directions
Crossectomy is a modern and effective method of treating varicose veins in the complication stage - thrombophlebitis. The technique is based on ligation of the great saphenous vein and its tributaries at the confluence with the deep veins in the groin area. This technique is the only way to treat acute ascending varicothrombophlebitis, as it prevents the patient from dying from a terrible complication - pulmonary embolism. The main goal of crossectomy is to eliminate the possibility of a blood clot spreading into the deep veins of the thigh and the blood clot breaking off with the development of pulmonary embolism.
Our clinics in St. Petersburg
Structural subdivision of Polikarpov Alley Polikarpov 6k2 Primorsky district
- Pionerskaya
- Specific
- Commandant's
Structural subdivision of Zhukov Marshal Zhukov Ave. 28k2 Kirovsky district
- Avtovo
- Avenue of Veterans
- Leninsky Prospekt
Structural subdivision Devyatkino Okhtinskaya alley 18 Vsevolozhsk district
- Devyatkino
- Civil Prospect
- Academic
For detailed information and to make an appointment, you can call +7 (812) 640-55-25
Make an appointment
Recommendations for conducting
Planned crossectomy surgery is possible only in a hospital by experienced vascular surgeons. Sometimes intervention is prescribed urgently, when minutes are counting and the patient needs to be saved. Indications for such urgent measures are:
Doctors who perform vein crossectomy must have sufficient experience and skills in performing complex interventions. You cannot trust your own health to the first specialists you come across. The Dobromed clinic has created the necessary conditions for ligation and removal of veins on the legs. Famous vascular surgeons and phlebologists work here and can help their patients.
Preparation and performance of the operation
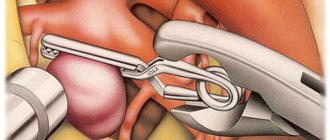
Before the operation, the doctor completely examines the patient and performs an ultrasound of the veins of the lower extremities. The operation itself is performed under local anesthesia and lasts on average about an hour. During the operation, a small oblique incision is made in the groin area, above the site of the desired vessel. The vessel is then mobilized and removed through the incision. Next, the doctor ties the large saphenous vein and sutures the surgical wound. The vein is crossed after ligating all estuarine venous tributaries 0.5-1.0 cm from the place of its confluence with the femoral vein.
Any operations on the veins should be carried out especially carefully and carefully. Careless movements of the doctor can lead to blood clots entering the bloodstream and the development of thrombosis.
The Medicenter clinic network employs qualified phlebologists who have extensive experience in performing vein operations and perform crossectomies without the risk of complications.
Possible complications
The crossectomy operation very rarely leads to any complications, but sometimes they are possible due to a violation of the intervention technique. We are aware of the following complications with this operation:
Lymphorrhea is the leakage of lymphatic fluid from an incision in the groin area. Lymphorrhea most often develops during operations for severe thrombophlebitis with a pronounced adhesive process in the area of the mouth of the great saphenous vein. In our practice, over 20 years, we encountered only one case of lymphorrhea, which resolved after 3 weeks.
Bleeding from the stump of the great saphenous vein is a rare complication that can develop with poor control over tying the ligature on the stump of the great saphenous vein. It manifests itself as an extensive hematoma in the access area and requires repeated surgery to stop the bleeding.
Thromboembolism from the stump of the great saphenous vein - can develop when a clamp or ligature is incorrectly placed on a vein containing thrombotic masses. With the technique used in our clinic, such a complication is impossible.
Suppuration of a postoperative wound - can be observed in very obese patients with a fatty apron covering the incision. To prevent this complication, we use multi-layer dressings that do not allow wound discharge to accumulate.
Postoperative period
After crossectomy, the patient recovers quite quickly. In the postoperative period, it is important to follow the doctor’s recommendations; for two weeks after crossectomy you should wear compression stockings and move a lot (activity helps restore and normalize blood flow). To prevent complications, the patient should take medications that reduce blood viscosity and clot formation.
Experts recommend combining crossectomy with other treatment methods. Most often, crossectomy is used in conjunction with conservative methods of local treatment.
