Increased aggregation is a marker of hyperaggregation syndrome and thrombophilia. The most commonly used are the Born turbidimetric method, based on recording changes in the light transmission of platelet-rich plasma, and the method for studying platelet aggregation, based on the analysis of light transmission fluctuations caused by a random change in the number of particles in the optical channel.
Material for research.
Citrate platelet rich plasma
Research method
is determined by the operating procedure on a particular type of aggregometer.
Solutions of ADP, ristocetin, collagen, adrenaline, and arachidonic acid are most often used as inducers. Solutions of thrombin, serotonin, etc. can also be used.
Platelet aggregation with ADP
Exposure to small doses of ADP (usually 1*10-7 mol) leads to the formation of a double wave of aggregation. The first phase (primary wave) depends on added exogenous ADP, and the second phase (secondary aggregation wave) occurs due to the release reaction of intrinsic agonists contained in platelet granules. Large doses of ADP (usually 1*10-5 mol) lead to the merging of the first and second waves of aggregation.
When analyzing aggregograms, attention is paid to the general nature of aggregation (single-wave, two-wave; complete, incomplete; reversible, irreversible) and the rate of aggregation. The appearance of two-wave aggregation upon stimulation of ADP at concentrations that normally cause reversible aggregation (usually 1-5 µmol) indicates an increase in platelet sensitivity, and the development of single-wave incomplete (and often reversible) aggregation upon stimulation of ADP at concentrations of 10 µmol or more indicates an increase in platelet sensitivity. impaired platelet release reaction.
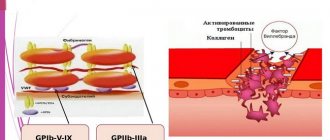
Platelet aggregation with ristocetin
Determination of platelet aggregation with ristocetin in plasma is used to quantify von Willebrand factor. The method is based on the ability of ristocetin to stimulate in vitro the interaction of von Willebrand factor with platelet glycoprotein Ib. In most cases of von Willebrand disease, there is a violation of ristocetin aggregation with a normal response to the effects of ADP, collagen and adrenaline. Disturbances in ristocetin aggregation are also detected in Bernard-Soulier disease. For differentiation, a test with the addition of normal plasma is used: in von Willebrand disease, after the addition of normal plasma, ristocetin aggregation is normalized, while in Bernard-Soulier syndrome this does not happen. Ristocetin-induced platelet agglutination is reduced in most cases of von Willebrand disease, except type IIB.
References
- Clinical laboratory diagnostics, National guidelines, Volume 1, Dolgov V.V., Menshikov V.V., 2012, pp. 761-765
- Kozlovsky V. I., Kovtun O. M., Seroukhova O. P., Detkovskaya I. N., Kozlovsky I. V. Research methods and clinical significance of platelet aggregation. Focus on spontaneous aggregation // Vestnik VSMU. 2013. No. 4.
- Puri RN, Colman RW.ADP-induced platelet activation.Crit Rev BiochemMol Biol. 1997;32(6):437-502. doi: 10.3109/10409239709082000. PMID: 9444477.
- "Clinical and laboratory diagnosis of platelet function disorders." Vasiliev S.A., Berkovsky A.L., Melkumyan A.L., Suvorov A.V., Mazurov A.V., Kozlov A.A. Federal State Budgetary Institution Hematological Research Center, Ministry of Health of the Russian Federation, Moscow, 2013.
Platelet aggregation with collagen
Platelet aggregation with collagen has a fairly pronounced latent phase, during which phospholipase C is activated. Depending on the concentration of the reagent used, the duration of this phase can be 5-7 minutes. After the end of this period, processes occur in platelets that lead to the formation of second messengers, as a result of which the secretion of platelet granules and the synthesis of thromboxane A2 develop, which is accompanied by a sharp increase in interplatelet interaction.
In laboratory and clinical practice, collagen is most often used in a final concentration of 50 μg/ml, however, collagens from different companies may have different activities, which must be taken into account when using them.
What are platelets?
These elements are formed in the bone marrow and are small, round, irregularly shaped plates that lack nuclei. The function of these particles is very important: they are involved in the process of blood clotting and regeneration of damaged tissue, that is, they help prevent large blood losses in the event of vascular damage. The cells live for no more than 10 days, after which they are destroyed in the spleen and liver, and they are replaced by new ones.
The platelet count changes throughout the day. They are increased during physical activity. During pregnancy and menstruation, their number, on the contrary, decreases. Such changes are considered natural, and platelet levels return to normal at rest, at the end of menstruation, or after childbirth.
