Blood is the most important matter of the body, performing regulatory, nutritional, excretory, respiratory and other functions.
50% of blood consists of plasma. This is a multicomponent liquid that includes trace elements, enzymes and hormones. The other 50% belongs to blood cells, each of which has its own unique role.
Any disease, be it inflammatory, oncological, autoimmune or metabolic, affects the qualitative and quantitative composition of the blood. And therefore, the diagnosis of diseases begins with the appointment of a general blood test.
When should you take a Reticulocyte (capillary blood) test?
- Assessment of erythropoiesis after bleeding or hemolysis;
- Assessing the ability of bone marrow to regenerate after taking cytotoxic drugs and/or bone marrow transplantation;
- Assessing the resumption of erythropoietin production after kidney transplantation;
- Doping control (for athletes when using erythropoietin);
- Diagnosis of various anemias;
- Assessment of bone marrow function in case of insufficient amounts of vitamin B12, iron, folate, copper and quality control of treatment.
Reasons for the increase
An increase in the number of immature cells does not always clearly indicate pathology. Although such cases are common in clinical practice, the diseases themselves account for no more than 60% of the total.
However, to be on the safe side, doctors initially believe that the deviation is of pathological origin. This presumption helps to look at things soberly.
What are the possible reasons for the increase in the indicator:
- Reticulocytes: what are they? normal blood levels, reasons for increase and decrease
- Light bleeding. They are especially common in patients with pathologies of the digestive tract: stomach ulcers, Crohn's disease, damage to the large intestine and others. In this case, the blood output is small. But it happens regularly. Anemic changes begin. Red blood cells simply do not have time to mature. Therefore, the body compensates for the deficiency with what is easier to synthesize. As a rule, in this case the predecessor is not much larger than under normal conditions. But if the bleeding intensifies, the situation changes radically.
- Acute infectious conditions. Malaria is considered a classic disease in this regard. She is a rather rare visitor to Europe, but anything is possible. Other septic disorders manifest themselves in the same way. Regardless of the provocateur: whether it is a bacterium, a virus or a fungus. The essence is always the same. After correcting the pathological process, it is possible to quickly take control of the situation.
- Severe bleeding. If you measure the reticulocyte count immediately, it will be significantly lower than normal. However, after a few days, about 3-4 days, the level will increase sharply. The deviation reaches truly shocking proportions: the number of cells increases hundreds of times. These are convulsive attempts by the body to restore at least part of the red blood cells, temporarily compensate for their deficiency and ensure gas exchange.
- Reticulocytes are always elevated in advanced forms of iron deficiency anemia. A sharp jump in the reticulocyte index occurs 3-5 days after the start of treatment.
The body begins to intensively synthesize red blood cells, but the work of the bone marrow is not yet so effective. Everything returns to normal in a week or a little more. Typically, this phenomenon is not considered dangerous. Although control over laboratory parameters is still necessary.
These pathological processes provoke sharp increases in the number of immature red cell precursors. If the level rapidly jumps, the concentration increases hundreds of times, we are talking about a reticulocyte crisis.
Usually the condition is natural and does not pose a threat to health or life. But this is very indicative from the point of view of diagnosis and control of the treatment. For example, a sharp increase when using vitamins and iron supplements indicates the effectiveness of the correction. This means that anemia is treatable.
There are other pathologies in which the number of reticulocytes increases. Although not as significant as during crises:
- Tumors. If cancer metastases reach the bone marrow. The levels of progenitor cells in this case vary greatly. The larger the secondary focus, the more serious the situation.
- All hypoxic and ischemic processes provoke reticulocytosis. The mechanism of development of the disorder is approximately the same. The body signals the bone marrow to produce “transport cells” faster. It is easiest to synthesize structures that are immature but have similar functions. What, in fact, is what the body does. Once ischemia is eliminated, hematopoiesis returns to normal.