After crossectomy
If the operation was performed for thrombophlebitis against the background of varicose veins, then subsequent intervention is necessary to eliminate varicose veins. Most often, we prescribe laser coagulation of the GSV trunk 2 months after thrombophlebitis. In some cases, the use of compression hosiery makes it possible to achieve obliteration of the saphenous vein trunk without additional interventions. Ultrasound monitoring of the condition of the saphenous veins must be carried out every 6 months.
Crossectomy: indications for performance
Crossectomy (Troyanov-Trendelenburg venectomy) may be recommended for patients at the Yusupov Hospital Therapy Clinic for the following diseases:
- in acute thrombophlebitis with a steadily ascending nature of thrombosis;
- with purulent thrombophlebitis, panphlebitis of various localizations (in the knee, femoral segment and above);
- with forms of thrombophlebitis resistant to antibacterial drugs (with immunodeficiency).
Thus, crossectomy is used for acute thrombophlebitis, i.e. complicated course of varicose veins.
Contraindications
Crossectomy has certain limitations. The operation cannot be performed in the following cases:
- The presence of malignant neoplasms in the body;
- Diabetes mellitus in advanced form;
- Obesity of various degrees;
- History of atherosclerosis;
- Cachexia;
- Narrowing of the lumen, blockage of deep-lying vessels;
- Severe renal or liver failure;
- Infectious diseases in the acute stage;
- Pregnancy period.
It is also worth noting that the procedure is not recommended in old age due to the high risk of complications.
Crossectomy: disadvantages of the method
Despite its high efficiency, the crossectomy method has several serious disadvantages:
- long rehabilitation period;
- the need for mandatory hospitalization of the patient in a 24-hour hospital.
Surgical treatment of varicose veins of the lower extremities, why did we completely abandon it?
As mentioned above, classical surgical treatment of varicose veins is actively used in European medical practice, including Moscow, the Moscow region and other Russian cities.
To the question: why is this, and why use horses when there are already good cars? By using a century-old operation, we lose the following advantages of innovation:
- No ultrasound imaging available. The intervention is controlled through the surgical wound; to improve visibility, it is necessary to enlarge the incision.
- Surgical trauma increases significantly. This not only increases the rehabilitation period, but also affects possible complications and side effects.
- The effectiveness of treatment decreases.
- In most cases, separation of the treating doctor from ultrasound diagnostics.
- Trauma, sometimes significant, at the sites of incisions and phleboextraction sites.
- Pseudo-radicalism. As practice shows, with phlebectomy, with very rare exceptions, significantly fewer varicose veins are removed than using modern techniques.
In the practice of the Moscow City Phlebological Center, we use only the best modern techniques and combined phlebectomy has long been out of place there.
What are the consequences of removing a vein in the leg? How does the blood drain after this?
Varicose veins are typical for superficial veins, which account for only 10% of venous blood flow. The remaining 90% of the blood flows through the deep veins, which take on additional load after removal.
If the patient still has doubts about the advisability of the operation, then an additional argument in favor of removing the vein can be the fact that the varicose vein is already practically cut off from their blood flow. It cannot ensure the normal movement of blood, which stagnates in it, still stretching the vascular wall. That is why the main “consequence” of phlebectomy (vein removal surgery) is the normalization of blood circulation in the extremities.
Reviews of doctors providing the service - crossectomy
I had surgery on 2 legs with Yuri Stanislavovich Malakhov.
I want to express my deep gratitude to him for a new breath of life, lightness on my feet, one might say, a completely different standard of living. Yuri Stanislavovich, you have golden hands and you are a doctor from God! I recommend it to everyone, women and men - don’t be afraid and... Read full review Irina Nikolaevna G
11.06.2021
I would like to sincerely thank the surgeon-phlebologist Yuri Stanislavovich Malakhov for the high-quality treatment of varicose veins using a modern method: no incision, no hospitalization, high cosmetic effect. The very next day I went to work. Yuri Stanislavovich is a professional... Read full review
Natalia Viktorovna F
18.04.2021
Surgical combined phlebectomy, why the technique is not ideal
Combined phlebectomy at one time made a splash, a kind of revolution both in the treatment and understanding of the pathogenesis of varicose veins. More than a century has passed since then, today milder versions of anesthesia and other surgical instruments are used, but no fundamental changes have occurred in this surgical technique. Even with the advent of innovations in the form of: PIN stripping, intussusception stripping and cryostripping, the technique essentially remained the same.
