An increase in pressure in the blood vessels can lead to the formation of trophic ulcers. Varicose veins can be complicated by thrombosis and thrombophlebitis - a condition when blood clots (thrombi) form inside the veins, interfering with the free movement of blood throughout the body. The most dangerous consequence, even death, is considered to be thromboembolism - the separation of a blood clot, as a result of which the clot clogs the artery of the pulmonary circulation.
When the first symptoms of varicose veins appear (swelling and heaviness in the legs, the appearance of spider veins, dilated veins in the legs), you should consult a phlebologist. This will allow you to timely identify the essence of the problem - by performing an ultrasound of the veins, begin treatment and prevent complications.
What are varicose veins?
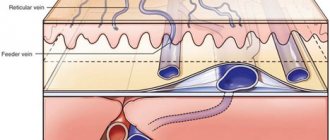
This is a deformation and disruption of the normal functioning of the veins in the legs. In a normal state, blood in the veins moves from bottom to top; this is achieved due to contractions of the heart, the coordinated work of the elastic walls of the vessel, the muscles around the vessel and the valve in the vein. This valve allows blood to flow upward and prevents it from flowing in the opposite direction. When there is a violation, the vessel walls expand, the valve gap diverges, and the blood can partially move in the opposite direction, creating a counterflow, expanding the vessel walls even more and weakening the valve. Varicose veins appear. The disease is extremely common among people over 30 years of age, with women most often affected.
Causes of the disease.
Factors contributing to the development of the disease:
- Sedentary work or work “on your feet”
- Overweight
- Heredity, predisposition to disease
- Age and gender. The greatest likelihood of developing varicose veins in women is 30-40 years old.
- Pregnancy.
The cause-and-effect relationships of the occurrence of varicose veins are still a subject of debate and scientific research. Disturbances in the outflow of venous blood are most often caused by the absence or weakness of the vascular valve apparatus located deep in the tissues. Also, varicose veins of the lower extremities and other organs can be caused by a decrease in the tone of the vascular wall.
Less commonly, varicose veins in the legs are associated with conditions such as:
- previous inflammation of the veins (phlebitis);
- formation of blood clots in the venous bed;
- congenital anomalies of vascular development.
Causes and prevention of varicose veins of the lower extremities
The causes of varicose veins in most cases lie in a sedentary lifestyle: we spend a long time in a static position (especially sitting), and do not give the necessary stress to our muscles. The following risk factors may also affect:
- excessively tight clothing (pants, socks),
- uncomfortable shoes (especially high heels),
- disturbances in hormonal balance,
- frequent hot baths, sauna visits,
- prolonged serious physical activity, heavy lifting,
- obesity.
The main prevention of varicose veins is maintaining a healthy lifestyle. Even if you have a sedentary job, try not to sit without moving for several hours in a row: get up, stretch your legs, walk more; and don’t forget about a balanced diet, which, along with moderate physical activity, will protect you from many diseases.
Pregnancy is also one of the serious risk factors for varicose veins. But genetic predisposition is still being studied, and there are even a number of studies that refute it.
Modern methods of treating varicose veins
Unlike classical operations, treatment methods for varicose veins, carried out using modern technologies, have many advantages:
- In most cases, there is no need for hospitalization.
- The surgeon does not use general anesthesia (the patient is conscious). After surgery, patients are back on their feet immediately.
- The rehabilitation period is minimal. You can usually return to work the next day.
- There are no scars or scars left on the body.
- The risk of relapse is very low, not exceeding 3%. For comparison, when using classical methods, the probability of recurrence of the disease is up to 30%.
Modern methods include:
- Endovasal laser vein coagulation (EVLC)
- Radiofrequency obliteration (RFA/RFO)
- Sclerotherapy
- Miniphlebectomy
Endovasal laser vein coagulation (EVLC)
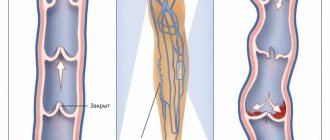
- EVLT refers to thermal methods of treatment.