In other cases, deviations from the norm in any direction indicate some kind of pathology. A condition in which platelets are elevated is called thrombocytosis, and if they are low, it is called thrombocytopenia.
Platelet aggregation with adrenaline
Adrenaline, upon contact with platelets, interacts with α2-adrenergic receptors, which causes inhibition of adenylate cyclase. It is possible that the mechanism underlying the implementation of the effect of adrenaline and the development of the first wave of aggregation does not depend on the formation of thromboxane A2, the release reaction or the synthesis of platelet aggregation factor, but is associated with the ability of adrenaline to directly change the permeability of the cell membrane to calcium ions. The second wave of aggregation occurs as a result of the release reaction and production of thromboxane A2.
Testing for PLT in children
Monitoring blood composition, including PLT levels, is especially important in childhood. If this indicator drops below normal, the following diseases can be assumed:
- allergic reactions to medications;
- intoxication;
- thyrotoxicosis;
- blood diseases;
- parasitic and viral infections.
The causes of elevated PLT levels in children are varied. There are primary and secondary thrombocytosis. The first is due to the fact that brain stem cells produce an excess amount of platelets with an altered structure, which, for example, is observed in leukemia.
Secondary, or reactive, develops as a result of some pathological process, which disrupts the production of these cells, as well as their structure and shape. Factors in the development of reactive thrombocytosis include:
- heavy operations;
- splenectomy;
- sudden bleeding;
- osteomyelitis;
- anemia;
- fractures of tubular bones;
- pulmonary infections;
- malignant diseases;
- some drugs.
Video about the functions of platelets and the reasons for changes in their number in the blood:
Platelet aggregation with arachidonic acid
Arachidonic acid is a natural aggregation agonist, and its action is mediated by the effects of prostaglandins G2 and H2, thromboxane A2, and includes activation of both phospholipase C with subsequent formation of second messengers, mobilization of intracellular calcium and expansion of the cell activation process, and phospholipase A2, which directly leads to release of endogenous arachidonic acid. Platelet aggregation with arachidonic acid occurs quite quickly, so the curve characterizing this process is often single-wave in nature.
To induce aggregation of blood platelets, arachidonic acid is used in concentrations of 10-3-10-4 mol. When working with arachidonic acid, it should be taken into account that in air this substance oxidizes very quickly.
An aggregation test with arachidonic acid is recommended in cases of using drugs that affect the aggregation reaction (for example, acetylsalicylic acid, penicillin, indomethacin, delagil, diuretics), which must be taken into account when assessing the research results.
Platelet aggregation
To assess platelet function, CIR Laboratories LLC performs an analysis for induced platelet aggregation. This is a high-quality analysis performed on an automatic aggregometer.
To assess platelet function, the CIR Laboratory performs an analysis for induced platelet aggregation. This is a high-quality analysis performed on an automatic aggregometer. Since this test changes dramatically when taking drugs that affect blood clotting (antiplatelet agents, for example, aspirin, thromboass, anticoagulants, for example, heparin), it is advisable to take it before starting to take these drugs. For each aggregogram, the laboratory doctor issues a conclusion.
A platelet aggregation test is recommended in the following cases: miscarriage, unsuccessful IVF attempts, a history of severe pregnancy complications, infertility of unknown origin, as well as increased bleeding: easy bruising, menorrhagia, nosebleeds.
The aggregation curve evaluates the amplitude of aggregation, the shape of the curve, the presence of one or two waves, and the presence of disaggregation.
The sample shown shows: 1—zeroing of the device, 2—before adding the inductor, 3—peak associated with dilution of the sample by the inductor, 4—reference point, first wave, 5—second wave, 6—disaggregation.
Important information: the combination of taking foods, herbal medicines and nutritional supplements containing components from this list with taking antiplatelet agents (thromboASS) and anticoagulants (heparin) is a dangerous combination due to the risk of bleeding (category D according to the FDA classification). The risk of bleeding in most cases outweighs the potential benefit.
More details At CJSC Laboratories CIR, platelet aggregation is performed with the following inducers:
- Aggregation with ADP
- Aggregation with arachidonic acid
- Aggregation with adrenaline (epinephrine)
- Aggregation with ristocetin. The first three inducers make it possible to evaluate the function of platelets from different sides; they complement each other. Aggregation with ristocetin allows one to suspect a dangerous bleeding condition - von Willebrand disease (von Willebrand factor deficiency). When planning a pregnancy, this analysis is important to eliminate the risk of bleeding during childbirth.