Cryostripping - removal of varicose veins with cold
Classic combined phlebectomy using a Babcock probe still remains the most widespread for the treatment of varicose veins in the public sector of medicine due to the unobvious advantages of the above innovations.
Crossectomy of the veins of the lower extremities: definition
Vein crossectomy is used for varicose veins and is a ligation (ligation) of the femoral vein (large or small). This prevents blood from flowing back through the diseased vessel. The procedure can be used either independently or during phlebectomy. Crossectomy of the great or small saphenous vein may be prescribed. It is pathological in nature and is considered a necessary measure.
Crossectomy: progress of the operation
The patient is asked to assume a supine position on the operating table. During the process, conduction anesthesia is used. Next steps:
- Disinfection of the surgical field in the area of previously determined access;
- Making a skin incision in the groin area and spreading the subcutaneous tissue until the vein trunk is visible;
- Isolation of a vein near the point of confluence, ligation of it along with its tributaries at a distance of 10 mm from the anastomosis;
- Stitching.
Crossectomy (ostial ligation of the great or small saphenous vein) is considered an effective way to prevent pulmonary embolism in acute ascending thrombophlebitis, since it prevents the spread of the thrombotic process from the superficial to the deep veins [1, 2]. The operation is short, low-traumatic, has been used for decades and has become routine in clinical practice. The vast majority of surgeons believe it is so reliable that if they use anticoagulants, it is only in prophylactic doses, and more often they are limited to the use of antiplatelet and venotonic drugs.
How justified is such an unconditional belief that crossectomy for ascending thrombophlebitis solves the problem of preventing pulmonary embolism? Our experience indicates that surgeons' expectations are too high, as evidenced by two clinical cases that we would like to present to the attention of our colleagues.
Patient S.
64 years old, was admitted to the surgical department on January 12, 2011 with complaints of a painful lump on the inner surface of the right thigh, redness of the skin in this area, pain in the right lower limb when walking.
From the anamnesis it is known that she was sick for 2 days and noted the occurrence of the above complaints. She did not report shortness of breath, hemoptysis, chest pain, or episodes of loss of consciousness during the course of the disease.
Upon examination, the condition is satisfactory. Breathing in the lungs is carried out in all parts, vesicular, there is no wheezing. Pulse 84 per minute, rhythmic, blood pressure 130/90 mm Hg. The abdomen is soft, painless in all parts. Peristalsis is audible, but not increased. Rectal and vaginal examinations revealed no pathology.
Local status: the right lower limb is not swollen, the skin is of normal color and warm. The pulsation in the arteries is clear throughout. Along the inner surface of the upper third of the leg, lower, middle and upper third of the thigh there is a dense painful cord with hyperemia of the skin above it. There are no varicose veins. Homans and Moses symptoms are negative.
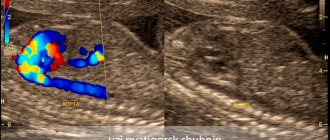
Ultrasound angioscanning of the veins of the lower extremities (USA): the right great saphenous vein is thrombosed along its entire length to the saphenofemoral junction (Fig. 1, a).
Figure 1. Angioscanograms of patient S. a - thrombus in the estuarine section of the great saphenous vein (arrow). The deep veins of both lower extremities are passable, their valves are intact. The perforating veins are not thrombosed.
In order to prevent deep vein thrombosis and pulmonary embolism, it was decided to perform a crossectomy. The surgical intervention was carried out without technical difficulties; no pronounced phenomena of periphlebitis were detected in the operation area.