- A light-conducting fiber is inserted into the vein under ultrasound guidance.
- The light beam heats the venous wall. Destruction of connective tissue occurs, causing blood flow through the vein to completely stop.
- A vein that has undergone this procedure is scarred - a fibrous cord is formed and disappears after 6-12 months.
- The result of EVLT is comparable to mechanical vein removal.
- The operation can be carried out with varying degrees of manifestation of opacity.
Symptoms of varicose veins
The disease can develop very slowly: years or even decades. The symptoms of the initial stage are varied, but for convenience they are combined into a certain complex under the general feeling of heaviness in the legs:
- fatigue in the legs without serious exercise,
- sore veins,
- night cramps in the calves,
- pulling sensation in legs.
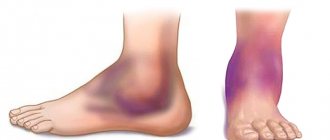
If you do not track the symptoms of varicose veins at the initial stage, the vein will become more and more deformed. In the evenings, swelling in the feet and ankles will begin to appear, disappearing by morning; Spider veins will become visible, and then swollen veins and nodules on them will be felt. If you do not consult a specialist at this stage, then in addition to the obvious decrease in quality of life and obvious pain, the person risks getting skin pigmentation and trophic ulcers. The further course of varicose veins brings complications such as bleeding from the venous nodes and the risk of developing such a serious disease as thrombosis, which can be fatal without contacting a specialist.
Drug therapy for varicose veins of the lower extremities
Today, a phlebologist has a wide range of different drugs in his arsenal that are used for varicose veins. The main indication for drug therapy is the presence of chronic venous insufficiency or prevention in risk groups.
Phleboprotectors are the main group of drugs that affect venous tone and protect its wall and valves from destruction. The main phleboprotector recommended by world associations of phlebologists is micronized diosmin (Detralex), which improves microcirculation, reduces vascular permeability and protects the venous wall and vein valves from destruction. In addition to the main drug in the treatment of varicose veins, phlebologists prescribe auxiliary drugs that help fight the symptoms of venous insufficiency in the legs (anti-inflammatory drugs, disaggregants, anticoagulants, antihistamines, glucocorticoids, including in the form of ointments and gels). Drug therapy is prescribed in courses. A course of medications is also recommended before and after surgical treatment (EVLT, sclerotherapy, miniphlebectomy) to prevent relapse.
Modern classification of drugs for the treatment of varicose veins:
1. Venotonic drugs:
- Detralex;
- Rutoside (Venoruton, Rutin);
- Tribenoside (Glivenol);
- Troxerutin (Troxevasin);
- Cyclo-tri-forte;
- Endothelon;
- Escin (Aescin, Venen, Venitan, Venoplant, Concentrin, Reparil, Aescusan);
- Ginkor-forte.
2. Drugs that improve blood flow in blood vessels:
- Pentoxifylline (Agapurin, Arbiflex, Vazonit, Darte-lin, Mellinorm, Pentilin, Pentohexal, Radomin, Ra-lofect, Trenpental, Trental, Flexital, Quinotal)
3. Anticoagulants:
- Heparin-containing ointments, gels (Troxevasin, Lyoton 1000 mg, Detragel)
Venotonic drugs
Detralex
Detralex is a venoprotector and venotonic. Effective in the treatment of all types of chronic venous insufficiency. Reduces the severity of symptoms of CVI of the lower extremities (feeling of heaviness, pain in the legs, night cramps, impaired trophic tissue of the legs). Detralex is also used to relieve acute hemorrhoidal attacks (acute attacks of hemorrhoids).
- improves vein tone;
- improves lymphatic drainage;
- normalizes microcirculation;
- fast-acting and lasting effect.
"Detralex" affects the venous vascular system: it reduces the distensibility of veins, increases their tone and reduces venous stagnation. At the microcirculation level, Detralex reduces capillary permeability and increases their resistance. Detralex improves lymphatic drainage.
Rutoside
(Venoruton, Rutin)
"Rutoside" belongs to the group of bioflavonoids (flavonols). Contained in the leaves of mint (Ruta graveolens L.) and other plants.
