
Why is analysis needed and what does it give?
| During an annual medical examination, persons over 40 years of age are recommended to undergo a fecal occult blood test. The analysis reveals gastrointestinal pathologies in the early stages, which makes it possible to use it as a screening method. Any inflammation, polyp or tumor of the intestine is accompanied by bleeding, but the amount of blood is so small that it cannot be determined visually. However, this amount is sufficient to determine blood contamination using a laboratory method. |
There are two methods for determining occult blood in stool:
- benzidine (guaiac test)
- shows an admixture of any hemoglobin in the stool. Therefore, the method gives a number of errors in the absence of preparation in the form of a special diet three days before the test;
- immunochemical method
is the most accurate. It shows the presence of human hemoglobin, and not what comes from food. The method does not require special preparation. The disadvantage of the immunochemical method is the long readiness period, about 14 days.
Indications for use
- As a preventive examination for persons over 50 years of age.
- Diagnosis of pathology of the digestive tract, accompanied by hidden bleeding: colon polyps, colon diverticula, ulcerative colitis, Crohn's disease.
- Screening for colorectal cancer.
- Infestation by helminths that injure the intestinal wall.
- Rendu-Osler disease with localization of bleeding telangiectasias on the mucous membrane of the gastrointestinal tract.
- Typhoid fever, diagnosis of necrotizing enterocolitis.
- As a differential diagnosis of anemia.
- As a preventive examination for persons over 50 years of age.
- Diagnosis of necrotizing enterocolitis.
Hidden blood in feces, quantitatively (FOB Gold method)
An immunological method for the quantitative determination of hemoglobin in stool, which allows the diagnosis of minor occult bleeding from the lower gastrointestinal tract.
Synonyms Russian
Hidden blood in feces (quantitative immunochemical method).
English synonyms
FOB Gold Test, Immunological faecal occult blood test (iFOBT).
Research method
Immunochemical method.
Units
ng/ml (nanograms per milliliter).
What biomaterial can be used for research?
Cal.
How to properly prepare for research?
- Avoid taking laxatives, administering rectal suppositories, oils, limit taking medications that affect intestinal motility (belladonna, pilocarpine, etc.) 72 hours before stool collection.
- The study should be carried out before performing sigmoidoscopy and other diagnostic procedures in the area of the intestines and stomach or at least 2 weeks after such.
General information about the study
Colorectal cancer is one of the most common types of tumors, both in terms of incidence and mortality. It ranks second in mortality among malignant neoplasms in men and women. Every year there are more than 1 million new cases of the disease worldwide, and the annual death rate exceeds 500,000. The risk of developing the disease increases with age, 90% of those affected are over 55 years of age. According to epidemiological data, heredity is the cause of the development of colorectal cancer in 5-30% of patients. Hereditary syndromes that significantly increase your risk of developing it include familial adenomatous polyposis, Lynch syndrome, juvenile polyposis, and some rarer conditions. A patient's 5-year survival rate depends on the stage of the cancer at the time of diagnosis.
Colorectal cancer develops slowly over several years. The tumor often occurs as a result of the transformation of a polyp of the intestinal mucosa. This process can take from 8 to 12 years. Not all types of polyps can turn into tumors, but their presence, especially in large quantities, significantly increases the risk of developing colorectal cancer. Other precancerous conditions include dysplasia, which is typical for people with ulcerative colitis and Crohn's disease.
With colorectal cancer, blood can be released in the stool long before the first symptoms of the disease. Screening examination of feces for occult blood among people at risk helps to diagnose the disease in a timely manner and reduce mortality from colorectal cancer by 15-33%. The effectiveness of such screening has been confirmed by several studies.
To detect hidden blood in stool, guaiac or benzidine tests are most often used, but they require strict adherence to certain rules, in particular following a diet several days before the test. In addition, unlike the guaiac test, modern immunochemical methods are highly sensitive and specific.