In the postoperative period, the patient received compression (elastic bandaging), venotonic (troxerutin 300 mg 2 times a day) therapy. Taking into account the nature of the lesion, the age of the patient, the extent of the operation, and also taking into account the fact that there were no varicose veins, the risk of postoperative thromboembolic complications was assessed as high, and therefore unfractionated heparin 7500 units was prescribed 3 times under the skin of the abdomen until discharge from the hospital (7 days).
The patient in the hospital was additionally examined, an ultrasound examination of the abdominal organs, retroperitoneal space, esophagogastroduodenoscopy, colonoscopy was performed - no organic pathology was detected, examined by a gynecologist - no diseases of the internal genital organs were found.
During the control ultrasound examination of the veins of the lower extremities on the 5th day after surgery: the deep veins of both lower extremities are patent, no signs of thrombosis were detected.
The sutures were removed on the 8th day of the postoperative period, the patient was discharged from the hospital in satisfactory condition, recommendations: elastic compression of the lower extremities, taking antiplatelet and phlebotropic drugs.
At a follow-up examination 1 month after surgery, the patient did not have any complaints. Swelling and pain in the right lower extremity did not bother me, shortness of breath, hemoptysis, chest pain, or episodes of loss of consciousness were not noted.
Ultrasound examination revealed non-occlusive thrombosis of the right superficial femoral vein, which required the patient to be re-admitted to the hospital (Fig. 1, b).
Figure 1. Angioscanograms of patient S. b - non-occlusive thrombus of the right superficial femoral vein (arrows). Anticoagulant therapy was administered (unfractionated heparin 12,500 units 3 times under the skin of the abdomen for 8 days, followed by warfarin at a dose of 5 mg per day).
To exclude/confirm the asymptomatic form of pulmonary embolism, the patient underwent lung scintigraphy, which revealed disturbances in lung perfusion of the subsegmental type, which indicated the presence of thromboembolism of small branches of the pulmonary artery (Fig. 2, a).
Figure 2. Scintigrams of the lungs of patient S. a - impaired perfusion of the left lung according to the subsegmental type (arrows).
USAS on the 10th day of re-hospitalization: initial recanalization of the right superficial femoral vein. The patient was discharged from the hospital on the 14th day in satisfactory condition (INR at discharge 2.2). Elastic compression and warfarin for 6 months are recommended.
A follow-up examination after 2 months showed the absence of chronic venous insufficiency of the lower limb and cardiopulmonary failure. With USAS: good recanalization of the deep veins of the right lower limb. Lung scintigraphy indicated the absence of perfusion-ventilation disorders (Fig. 2, b).
Figure 2. Scintigrams of the lungs of patient S. b - after 2 months. Absence of perfusion-ventilation disorders.
An analysis of the medical history of this patient shows that the actions and prescriptions of the attending physicians in the hospital complied with all existing standards for the treatment of ascending thrombophlebitis of the main saphenous veins. However, this did not protect the patient from developing deep vein thrombosis and pulmonary embolism, which developed after discharge. The next incident ended more tragically.
Patient K., 48 years old, was admitted to the surgical department on March 28, 2011 with complaints of a painful lump on the inner surface of the right leg and thigh, redness of the skin in this area.
From the anamnesis: he was ill for 7 days, when a hyperemic, dense, sharply painful cord appeared along the inner surface of the right shin to the level of the knee joint.
He was treated on an outpatient basis under the supervision of a surgeon, using heparin ointment locally 2 times a day and taking troxerutin 300 mg 2 times a day. Despite treatment, over time the cord spread to the middle third of the right thigh. No shortness of breath, hemoptysis, chest pain, or episodes of loss of consciousness were noted during the course of the disease.
On examination the condition is of moderate severity. Breathing in the lungs is carried out in all parts, vesicular, there is no wheezing. Respiratory rate 17 per minute. Pulse 80 per minute, rhythmic, blood pressure 140/80 mm Hg. The abdomen is soft, painless in all parts. Peristalsis is audible, but not increased. A rectal examination revealed no pathology.