Has P-vitamin activity. Normalizes capillary permeability, strengthens the vascular wall, and has an anti-inflammatory effect. In patients with CVI, it leads to a reduction in swelling and pain, the disappearance of numbness and cramps.
Troxerutin
Troxerutin: Flavonoid (semi-synthetic derivative of rutin) - venotonic, angioprotective, anti-inflammatory, decongestant, antioxidant effect.
Normalizes the permeability of capillary walls, increases their tone. Increases the density of the vascular wall. Reduces inflammation in the vascular wall.
It is also used for CVI. It is recommended to use both in the initial and late stages of the disease. As a result of treatment, the feeling of heaviness in the legs disappears, swelling of the lower extremities decreases, and trophism improves.
Escin
Triterpene glycoside (saponin) from the fruits (seeds) of horse chestnut.
Synonyms: Aescin, Venastat, Venitan, Concentrin, Reparil, Cycloven forte, Aescin, Concentrin, Cycloven forte, Reparil, Venastat, Venitan.
Herbal preparations from horse chestnut (Aesculus hippocastanum L.): infusions and decoctions of bark, leaves, fruits have long been used in folk medicine as astringents, choleretic, hemostatic (for uterine and hemorrhoidal bleeding) agents. A particularly important pharmacologically active substance is escin - it largely determines the effectiveness of drugs obtained from horse chestnut (escusan, esflazide, etc.).
Escin has a pronounced capillary protective activity and has an anti-inflammatory effect.
Be healthy!
Make an appointment with a phlebologist
Surgeon-phlebologist - Andrey Aleksandrovich Nisin
You can make an appointment by calling (391) 218−35−13 or through your personal account
Diagnostics
Diagnosis of varicose veins is quite simple - it is a survey, examination of the patient and an ultrasound, which will show the affected area of the vein and the extent of the damage to select the optimal treatment. If for some reason (for example, when the damaged veins are located deep), the ultrasound does not provide all the necessary information, then the specialist will conduct an additional examination - phlebography - injection of a contrast agent into the vein, which under X-rays will show the smallest changes in the vein along the blood flow.
Questions from patients from the Internet:
Is it possible to cure varicose veins forever?
The answer to this question will be: yes and no. Varicose veins are a chronic progressive disease; the destruction of venous vessels continues throughout a person’s life. However, timely treatment by a phlebologist, the use of compression hosiery during exercise, and balanced physical activity can achieve stable remission for many years.
How long does the effect last after surgery on varicose veins?
The effect of modern intervention on the venous system lasts forever. The problem is that over the years, some healthy (at the time of surgery) veins undergo varicose transformation and correction of the venous blood flow is again required.
Is it possible to cure varicose veins?
It is impossible to completely cure varicose veins, given its chronic, progressive nature. It is possible to achieve a period of stable remission, which can last for years or even decades.
They say that after removal, new varicose veins appear. This is true?
In the context in which such a phrase is usually voiced, this is completely wrong. Removing (correctly) varicose veins not only improves blood flow in the soft tissues, but also removes the pathological load from healthy venous vessels. In other words, healthy veins become less likely to become varicose veins. The progression of varicose veins often leads to the appearance of new varicose veins years later. But this is a slightly different story.
When to see a doctor
If you have symptoms of chronic venous insufficiency and you want to determine the exact cause and completely get rid of the discomfort, then sign up for a consultation right now. Employees of the Phlebological Center of the City Clinical Hospital named after V.V. Veresaeva will check the condition of the vascular bed and give individual recommendations based on the treatment experience of the best clinics in the USA and Europe.
Causes of varicose veins
Weak or damaged valves can lead to varicose veins. Arteries carry blood from your heart to your tissues, and veins return blood to your heart. The veins in the legs work against gravity.
The contractions of the muscles in the lower legs act as a pump, and the walls of the elastic vein help blood return to your heart. Tiny valves in your veins open as blood flows toward your heart and then close to stop the blood flowing back. If these valves are weak or damaged, blood can flow backward and pool in the vein, causing the veins to stretch or twist.