The fecal occult blood (FOB) immunoassay test has been proven to be the most convenient test method due to its ease and effectiveness in patient management. It allows you to accurately determine the amount of hemoglobin (Hb) in the stool, without requiring patients to follow a diet or change their lifestyle. The method is based on an antigen-antibody agglutination reaction between the human hemoglobin present in the sample and the anti-hemoglobin antibody on latex particles. Agglutination is measured as an increase at absorbance of 570 nm, the unit of which is proportional to the amount of human hemoglobin in the sample. The study determines hidden blood that has entered the intestinal lumen in the lower parts of the gastrointestinal tract, since hemoglobin from the upper parts is destroyed when passing through the digestive tract.
A positive test result requires further examination to clarify the reasons, since the source of minor blood loss may be a benign polyp, diverticulum, hemorrhoids, or inflammatory bowel disease. On average, 1-5% of people test positive for occult blood, of which 2-10% are diagnosed with cancer, and 20-30% are diagnosed with adenomatous polyps of the colon. If occult blood is positive, further testing is done to look for cancer, a polyp, or another cause of bleeding. To confirm the diagnosis, patients in the absence of contraindications are prescribed colonoscopy, sigmoidoscopy or double contrast radiography. The absence of blood in the stool does not completely exclude the possibility of colorectal cancer, so endoscopy is recommended for people at high risk (with a family history), even if the test result is negative.
What is the research used for?
- For screening for colon and rectal cancer.
- For the diagnosis of bleeding from the lower gastrointestinal tract in certain benign and inflammatory diseases (colon polyps, Crohn's disease, ulcerative colitis, hemorrhoids).
When is the study scheduled?
- During a preventive annual examination of persons aged 50-75 years.
- If you suspect hidden intestinal bleeding.
What do the results mean?
Reference values: 0 - 50 ng/ml.
A positive result indicates minor bleeding from the lower gastrointestinal tract. To clarify the cause of bleeding, endoscopic diagnostic methods (sigmoidoscopy, colonoscopy) are necessary.
Possible reasons for a positive result:
- colon or rectal cancer,
- polyps and adenomas of the large intestine,
- inflammatory diseases of the large intestine (Crohn's disease, ulcerative colitis),
- intestinal diverticulosis,
- haemorrhoids.
A negative result cannot completely exclude the possibility of colorectal cancer.
What can influence the result?
- Damage to the intestinal mucosa during medical procedures (colonoscopy, sigmoidoscopy, enemas) performed several days before the study can lead to false-positive results.
Important Notes
- The sample must be collected from three different areas.
- The study is not recommended to be carried out within two weeks after colonoscopy, sigmoidoscopy, and cleansing enemas.
Also recommended
- CA 72-4
- CA 242
- Tumor Marker 2 (TM 2) – pyruvate kinase
- Carcinoembryonic antigen (CEA)
- Fecal occult blood test
- General laboratory screening (oncological)
- Predisposition to colorectal cancer
Who orders the study?
Gastroenterologist, proctologist, surgeon, therapist, oncologist.
Literature
- European guidelines for quality assurance in colorectal cancer screening and diagnosis: overview and introduction to the full supplement publication. Endoscopy 2013 Jan;45(1):51-9.
- Haug U, Hundt S, Brenner H. Quantitative immunochemical fecal occult blood testing for colorectal adenoma detection: evaluation in the target population of screening and comparison with qualitative tests. Am J Gastroenterol. Mar 2010; 105(3):682-90.
- Levi Z, Rozen P, et al. A quantitative immunochemical fecal occult blood test for colorectal neoplasia. Ann Intern Med. 2007 Feb 20;146(4):244-55.
Preparing for the study
The stool is collected in a sterile, disposable container. When preparing a patient for the study, alcohol and NSAID drugs (non-steroidal anti-inflammatory drugs - ortofen, indomethacin, etc.) acetylsalicylic acid, warfarin (and other anicoagulants), corticosteroid drugs reserpine, phenylbutazone should be discontinued 2 days in advance.
To obtain reliable results, samples should not be used in patients during menstruation, as well as during rectal bleeding due to hemorrhoids or constipation.