Local status: the right lower limb is not swollen, the skin is of normal color and warm. The pulsation in the arteries is clear throughout. Along the inner surface of the upper third of the leg, the lower and middle third of the thigh, there is a dense, painful cord with hyperemia of the skin above it. Homans and Moses symptoms are negative. Varicose dilation of the tributaries of the main veins on the legs. The left lower limb is not swollen, the skin is of normal color and warm. The pulsation in the arteries is clear throughout. Homans and Moses symptoms are negative.
With USAS: the right great saphenous vein is thrombosed along its entire length to the upper third of the thigh. The right small saphenous vein is thrombosed along its entire length to the middle third of the leg. The deep veins of both lower extremities are passable, their valves are intact. The perforating veins are not thrombosed.
In order to prevent deep vein thrombosis of the right lower limb and pulmonary embolism, it was decided to perform ligation of the small and great saphenous veins for the patient. The surgical intervention was carried out without technical difficulties, no pronounced phenomena of periphlebitis were detected in the operation area, and no thrombotic masses were detected upon palpation of the small and great saphenous veins within the surgical wound.
In the postoperative period, the patient underwent compression (elastic bandaging), venotonic (micronized purified flavonoid fraction 500 mg 2 times a day). Taking into account the patient's age and the extent of the surgical intervention, the risk of postoperative venous thromboembolic complications was assessed as moderate, and therefore unfractionated heparin was prescribed at a dose of 5000 units 3 times under the skin of the abdomen.
In the postoperative period, the patient complained of moderate pain in the area of postoperative wounds; there were no other complaints. Local status - no negative dynamics. On the 5th day after surgery, the patient suddenly developed severe shortness of breath at rest, a feeling of suffocation, and general weakness. On examination: the condition is serious, the skin is pale, cold sweat. Breathing is harsh, sharply weakened in the lower regions on both sides. Respiration rate 30 per minute. Heart sounds are muffled, pulse is 105 per minute, rhythmic. Blood pressure 90/60 mm Hg. The abdomen is soft, painless in all parts. Peristalsis is audible, but not increased. Local status: no negative dynamics, dressings are dry. The situation was assessed as massive thromboembolism of the pulmonary arteries.
Due to his serious condition and severe symptoms of respiratory and cardiovascular failure, the patient was transferred to the intensive care unit for further treatment. In order to clarify the extent of pulmonary lesions and determine further treatment tactics, the patient was decided to undergo computed tomography of the chest with intravenous bolus enhancement. However, despite the intensive therapy, the patient's condition quickly and progressively worsened, and the symptoms of cardiopulmonary failure increased. Against the background of severe bradycardia, resuscitation measures were started, but were unsuccessful. The patient was declared dead.
Autopsy revealed thrombosis of the left femoral vein and pulmonary embolism, which was recognized as the cause of death.
As in the previous case, it was hardly possible to blame the attending physicians for violating the protocol for managing patients with varicothrombophlebitis: an operation was performed to prevent the transition of thrombosis to the deep venous system, anticoagulant prophylaxis was carried out, as well as other conservative measures. Nevertheless, the patient died from a pulmonary embolism, the source of which was deep vein thrombosis of the contralateral limb that developed in the postoperative period.
These cases from everyday clinical practice clearly demonstrate that not always, not in every patient, even timely crossectomy is a guarantee against the development of such a formidable complication as pulmonary embolism. We are confident that similar situations can be reported by employees of any surgical clinic that has even a small flow of patients with ascending thrombophlebitis. Moreover, in our observations, anticoagulant prophylaxis was used, which also turned out to be ineffective. It is quite possible, although there is no consistent data on this in the literature, that in patients with ascending thrombophlebitis it is necessary to use other dosages of anticoagulants - therapeutic or intermediate. This should be the subject of close attention by the surgical community, as well as the duration of anticoagulant therapy for this pathology.
Conflict of interest
absent.
Rehabilitation period
For three days after surgery, it is recommended to remain in a hospital setting under constant medical supervision. If there are no complications, the sutures are removed, the drainage is removed, and the patient is transferred to outpatient treatment. During the recovery period, it is important to follow the following rules:
- It is mandatory to purchase compression stockings. The degree of compression is determined individually for each patient.
