The best treatment for heart failure is its prevention, which includes treatment of arterial hypertension, prevention of atherosclerosis, a healthy lifestyle, exercise and diet (primarily salt restriction). Treatment of heart failure, begun at the earliest stages, significantly improves the patient's life prognosis.
The main function of the heart is to supply oxygen and nutrients to all organs and tissues of the body, as well as remove their waste products. Depending on whether we are resting or actively working, the body requires different amounts of blood. To adequately meet the body's needs, the frequency and strength of heart contractions, as well as the size of the lumen of blood vessels, can vary significantly.
A diagnosis of heart failure means that the heart has ceased to sufficiently supply tissues and organs with oxygen and nutrients. The disease is usually chronic and the patient may live with it for many years before being diagnosed. Around the world, tens of millions of people suffer from heart failure, and the number of patients with this diagnosis increases every year. The most common cause of heart failure is a narrowing of the arteries that supply oxygen to the heart muscle. Although vascular disease develops at a relatively young age, the manifestation of congestive heart failure is most often observed in older people.
According to statistics, among people over 70 years of age, 10 out of 1,000 patients are diagnosed with heart failure. The disease is more common in women, because In men, there is a high mortality rate directly from vascular diseases (myocardial infarction) before they develop into heart failure.
Other factors that contribute to the development of this disease are hypertension, alcohol and drug addiction, changes in the structure of the heart valves, hormonal disorders (for example, hyperthyroidism - excessive function of the thyroid gland), infectious inflammation of the heart muscle (myocarditis), etc.
Classifications of heart failure
The world has adopted the following classification, based on the effects that appear at different stages of the disease:
Class 1: no restrictions on physical activity and no impact on the patient’s quality of life. Class 2: mild restrictions on physical activity and complete absence of discomfort during rest. Class 3: noticeable decrease in performance, symptoms disappear with rest. Class 4: Total or partial loss of function, symptoms of heart failure and chest pain occur even during rest.
Symptoms of heart failure
Depending on the nature of the disease, acute and chronic heart failure are distinguished.
Manifestations of the disease are:
- slowing down the speed of general blood flow,
- decrease in the amount of blood pumped out by the heart
- increased pressure in the heart chambers,
- accumulation of excess blood volumes, which the heart cannot cope with, in the so-called “depots” - the veins of the legs and abdominal cavity.
Weakness and fatigue are the first symptoms of heart failure.
Due to the inability of the heart to cope with the entire volume of circulating blood, excess fluid from the bloodstream accumulates in various organs and tissues of the body, usually in the feet, calves, thighs, abdomen and liver.
As a result of increased pressure and fluid accumulation in the lungs, a phenomenon such as dyspnea, or breathing difficulties, may occur. Normally, oxygen easily passes from the capillary-rich tissue of the lungs into the general bloodstream, but when fluid accumulates in the lungs, which is observed in heart failure, oxygen does not fully penetrate the capillaries. Low oxygen concentration in the blood stimulates increased breathing. Patients often wake up at night from attacks of suffocation.
For example, American President Roosevelt, who suffered from heart failure for a long time, slept sitting in a chair due to problems with breathing problems.
The release of fluid from the bloodstream into tissues and organs can stimulate not only breathing problems and sleep disorders. Patients suddenly gain weight due to swelling of soft tissues in the feet, legs, thighs, and sometimes in the abdomen. Swelling is clearly felt when pressing with a finger in these places.
In particularly severe cases, fluid may accumulate inside the abdominal cavity. A dangerous condition occurs - ascites. Ascites is usually a complication of advanced heart failure.
When a certain amount of fluid from the bloodstream enters the lungs, a condition characterized by the term “pulmonary edema” occurs. Pulmonary edema often occurs in chronic heart failure and is accompanied by pink, bloody sputum when coughing.
Insufficient blood supply affects all organs and systems of the human body. On the part of the central nervous system, especially in elderly patients, a decrease in mental function may be observed.
Treatment of chronic heart failure. Decompensation of CHF.