You cannot examine stool obtained after an enema and taking laxatives, as well as X-ray examination of the stomach and intestines using contrast agents.
When is a referral for analysis issued?
In addition to screening the age group over forty years, the doctor writes a referral for this test in the following cases:
|
The analysis reveals the slightest damage to the walls of the intestine. If an admixture of blood higher than normal is detected in the stool, the test is repeated and, if the result is confirmed, the patient is sent to see a proctologist or gastroenterologist.
Interpretation of results/Information for specialists
NEGATIVE RESULT
Hemoglobin and haptohemoglobin complex – NOT DETECTED
Absence of hemoglobin and haptohemoglobin complex in the stool sample is normal
A false negative result is also possible against the background of an occasionally bleeding polyp (neoplasm) and in the absence of bleeding at the moment.
IMPORTANT: a negative test result does not completely exclude intestinal pathology, for example, in the case of episodic bleeding of a polyp. In this case, it is possible to recommend repeated examinations (at least three times) at intervals determined by the attending physician, and to use instrumental diagnostic methods for final verification of the diagnosis.
Detailed description of the study
Iron is a trace element involved in many vital processes in the body. In its free form it has a toxic effect on tissues, so it circulates in the blood in combination with proteins. Iron enters the body with food, mainly meat products and some cereals. It is absorbed in the small intestine and from there enters the blood, where it combines with the carrier protein - transferrin.
The main amount of the microelement in combination with transferrin is transferred to the bone marrow. Here, iron is included in the hemoglobin inside red blood cells. Its function is to deliver oxygen to tissues. When red blood cells are destroyed, iron is released from them and again forms a compound with transferrin. The trace element is then sent to the bone marrow. This way it circulates in the body.
Some of the iron is used by the cells of internal organs for the synthesis of enzymes. Transferrin transports iron to the liver, kidneys, and muscles, where it is deposited in the form of ferritin. This form is the main reserve of the microelement.
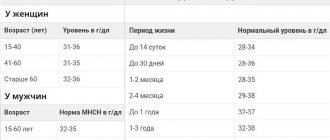
Iron deficiency can negatively affect human health. This condition occurs against the background of insufficient intake of the microelement from food, impaired absorption in the intestines, increased consumption of its reserves - during the growth period in children, pregnancy and breastfeeding in women - or loss due to bleeding. With small losses of iron in the absence of compensation, latent, or hidden, iron deficiency is observed. In this case, there may be no disturbance in health, and the content of hemoglobin and red blood cells remains normal.
If iron levels continue to decrease, iron deficiency anemia develops. IDA is a condition in which hemoglobin synthesis is disrupted and oxygen delivery to cells is impaired. Symptoms of anemia include weakness, dizziness, and increased heart rate. Also characterized by pale skin, brittle hair and nails, inflammatory diseases of the oral cavity, changes in the senses of taste and smell.
To prevent these disorders, timely detection of iron deficiency in the body is necessary. Transferrin is one of the indicators that allows one to diagnose insufficient levels of a microelement even in the absence of iron deficiency anemia, that is, at the stage of latent iron deficiency. The less iron there is in the body, the more carrier protein molecules there will be in the blood; accordingly, the concentration of transferrin increases.
Not only a lack of iron, but also its excess leads to disturbances in the body. In this case, in a biochemical analysis, the level of transferrin in the blood serum will be reduced, which indicates an excess of iron in the tissues.
Excessive levels of microelements in the body are observed much less frequently than deficiency. This condition may be associated with mutations in genes responsible for iron metabolism. This disease is called primary hemochromatosis. Acquired, or secondary, hemochromatosis is also distinguished due to multiple blood transfusions, alcohol abuse, and hematological diseases. Symptoms appear slowly, predominantly in adulthood with feelings of weakness, joint pain, loss of weight and loss of appetite. Further developments occur: skin pigmentation, liver damage and diabetes mellitus.
Determining the amount of transferrin in the blood together with other indicators of iron saturation in the body makes it possible to diagnose iron metabolism disorders and prescribe treatment in a timely manner.