Altitude sickness
When a resident of a flat area comes to the mountains on vacation, it seems that the air there is especially clean and it is simply impossible to breathe it.
In fact, such reflex urges to breathe frequently and deeply are caused by hypoxia. In order for a person to equalize the partial pressure of oxygen in the alveolar air, he needs to ventilate his own lungs as best as possible at first. Of course, after staying in the mountains for several days or weeks, the body begins to get used to the new conditions by adjusting the functioning of the internal organs. This is how the situation is saved by the kidneys, which begin to secrete bicarbonate to enhance ventilation of the lungs and increase the number of red blood cells in the blood that can carry more oxygen.
Thus, residents of mountainous areas always have higher hemoglobin levels than those living in lowlands.
Acute form
Depending on the characteristics of the body, the norm of partial pressure of oxygen may differ for each person at a certain age, state of health, or simply depending on the ability to acclimatize. That is why not everyone is destined to conquer the peaks, because even with a great desire, a person is not able to completely subjugate his body and force it to work differently.
Very often, untrained climbers may develop various symptoms of hypoxia during high-speed ascent. At an altitude of less than 4.5 km, they are manifested by headaches, nausea, fatigue and sudden changes in mood, since the lack of oxygen in the blood greatly affects the functioning of the nervous system. If such symptoms are ignored, cerebral or pulmonary edema subsequently develops, each of which can lead to death.
Thus, it is strictly prohibited to ignore changes in the partial pressure of oxygen in the environment, because it always affects the performance of the entire human body.
Diving underwater
When a diver dives into conditions where the atmospheric pressure is lower than usual, his body also faces a kind of acclimatization. The partial pressure of oxygen at sea level is an average value and also changes with immersion, but nitrogen is of particular danger to humans in this case. On the surface of the earth in flat areas, it does not affect people, but after every 10 meters of immersion it gradually contracts and provokes various degrees of anesthesia in the diver’s body. The first signs of such a violation may appear after 37 meters under water, especially if a person spends a long time at depth.
When atmospheric pressure exceeds 8 atmospheres, and this figure is reached after 70 meters under water, divers begin to feel nitrogen narcosis. This phenomenon is manifested by a feeling of alcoholic intoxication, which disrupts the submariner’s coordination and attentiveness.
To avoid consequences
In cases where the partial pressure of oxygen and other gases in the blood is abnormal and the diver begins to feel signs of intoxication, it is very important to ascend as slowly as possible. This is due to the fact that with a sharp change in pressure, the diffusion of nitrogen provokes the appearance of bubbles with this substance in the blood. In simple terms, the blood seems to boil, and the person begins to feel severe pain in the joints. In the future, he may develop disturbances in vision, hearing and the functioning of the nervous system, which is called decompression sickness. To avoid this phenomenon, the diver should be lifted very slowly or the nitrogen in his breathing mixture should be replaced with helium. This gas is less soluble, has lower mass and density, so the cost of external respiration is reduced.
If such a situation occurs, then the person must be immediately placed back into the high-pressure environment and wait for gradual decompression, which can last up to several days.
Blood gases affect pH
Despite the fact that the study of the acid-base status, strictly speaking, implies the study of only the pH (concentration of H + ions), in reality it also includes the study of physiologically important gases present in the blood - O2 and CO2. Gas analysis shows the efficiency of gas exchange by the values of partial pressures - pO2 and pCO2 .
Molecules of any gases move diffusely through the alveolar membrane along a concentration gradient. O2 molecules of atmospheric air flow from the alveoli into the blood, and CO2 molecules from the blood into the alveoli until their partial pressures are equalized.
The partial pressure is the percentage of gas in the total volume.
Carbon dioxide
The concentration of CO2 in the alveolar air is so low and in the blood so high that the diffusion of this gas into the alveoli is extremely effective and the rate of its removal depends only on alveolar ventilation - the total volume of air transported per minute between the alveoli and a).
Hence,
- With increased ventilation of the lungs, carbon dioxide is quickly eliminated, and the pCO2 in the blood decreases . This means the body loses carbonic acid (H+ ions), which causes alkalization of the blood - alkalosis , called respiratory or respiratory .
- with insufficient alveolar ventilation, the pCO2 value increases, which indicates insufficient removal and accumulation of H2CO3. In other words, an increase in pCO2 in the blood is the cause of respiratory acidosis.
Increased pCO2 (hypercapnia) always indicates a decrease in alveolar ventilation.
Oxygen
Issues related to blood oxygenation and oxygen transport are more complex. This is due to the fact that only a small fraction of the total oxygen in the blood is found in the form of free (dissolved) O2 molecules. The main part of oxygen is associated with hemoglobin (oxyhemoglobin) and the true oxygen content depends on two additional parameters - Hb concentration and saturation (saturation) of hemoglobin with oxygen.
Oxyhemoglobin
Oxyhemoglobin (HbO2) – percentage in the blood, is the ratio of the oxyhemoglobin fraction (HbO2) to the sum of all fractions (total hemoglobin).
Hemoglobin oxygen saturation
Hemoglobin oxygen saturation (HbOSAT, SO2) is the ratio of the fraction of oxygenated hemoglobin to the amount of hemoglobin in the blood that is capable of transporting O2.