First of all, patients are advised to follow an appropriate diet and limit physical activity. You should completely avoid fast carbohydrates, hydrogenated fats, in particular those of animal origin, and also carefully monitor your salt intake. It is also necessary to immediately stop smoking and drinking alcohol.
All methods of therapeutic treatment of chronic heart failure consist of a set of measures that are aimed at creating the necessary conditions in everyday life that contribute to a rapid reduction in the load on the cardiovascular system, as well as the use of medications designed to help the myocardium work and influence impaired water processes. salt metabolism. The purpose of the volume of treatment measures is related to the stage of development of the disease itself.
Treatment of chronic heart failure is long-term. It includes:
- Drug therapy aimed at combating the symptoms of the underlying disease and eliminating the causes contributing to its development.
- A rational regime, including restriction of work activity according to the forms and stages of the disease. This does not mean that the patient must remain in bed all the time. He can move around the room, and exercise therapy is recommended.
- Diet therapy. It is necessary to monitor the caloric content of food. It must comply with the patient’s prescribed regimen. For obese people, the calorie content of food is reduced by 30%. On the contrary, patients with malnutrition are prescribed enhanced nutrition. If necessary, fasting days are carried out.
- Cardiotonic therapy.
- Treatment with diuretics aimed at restoring water-salt and acid-base balance.
Patients with the first stage are fully able to work; in the second stage, there is limited ability to work or it is completely lost. But in the third stage, patients with chronic heart failure require constant care.
Drug treatment
Drug treatment of chronic heart failure is aimed at increasing contraction functions and ridding the body of excess fluid. Depending on the stage and severity of symptoms for heart failure, the following groups of drugs are prescribed:
- Vasodilators and ACE inhibitors - angiotensin-converting enzyme (enalapril, lisinopril, perindopril, ramipril) - reduce vascular tone, dilate veins and arteries, thereby reducing vascular resistance during heart contractions and helping to increase cardiac output;
- Cardiac glycosides (digoxin, etc.) – increase myocardial contractility, increase its pumping function and diuresis, and promote satisfactory exercise tolerance;
- Nitrates (nitroglycerin, dilasid, etc.) - improve blood flow to the ventricles, increase cardiac output, dilate the coronary arteries;
- Diuretics (furosemide, spironolactone, torsemide) – reduce the retention of excess fluid in the body;
- B-blockers (carvedilol, bisoprolol) - reduce heart rate, improve blood flow to the heart, increase cardiac output;
- Drugs that improve myocardial metabolism (B vitamins, mildronate, potassium preparations);
- Anticoagulants (aspirin, warfarin, rivaroxaban) – prevent thrombus formation in blood vessels.
Monotherapy in the treatment of CHF is rarely used, and only ACE inhibitors can be used in this capacity in the initial stages of CHF.
Triple therapy (ACE inhibitor + diuretic + glycoside) was the standard in the treatment of CHF in the 80s, and now remains an effective regimen in the treatment of CHF, however, for patients with sinus rhythm, it is recommended to replace the glycoside with a beta-blocker. The gold standard from the early 90s to the present is a combination of four drugs - ACE inhibitor + diuretic + glycoside + beta-blocker.
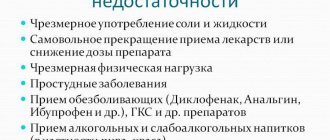
Decompensation of CHF
The main symptoms that require immediate medical attention Heart failure is a very dangerous condition in which the heart is not able to sufficiently perform its functions. As a result, the organs and all tissues of the body do not receive the required amount of blood, which supplies oxygen and nutrients. This disease has several stages of development, the most dangerous, the third, is decompensation.
Heart failure in the decompensation stage often leads to death. In this case, the heart fails to cope with its task not only during physical or emotional stress, but even if the person is in a calm state. This form is irreversible, and therefore so dangerous.
Decompensated heart failure is characterized by:
- Enlargement of the myocardium, or rather, its stretching and thinning.
- Fluid retention in the body.
- Rapid decrease in cardiac output.
- Swelling of the myocardium.