- Use of certain medications. There are quite a lot of such drugs. This includes anti-inflammatory, antipyretic, and antiseptics for internal use. It is very difficult to provide a list of specific means. Because there are hundreds of titles. It is best to read the annotation. The manufacturer indicates such points in the instructions.
- Systemic destruction of red blood cells. It develops for various reasons. Up to radiation sickness or some infectious pathologies. As soon as the number of dead cells reaches at least 30%, an active compensatory process begins and reticulocytes in the blood increase significantly. This is a dangerous condition. Not because the rate of precursor cells is growing, but because of the destruction of their mature forms. Provoking factors are usually threatening. We need to fight the culprit as quickly as possible.
When the level of reticulocytes is elevated, there is often some pathological process. If no anomalies are detected, natural factors are also possible:
- Heavy drinking.
- Excessive physical overload.
- Peak hormonal conditions or disruptions. From puberty to pregnancy and temporary “problems.”
There are more options. If the cause is natural, reticulocyte counts increase slightly.
In some cases the growth is false. A similar condition is said to occur when the number of cells increases only in the blood, but remains normal in the bone marrow.
In such cases, extensive diagnostics and testing are not always necessary. Only in exceptional, complex clinical situations.
Detailed description of the study
Reticulocytes are young red blood cells (erythrocytes). Reticulocytes are formed in the bone marrow from normoblasts that have lost their nucleus. It takes several days to ripen, usually 4-5. The maturation process begins in the bone marrow and then continues in the peripheral blood. The formation of red blood cells and their forms depends on the hormone erythropoietin, which is produced in the kidneys.
Reticulocytes are larger in size than red blood cells. The internal environment of the cell contains a basophilic network (reticulum), which is located in the form of threads and small grains. An important difference between reticulocytes and mature erythrocytes is their inability to fully transport oxygen and carbon dioxide, since the cells still do not have enough hemoglobin.
There are 5 different stages of maturity of young red blood cells:
- They have a core, the grain is located around the core in the shape of a corolla;
- Granular-mesh mass, which is represented by a ball;
- The grain size is represented by a dense network;
- Mass, which is represented by threads;
- There are individual grains.
It is important to note that about 80% of young forms belong to group 4-5.
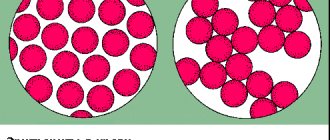
In a healthy person, 0.2-1% of reticulocytes are determined in the blood. The percentage is calculated from the total number of red blood cells. With increased destruction of red blood cells (hemolysis) or bleeding, the number of immature forms will increase, so it is important to use the “reticular index” to assess the severity of anemia. Such a small concentration shows that young forms are able to exit into the peripheral blood and can then mature and turn into mature erythrocytes.
In infants in the first days after birth, the concentration of reticulocytes is higher than in an adult; they can be 10%. Gradually their number will decrease. Also, an increased number of young forms is observed due to the destruction of red blood cells with negative Rh factors of the mother and child. In case of blood loss or insufficient intake of iron from food, the concentration is also higher than normal, as the body independently tries to restore the level of red blood cells. There are conditions and/or diseases in which a decrease in the concentration of reticulocytes is observed. This can be due to damage to the bone marrow (after ionizing radiation, chemotherapy treatment or tumor damage), which leads to a decrease in the formation of reticulocytes and, as a consequence, a decrease in their number in the peripheral blood.
There are true and false reticulocytosis - an increase in the concentration of young forms. True is characterized by an increase in the number of immature red blood cells both in the peripheral blood and in the bone marrow. And if false, there will be an increased concentration of reticulocytes in the circulating blood and no increase in the bone marrow. This fact indicates the “washing out” of immature red blood cells from the bone marrow into the blood.
The concentration increases with accelerated erythropoiesis, and decreases with its slowdown. Erythropoiesis is the process of hematopoiesis during which red blood cells are formed. Determination of reticulocytes in capillary blood shows that the bone marrow is capable of regeneration and evaluates the hematopoietic system.