- For the fastest possible recovery, it is recommended to walk. The very next day after the operation, walking along the corridor is necessary, and on the following days, walking.
- At the same time, heavy physical activity should be abandoned - activity should be moderate.
- During the rehabilitation period, it is prohibited to take hot baths, visit saunas and steam baths. The timing is determined individually for each patient.
- It is recommended to eat well so that the body receives the necessary vitamins and minerals.
In addition, after the operation, the doctor prescribes medication:
- Antibacterial and anti-inflammatory drugs to reduce the risk of complications.
- Venotonic drugs to improve the tone of the venous wall.
- Painkillers to relieve discomfort after surgery.
- To prevent thrombosis, it is recommended to take anticoagulants.
- Vitamin complexes will support the immune system and speed up recovery.
More detailed information about crossectomy can be obtained during an in-person consultation with a doctor. Be healthy!
A complex approach
The algorithm described above is suitable for crossectomy as monotherapy for emergency situations when it is necessary to block possible complications of thrombosis immediately. But usually the operation becomes only part of an extensive phlebectomy, acting as the first step towards restoring the health of the legs. Here it is impossible to do without excision of the affected vessel.
The first step of combined radical intervention involves an inguinal incision in the area of the junction of the deep and superficial veins. The second vessel is cut off taking into account the degree of damage, and then ligated.
The second step involves making another cut at the top of the shin or near the ankle. Having identified the saphenous vein, a special probe made of metal material is launched there, which, as it moves, should reach the area of the first cut.
After the probe reaches the designated location, the veins are fixed. To do this, use a special thread, having previously placed it on the probe tip. The third part of the intervention is called the Babcock operation. It provides for long stripping on the left or right, which was made possible thanks to the use of a flexible probe tip. It is pulled through the incision, and the sharp edge of the instrumentation cuts off the vessel from the nearest intact tissue.
The strategy of miniphlebectomy, which is also called the Narata method, is discussed separately. This operative aspect involves removal of pre-marked venous nodules and tributaries followed by ligation of the perforating veins.
It is especially difficult for the surgeon if the vessels have a tortuous shape, which prompts the integrity of the integument to be broken in several places in order to remove the affected areas in parts. The nodes are removed using a special surgical device called a Müller hook.
To make the result look aesthetically pleasing, the punctures are made very small, up to 2 mm. Such wounds heal on their own without the need for stitches, and after a couple of months not even a trace remains of them.
How long is the postoperative period after vein surgery?
The period of hospital stay after the operation is limited to one day. This is necessary for the doctor to monitor the patient’s condition after anesthesia, as well as to change the dressing every other day.
After discharge from the clinic, it is recommended to spend a week at home, but not on bed rest. After surgery to remove varicose veins, movement is indicated: the patient needs to walk more.
After the operation, patients feel better: after all, the diseased vein is no longer there. But many people are concerned about the appearance of their legs. Remaining cosmetic defects can be removed using sclerotherapy.
Preparatory measures for crossectomy of the great saphenous vein of the thigh
Proper preparation for crossectomy plays an important role, helping to identify existing contraindications and reduce the risk of complications. It provides the following:
- General blood and urine tests;
- Biochemical blood test;
- Research for the presence of dangerous infectious lesions;
- Electrocardiography;
- Duplex ultrasound scanning of leg veins.
The latter is carried out immediately before crossectomy, noting the affected trunks.
Indications and contraindications
Previously, varicose veins were considered a disease that exclusively affected older people. Unfortunately, today the situation has changed significantly. Varicose veins are getting younger every day, and are now found even in teenagers.
Crossectomy is indicated in the following cases:
- The presence of thrombophlebitis of the lower extremities;
- Too frequent relapses of inflammation of the vein walls;
- Lack of positive effect from drug treatment;
- Thrombophlebitis in the area of the knee joint and above.
We can conclude that surgery is required for serious complications of varicose veins. Alas, even surgery does not guarantee a complete recovery. Stable remission can only be achieved with further comprehensive treatment.