The chronic form of decompensation is a long-term process, that is, this pathology develops over the course of years, and at the same time progresses. Its peculiarity lies in the fact that due to any damage to the organ (necrosis, inflammation, dysplasia), the myocardial cells change. This affects its functioning. But the cells that are not yet affected do the work of compensating for the dysfunction of the affected myocytes. Then decompensation occurs, and the heart is not able to pump blood in the required quantity.
Symptoms
Pathology exhibits quite a lot of symptoms. There are no specific signs by which the disease can be accurately diagnosed.
Decompensated heart failure is a consequence of other heart diseases, so the clinical picture is quite varied, as some symptoms overlap with others.
The main symptoms of decompensated heart failure:
- Dyspnea. It manifests itself under light loads, but if there is no appropriate treatment, the pathology progresses and is disturbing, even if the person is in a calm state. This occurs due to congestion in the lungs.
- Swelling of the legs and arms. They are explained by impaired outflow of fluid from the body. In this case, the heart muscle is also affected.
- Dry cough.
- Pain or discomfort in the right hypochondrium.
- Ascites is dropsy in the abdominal cavity. At the same time, the stomach and weight of a person increase significantly.
- General weakness, feeling of overwork.
- Cold feet and hands.
- Small amount of urine, rare urge to urinate.
Prevention and prognosis
To prevent heart failure, you need proper nutrition, sufficient physical activity, and giving up bad habits. All diseases of the cardiovascular system must be promptly identified and treated.
The prognosis in the absence of treatment for CHF is unfavorable, since most heart diseases lead to its wear and tear and the development of severe complications. When carrying out drug and/or cardiac surgery, the prognosis is favorable, because the progression of the insufficiency slows down or a radical cure for the underlying disease occurs.
Left side or right side?
The different symptoms of heart failure depend on which side of the heart is involved. For example, the left atrium (upper chamber of the heart) receives oxygenated blood from the lungs and pumps it into the left ventricle (lower chamber), which in turn pumps blood to the rest of the organs. When the left side of the heart cannot pump blood efficiently, it backs up into the pulmonary vessels and excess fluid flows through the capillaries into the alveoli, causing difficulty breathing. Other symptoms of left-sided heart failure include general weakness and excessive mucus (sometimes mixed with blood).
Right-sided insufficiency occurs when there is difficulty in the outflow of blood from the right atrium and right ventricle, which happens, for example, when the heart valve is not functioning properly. As a result, pressure increases and fluid accumulates in the veins ending in the right chambers of the heart - the veins of the liver and legs. The liver becomes enlarged, painful, and the legs become very swollen. With right-sided insufficiency, a phenomenon such as nocturia or increased nighttime urination is observed.
In congestive heart failure, the kidneys cannot handle large volumes of fluid, and kidney failure develops. Salt, which is normally excreted by the kidneys along with water, is retained in the body, causing even greater swelling. Renal failure is reversible and disappears with adequate treatment of the main cause - heart failure.
3. How to prevent worsening of the condition in heart failure?
To prevent congestive heart failure from progressing, it is important to monitor your health very closely. Do not violate the recommended medication regimen. And you need to regularly visit your doctor to make sure that the disease is not developing. Fluid retention in the body is one of the symptoms of heart failure and is a reason to immediately consult a doctor. Dizziness, weakness, shortness of breath can also be signs of heart failure, and if these symptoms reappear during treatment, do not delay a visit to a specialist.
About our clinic Chistye Prudy metro station Medintercom page!
Causes of heart failure
There are many reasons for the development of heart failure. Among them, the most important place is occupied by coronary heart disease or insufficient blood supply to the heart muscle. Ischemia, in turn, is caused by blockage of the heart vessels with fat-like substances.
A heart attack can also cause heart failure because some of the heart tissue dies and becomes scarred.
Arterial hypertension is another common cause of insufficiency. The heart requires much more effort to move blood through the spasmodic vessels, which results in an increase in its size, in particular the left ventricle. Later, weakness of the heart muscle or heart failure develops.
Causes that influence the development of heart failure include cardiac arrhythmias (irregular contractions). A number of beats of more than 140 per minute is considered dangerous for the development of the disease, because the processes of filling and ejection of blood by the heart are disrupted.