Risk factors
These factors increase the risk of developing varicose veins:
- Age . The risk of varicose veins increases with age. Aging causes wear and tear on the vein valves that help regulate blood flow. Ultimately, wear and tear causes blood to flow back into your veins.
- Floor . Women are more likely to develop this disease. Hormonal changes during pregnancy, premenstruation, or menopause may be a factor because female hormones tend to reduce the elasticity of vein walls. Hormonal medications, such as birth control pills, may increase the risk of developing varicose veins.
- Pregnancy . During pregnancy, the volume of blood in your body increases. This change supports fetal growth, but can also lead to the unwanted side effect of dilated veins in the legs. Hormonal changes during pregnancy may also play a role.
- Family illness . If other family members have had varicose veins, you have a better chance.
- Obesity . Excess weight puts extra pressure on your veins.
- Standing or sedentary lifestyle . Your blood doesn't flow as well if you stay in the same position for a long time.
Complications
Complications of varicose veins, although rare, may include:
- Ulcer . Peptic ulcers can form on the skin near varicose veins, especially near the ankles. A discolored patch of skin usually appears before an ulcer forms. Call your doctor immediately if you suspect you have an ulcer.
- Blood clot formation . Sometimes the deep veins in the legs become enlarged. In such cases, the affected leg may become painful and swollen. Any persistent leg pain or swelling requires medical attention because it may indicate a blood clot, a condition medically known as thrombophlebitis.
- Bleeding . Sometimes veins very close to the skin can burst. This usually causes only minor bleeding. But any bleeding requires medical attention.
And so it became
There are few clinics that use new, less traumatic methods for treating varicose veins. The introduction of two minimally invasive (low-traumatic) techniques, the so-called, was revolutionary. endovenous laser coagulation (EVLC) and radiofrequency obliteration (RFO). Despite the complex names, their essence is simple: as with an ultrasound examination of the heart or liver, the probe’s progress through the vein is controlled using a sensor and its wall is cauterized in the right place. A kind of “brewing” occurs, blocking the lumen of the vein. This eliminates the very cause of the disease - blood through the vein stops flowing in the opposite direction, to the foot (and its outflow to the heart goes in a roundabout way - through other healthy veins). In the veins located below, the pressure does not increase - new nodes, blood clots and other changes do not develop. This virtually eliminates the possibility of relapse—recurrence of the disease. Within three years after the intervention, it occurs in only 2-3% of patients. All this is done without incisions, without anesthesia, under local anesthesia and does not leave any cosmetic defects.
“Stars” and small nodes are eliminated using sclerotherapy - a special composition in the form of foam is injected into them, the lumen closes, and they become invisible. In more serious cases, the so-called mini-phlebectomy. Unlike a conventional operation, this is a low-traumatic removal of veins: they are removed not in large parts, but little by little and without incisions - through punctures in the skin about 2 mm in size. The duration of the procedure is on average about 40-60 minutes. The subcutaneous injury is so small that the patient can walk after the operation. To prevent thrombosis, he is immediately put on compression hosiery (special compression stockings), and under the supervision of medical staff, he must walk along the clinic corridor for at least 30-40 minutes. After 1-1.5 hours, the patient can leave the clinic driving his car or even on foot.
In the postoperative period, as a rule, you can lead your usual lifestyle. You can go to work and mind your own business. The only prescription from the doctor is to wear compression stockings for about a month. They compress the veins, causing their walls to heal faster.
The advantages of such treatment over conventional surgical removal of veins are undeniable, but so far it is carried out mainly for a fee. In the last ten years, hundreds of thousands of patients around the world have been relieved of varicose veins using new treatment methods. And all this without incisions, scalpels, scars, without anesthesia or spinal anesthesia, without hospitalization and long recovery.
There are few contraindications for such an intervention. First of all, this is severe heart or respiratory failure, pregnancy. This treatment is not used if you have previously had deep vein thrombosis. In such cases, patients are often treated conservatively with compression stockings.