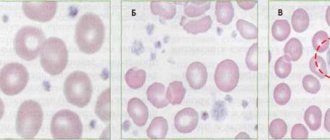
Aggregation with ADP (blue line) and arachidonic acid.
The aggregation response is sharply reduced. There is virtually no disaggregation.
Aggregation with ADP.
The aggregation response is reduced. There is virtually no disaggregation.
Platelet aggregation when taking NSAIDs
(aspirin has the maximum effect)
Aggregation with arachidonic acid. There is no aggregation response. A common situation when taking non-steroidal anti-inflammatory drugs
Also, platelet aggregation with ADP and adrenaline may decrease.
Aggregation with ADP, response reduced. Partial disaggregation.
Aggregation with ristocetin, the aggregation response is sharply reduced.
The analysis is given in Maryino on weekdays and Saturdays from 9.00 to 11.00, on Tretyakovskaya and Voykovskaya on weekdays from 8.00 to 10.00.
What medications affect platelet aggregation?
| Pathogenetic mechanism | The way to realize the impact | Drugs |
| Inhibitors of thromboxane A2 formation | ||
| Phospholipase inhibitors | Prevents the formation of arachidonic acid, inhibits collagen, ADP and adrenaline aggregation | Quinacarpine, high-dose corticosteroids |
| COX inhibitors | Acythelate platelet and COX membranes, block the formation of prostacyclin in the endothelium, inhibiting aggregation and release reactions. Against the background of drugs that block COX, arachidonic acid levels are sharply reduced. | PVP (aspirin, indomethacin, butadione, ibuprofen, sulpirazone), indocid, fenoprofen |
| Thromboxane synthetase inhibitors | They block the synthesis of thromboxane A2 without affecting the synthesis of prostacyclin. Inhibits aggregation under the influence of arachidonic acid | Prostacyclin and its synthetic analogues, imidazole and its derivatives (individual sensitivity) |
| Competitive antagonists of thromboxane A2 | Block thromboxane receptors and inhibit aggregation. Inhibits aggregation under the influence of arachidonic acid | 1,3-Azoprostanoic acid and its derivatives |
| Drugs that increase cAMP levels in platelets | ||
| Adenylate cyclase stimulators | They block the synthesis of thromboxane A2 without affecting the synthesis of prostacyclin. Inhibits aggregation under the influence of arachidonic acid. | Prostacyclin, PGE, diterpene foscolin |
| Phosphodiesterase inhibitors | Prevents cAMP degradation. Inhibit platelet adhesion to the subendothelium, the second wave of aggregation, disrupt the release reaction | Dipyridamole, papaverine, aminophylline, intensain |
| Stimulators of prostacyclin synthesis | They enhance the synthesis of prostacyclin, its release from the endothelium, and weaken its degradation | Anabolic steroids, nicotinic acid, vasopressin |
| Drugs that interfere with calcium transport | ||
| Suppress the second wave of aggregation | Isoptin, nifedipine | |
| Impairs the adhesive-aggregation function of platelets | Furosemide in high concentrations | |
| Disrupts the initial and second wave of ADP-collagen- and adrenaline-platelet aggregation | Nitrofurantoin, aminazine, imipramine, amitriptyline, antihistamines, α- and β-blockers, high (over 20 million units/day) doses of penicillin, carbenicillin | |
| Drugs of different groups | ||
| Anticoagulants | In high concentrations they reduce aggregation | Pelentan, warfarin |
| Dextrans | Reduce platelet aggregation | Reopoliglyukin |
| Anesthetics | Reduce ADP aggregation | Nitrous oxide, cyclopropane, phenobarbital |
| Alcohol | Reduces collagen and ADP aggregation | |
| Antiplatelet agents | Reduce all types of aggregation, significantly enhance the effect of prostacyclin, disrupt the connection between platelets and fibrinogen | Tiklid |
Presentation “Platelet aggregation”
- what is platelet aggregation
- What are platelet granules and what do they contain?
- what platelet activators are there in a living organism and what does the laboratory use?
- requirements for conducting research
- factors affecting platelet aggregation
- interpretation of aggregograms
Assessment of platelet aggregation and pregnancy planning What are you taking?
Effect of drugs on platelet aggregation The use of four inducers in the analysis of platelet aggregation, APS, gene polymorphism Reduced aggregation, polymorphism of hemostasis genes, coagulogram Why take platelet aggregation before pregnancy? Aggregation cost Tags:
Aggregation, ADP, platelets, von Willebrand disease, aspirin
Back to section