Changes in the heart valves lead to disturbances in the filling of the heart with blood and can also cause the development of heart failure. The problem is usually caused by an internal infection (endocarditis) or a rheumatic disease.
Inflammation of the heart muscle caused by infection, alcohol or toxic damage also leads to the development of heart failure.
It should be added that in some cases it is impossible to establish the exact cause that caused the deficiency. This condition is called idiopathic heart failure. Diagnosis of heart failure
Using a stethoscope, the doctor listens for unusual sounds in the lungs that occur due to the presence of fluid in the alveoli. The presence of fluid in a particular area of the body can also be detected using x-rays.
The doctor listens for heart murmurs that occur as blood fills and ejects, as well as when the heart valves work.
Blue discoloration of the extremities (cyanosis), often accompanied by chills, indicates insufficient oxygen concentration in the blood and is an important diagnostic sign of heart failure.
Swelling of the limbs is diagnosed by finger pressure. The time required to smooth out the compression area is noted.
To assess heart parameters, techniques such as echocardiogram and radionuclide cardiogram are used.
During cardiac catheterization, a thin tube is inserted through a vein or artery directly into the heart muscle. This procedure allows you to measure the pressure in the chambers of the heart and identify the location of blockage of blood vessels.
An electrocardiogram (ECG) provides a graphical assessment of changes in heart size and rhythm. In addition, using an ECG you can see how effective drug therapy is. What are the body's defenses to combat deficiency?
In cases where an organ or system of the body is unable to cope with its functions, protective mechanisms are activated and other organs or systems take part in solving the problem. The same is observed in the case of heart failure.
Firstly, changes occur in the heart muscle. The chambers of the heart increase in size and work harder to pump more blood to the organs and tissues.
Secondly, the heart rate increases.
Third, a compensatory mechanism called the renin-angiotensin system is activated. When the amount of blood ejected by the heart is reduced and less oxygen reaches the internal organs, the kidneys immediately begin producing a hormone called renin, which allows salt and water excreted in the urine to be retained and returned to the bloodstream. This leads to an increase in the volume of circulating blood and an increase in pressure. The body must make sure that enough oxygen is supplied to the brain and other vital organs. This compensatory mechanism, however, is only effective in the early stages of the disease. The heart turns out to be unable to work at high pressure for many years under conditions of high pressure.
Tachycardia
Thyrotoxicosis
Iron deficiency
Climax
Menopause
13755 12 February
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Tachycardia: causes of occurrence, in what diseases it occurs, diagnosis and treatment methods.
Definition
Tachycardia is a condition in which the heart rate is more than 100 beats per minute. Tachycardia is not an independent disease, but is a symptom (manifestation) of certain diseases. In addition to rapid heartbeat, this condition is characterized by shortness of breath, weakness, chest pain, and sometimes loss of consciousness.
If shortness of breath and chest pain worsens, you should immediately seek medical help.
Types of tachycardia
One of the classifications divides tachycardia into physiological and pathological.
Physiological tachycardia is characterized by the absence of damage to the heart muscle and cardiac pathways. This type of tachycardia can be called compensatory, since it develops in response to an increase in the body’s need for oxygen, for example, during sports, psycho-emotional stress, being at high altitudes, etc.
Physiological tachycardia is characterized by the following manifestations:
- changes in heart rate are transient (not permanent);
- there is an obvious connection with a provoking factor (stress, severe anxiety, physical activity);
- upon completion of the action of the provoking factor, the heart rate gradually returns to normal;
- there are no pathologies from the cardiovascular system (for example, congenital heart defects, previous heart attacks, damage to the heart valve apparatus and other heart rhythm disorders).
Pathological tachycardia is observed in the following diseases and conditions:
- Hyperfunction of the thyroid gland (hyperthyroidism, thyrotoxicosis, diffuse toxic goiter).
- Diseases of the adrenal glands with their hyperfunction and, as a result, increased release of adrenaline into the blood.
- Damage to the conduction pathways of the heart due to a heart attack, congenital pathology of the heart valve apparatus.