Reasons for the decline
There are also many culprits for the decline in the indicator. The following violations are especially common:
- Vitamin B12 or folic acid deficiency. With persistent deficiency, megaloblastic anemia develops. The condition leads to a rapid change in the process of hematopoiesis, and the development of red blood cells stops at the level of the erythroblast. Further, the degradation reaches such a wide scale that even the predecessors become less and less functional.
The body “releases into the wild” barely differentiated cells - megaloblasts. Of course, they can't do their job. Ischemic processes begin, which only worsens the situation. The vicious circle can be broken if the root cause is eliminated.
- Thyroid gland activity disorders. When the organ produces little T3, T4 substances, or the work of a small structure is not sufficiently stimulated by the pituitary TSH. There may be several options. The more active the pathological process, the more serious the violation in laboratory tests.
- Excessive consumption of alcohol. Dependent patients are more prone to developing hematopoietic disorders. The disorder also occurs in relatively healthy people who like to drink. Even if it's just one episode, the reticulocyte count will drop.
- Infectious inflammations of a chronic nature. Over a long period of time, they cause compensatory reactions of the body. In particular, this one. When the body, instead of ensuring the maturation of red blood cells, takes the easy way out. Because it is necessary to fight the outbreak and contain the infection. Even after treatment, the indicators do not return to normal immediately. It takes from several weeks to a couple of months. With the participation of a hematologist, the time frame becomes shorter.
- Autoimmune inflammation. Caused by disruption of one's own defenses. May be primary or secondary. Regardless of this, the reticulocyte count always decreases.
- Radiation sickness or simply an effect on the body of this kind. Occurs in the treatment of cancer. Especially if the doses are large. The bone marrow responds extremely poorly to such stimulation. Irradiation is harmful to sensitive functional cells. The synthesis and rate of maturation of all structures, not just red blood cells, temporarily decreases.
- Chemotherapy. Reticulocytes are reduced as a result of drug suppression of their production, because drugs for cancer treatment reduce the proliferative activity of “fast” structures. Including those that make up hair, nails, immune barriers, etc. This is a side effect from which it is impossible to protect yourself. Sometimes, if the dosage is small, reticulocytes remain normal.
- Endocrine disorders. The leader of this group is diabetes mellitus. Especially when the kidneys are involved. The more advanced the pathological process, the worse the state of hematopoiesis. Irreversible damage is possible if treatment is not carried out on time.
- Poisoning with certain toxic components and substances. Arsenic, mercury, lead and other elements have destructive potential. It is especially noticeable in relation to bone marrow.
The reasons mentioned are just the tip of the iceberg. There are many more violations. A decrease in reticulocyte levels is a small fragment of the overall picture.
Important Notes
Material for research Capillary blood.
Children under 7 years of age: venous blood/capillary blood (for special indications). Children over 7 years of age and adults: venous blood. Capillary blood collection for research is carried out only for children under 7 years of age (for special indications)! According to GOST R 53079.4-2008, indications for taking capillary blood are possible: in newborns, in patients with very small or hard-to-reach veins, with large-area burns, and in severely obese patients.
What indicators are included in the UAC?
The general blood test includes the following indicators: red blood cells, hemoglobin, leukocytes, color index, hematocrit, reticulocytes, platelets, ESR.
The leukocyte formula in some laboratories is signed by default, in some a doctor’s note is required. It includes the following indicators: eosinophils, basophils, band and segmented neutrophils, lymphocytes, monocytes.
Below is a table of norms for a general blood test:
| Index | Laboratory designation | Norma (women) | Norma (men) | Unit |
| Red blood cells | R.B.C. | 3,8-4,5 | 4,4-5,0 | 1012/l |
| Hemoglobin | HGB | 120-140 | 130-160 | g/l |
| Leukocytes | WBC | 4,0-9,0 | 4,0-9,0 | 109/l |
| Color index | CPU | 0,8-1,0 | 0,8-1,0 | |
| Hematocrit | HCT | 35-45 | 39-49 | % |
| Reticulocytes | RET | 0,2-1,2 | 0,2-1,2 | % |
| Platelets | PLT | 170,0-320,0 | 180,0-320,0 | 109/l |
| ESR | ESR | 2-15 | 1-10 | mm/hour |
| Leukocyte formula: | ||||
| Basophils | BAS | 0-1 | 0-1 | % |
| Eosinophils | EO | 0,5-5 | 0,5-5 | % |
| Myelocytes | 0 | 0 | % | |
| Metamyelocytes | 0 | 0 | % | |
| Band neutrophils | NEUT | 1-6 | 1-6 | % |
| Segmented neutrophils | NEUT | 47-67 | 47-67 | % |
| Lymphocytes | LYM | 18-40 | 18-40 | % |
| Monocytes | MON | 3-11 | 3-11 | % |
At some points, the standard blood test for adults differs from that for children.
For example, the norm of hemoglobin in a child is 110-145 g/l, leukocytes 5.0-12.0 109/l, the content of lymphocytes can be in the range of 26-60%. The remaining blood test parameters correspond to the reference values for adults.
By order of the Ministry of Health, in the first year of life, a child’s blood is taken for general analysis 4 times, then at 1 year 6 months, and then annually, starting from two years. Such measures are necessary for the early detection of blood diseases, anemia, and infections.
Reticulonocytes during pregnancy
Pregnant women typically have a slight increase in reticulonocyte counts. The fact is that in expectant mothers the total blood volume increases and this happens not due to blood cells, but due to plasma. In the “liquid” blood of pregnant women, the level of hemoglobin is reduced, anemia develops, and therefore the process of hematopoiesis is activated. A slight increase in the level of reticulonocytes is considered normal and indicates physiological adaptation, although ideally the number of these cells does not increase during gestation.
What they are and what functions they perform
These are nuclear-free cells of a pinkish color with a bluish tint. Microscopic examination reveals intracellular structures that are not found in red blood cells. These are thread-like and granular formations: mitochondria, RNA remnants, and other organelles.
Reticulocytes perform the same functions as red blood cells, that is, they carry oxygen, but less efficiently.
How is it carried out?
Determination of the level of reticulonocytes is not included in the clinical blood test and is prescribed additionally if indicated. Their number is calculated by microscopic examination of a blood smear. The essence of the method is to identify cells with granular-mesh substances, which are visible when stained with special alkaline dyes.
To test for reticulocytes, blood is taken from a finger prick
This is the simplest, most accessible and low-cost method still used in laboratories, although it is less accurate than automatic counting. For analysis you need a dye (three different types are used), a microscope, a test tube or glass. Today, ready-made reagents are used, for example, the Diagem kit. The coloring on glass and in a test tube are different.
On glass
The glass is washed, dried and heated using a burner. A drop of one of the three dyes is applied to the glass using a glass rod and a stroke of paint is made using a grinding glass. A drop of blood is applied to a smear of paint and a thin stroke is made. For 5-10 minutes, place the glass in a damp chamber (usually a Petri dish, along the edges of which rolls of moistened cotton wool are placed). The smears are then air dried.
In vitro
Dyeing is done in different ways, depending on the type of dye. In general, the procedure involves placing paint in a test tube, adding a drop of blood to it and mixing. The mixture is left for some time (from 20 minutes to 3 hours depending on the reagent used), then mixed again and smears are made.
Count
The finished smears are examined under a microscope. Red blood cells and reticulocytes have a yellowish-greenish color, the granular structure of reticulocytes is blue or bluish-violet. Counted cells are expressed in ppm or percentage.
View of reticulocytes on glass in a smear after staining
For example: a smear revealed 20 cells with a granular-mesh structure per 1000 red blood cells. That is, the reticulocyte content is 20 ppm or 2 percent.