- Presence of anemia (decreased blood hemoglobin level).
- Damages of the heart muscle (for example, myocarditis, pericarditis).
- Hormonal changes in the body (pregnancy, menopause).
Possible causes of tachycardia
Tachycardia with
hyperfunction of the thyroid gland
is more often observed in women than in men. An increase in thyroid hormone levels is reflected in the sinus node, which is located in the right atrium. It generates electrical impulses that cause myocardial contractions. When hormone levels are high, they reproduce chaotically, affecting the heart. As a result, the heart rate increases and tachycardia occurs.
Adrenal cortex dysfunction, or Addison's disease
, in which the adrenal glands cannot produce enough hormones. Their deficiency leads to the fact that the kidneys begin to quickly excrete sodium and water in the urine, dehydration of the body occurs, the water-electrolyte balance is disturbed, the blood thickens, circulation and blood supply to peripheral tissues slow down. Against the background of these changes, pathological changes in the cardiovascular system occur.
For anemia
the increase in the number of heart contractions is due to the need to maintain the required level of oxygen in the blood in conditions of hemoglobin deficiency.
Let us recall that hemoglobin is a carrier of oxygen to tissues and is found in red blood cells.
When hemoglobin levels decrease, an increase in heart rate allows blood and oxygen to be “driven” to the tissues faster, which makes it possible to partially maintain the required level of oxygenation. There are several types of anemia, including those associated with bone marrow pathology (for example, aplastic anemia, leukemia), with a lack of microelements (iron deficiency, B12 and folate deficiency anemia), anemia due to blood loss (chronic and acute).
If you suspect the development of anemia due to acute blood loss, you should immediately seek medical help.
Tachycardia
in pregnant women is caused by both an increase in the need of the mother and fetus for oxygen, and an increase in the consumption of serum iron, folate, and cyanocobalamin.
Tachycardia may develop while taking certain medications
, drinking
coffee
and
caffeine-containing products
, energy drinks containing
taurine, smoking
.
Which doctors should I contact?
If you suspect a pathology of the thyroid gland or adrenal glands, you should contact an endocrinologist. To treat conditions associated with cardiac dysfunction, see a cardiologist. If you have anemia, see a therapist or hematologist. Pregnant women are observed in the antenatal clinic, where an obstetrician-gynecologist can promptly identify the pathology and prescribe treatment.
Diagnosis and examinations for tachycardia
When a patient presents with symptoms characteristic of tachycardia, it is necessary to find out whether the tachycardia is the root cause of the deterioration in well-being that prompted the patient to see a doctor, or whether it is secondary and there is an underlying disease.
If there is a suspicion of thyroid pathology, the level of thyroid hormones in the blood (T3 - triiodothyronine, T4 - thyroxine and their free fractions) and the level of thyroid-stimulating hormone are determined.
Treatment of heart failure
For drug therapy of heart failure, the following groups of drugs are used: diuretics, cardiac glycosides, vasodilators (nitrates), calcium channel blockers, beta blockers and others. In particularly severe cases, surgical treatment is performed.
Diuretics have been used since the 50s of the 20th century. The drugs help the heart function by stimulating the excretion of excess salt and water in the urine. As a result, the volume of circulating blood decreases, blood pressure decreases, and blood flow improves.
The most important for heart failure is a group of drugs derived from the digitalis plant or “cardiac glycosides”. These medicinal substances were first discovered in the 18th century and are widely used to this day. Cardiac glycosides affect internal metabolic processes inside heart cells, increasing the force of heart contractions. Thanks to this, blood supply to internal organs significantly improves.
Recently, new classes of drugs, such as vasodilators (vasodilators), have been used to treat heart failure. These drugs primarily affect peripheral arteries, stimulating their dilation. As a result, by facilitating blood flow through the vessels, heart function improves. Vasodilators include nitrates, angiotensin-converting enzyme blockers, and calcium channel blockers.
In emergency cases, surgical intervention is performed, which is especially necessary when the failure is caused by disorders of the heart valves.
There are situations when the only way to save a patient’s life is a heart transplant.