The differences between the two indicators HbO2 and HbOSAT are that patients may have a form of hemoglobin in their blood that is not capable of accepting O2 (Hb‑CO, metHb, sulfoHb). But since most patients do not have elevated levels of these forms of hemoglobin in their blood, the values of HbO2 and SO2 are usually very close.
For example, if in case of nitrite poisoning the amount of metHb is 15%, then the HbO2 value can never exceed 85%, but the saturation (HbOsat) can be different - from a maximum (HbOsat = 95-98%) with full saturation to low values in the absence of oxygen .
The oxygen saturation index shows the percentage of available binding sites on hemoglobin.
Illustration of the concepts of oxyhemoglobin (HbO2) and hemoglobin saturation (HbO2sat)
Partial pressure of oxygen (pO2)
The partial pressure of O2 acts as the driving force leading to the saturation of hemoglobin with oxygen. And although, as a rule, the higher the pO2, the higher the HbOsat, this relationship is not linear.
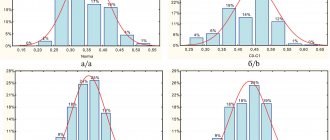
Hemoglobin dissociation curve under normal conditions and with changes in pH and 2,3-diphosphoglycerate concentration
In the central part of the hemoglobin saturation curve (or dissociation curve), the slightest shifts in pO2 lead to sharp changes in hemoglobin saturation. Conversely, at high pO2 (80-90-100 mmHg) the curve becomes flat, hemoglobin saturation depends little on fluctuations in oxygen in the plasma.
A shift to the left occurs with alkalization and a decrease in the concentration of 2,3-diphosphoglycerate and signals an increase the affinity of oxygen for hemoglobin (in the lungs). A shift to the right is a decrease in the affinity of oxygen for hemoglobin (in tissues), which is ensured by acidification of the environment and the accumulation of 2,3-diphosphoglycerate.
The pO2 value does not reflect the oxygen content of whole blood! But although pO2 does not indicate the total amount of oxygen in the blood, this total amount depends on pO2 through the hemoglobin saturation indicator.
In turn, there are factors that influence the pO2 value:
1. Alveolar ventilation . Although it affects both pO2 and pCO2, the proportion of oxygen in the alveoli during hyperventilation can only slightly increase, approaching the pO2 of atmospheric air; during hypoventilation, it rapidly falls, being replaced by CO2 coming from the blood. At the same time, the proportion of CO2 in the alveoli decreases rapidly with increased ventilation.
2. Ventilation-perfusion ratio is determined by the fact that
- not all the blood flowing to the lungs comes into contact with the well-ventilated alveoli (collapse of the alveoli, hardening of the wall).
- not all well-ventilated alveoli receive enough blood (right ventricular heart failure).
3. Oxygen concentration in inspired air (FiO2, fraction of inspired oxygen).
The table shows comparative values for the concentrations of oxygen and carbon dioxide in the air, blood and tissues. It is necessary to pay attention to changes in the concentrations of oxygen and carbon dioxide in the blood and alveolar air. An important feature is that pO2 in alveolar air and arterial blood are very close, i.e. Under normal conditions, deep and/or frequent breathing cannot increase oxygen consumption and saturation of hemoglobin. At the same time, the difference in pCO2 concentrations in venous blood and alveolar air allows it to be effectively removed with frequent breathing.
| pO2, mm Hg | pCO2, mm Hg | |
| Inhaled air | 159 | 0,23 |
| Alveolar air | 105-110 | 40 |
| Arterial blood | 83-108 | 35-45 |
| Fabrics | 10-20 | 50-60 |
| Deoxygenated blood | 35-49 | 46-51 |
| Exhaled air | 116 | 32 |
0
Partial pressure of oxygen in arterial blood
In order for the gas composition of the blood to change, it is not necessary to conquer peaks or descend to the seabed. Various pathologies of the cardiovascular, urinary and respiratory systems can also affect changes in gas pressure in the main fluid of the human body.
To accurately determine the diagnosis, appropriate tests are taken from patients. Most often, doctors are interested in the partial pressure of oxygen and carbon dioxide, since they ensure proper breathing of all human organs.
Pressure in this case is a process of dissolution of gases, which shows how efficiently oxygen works in the body and whether its indicators correspond to standards.
The slightest deviations indicate that the patient has deviations that affect the ability to use the gases entering the body to the maximum.
Arterial blood gases: metabolic, respiratory acidosis, alkalosis
Misinterpretation of blood gases can lead to dangerous therapeutic decisions. These guidelines describe a simple approach to help you correctly interpret your blood gas results.
- 9.1 Why is recognizing compensation important?
- 10.1 What is the alveolar-arterial gradient?
- 11.1 Respiratory acidosis
Key points
- There are four main types of acid-base imbalance: Respiratory acidosis
- Metabolic acidosis
- Respiratory alkalosis
- Metabolic alkalosis
Blood pH control
Normal blood pH is somewhat alkaline (7.35-7.45). In order to function normally, the body maintains the blood pH at approximately 7.4. There are three mechanisms by which the body maintains acid-base balance within this narrow range:
- Intracellular and extracellular buffer systems
- Renal regulation
- Regulation with the help of the lungs.
The most important pH buffer systems include hemoglobin, carbonic acid (a weak acid that is formed when CO2 dissolves) and bicarbonate (its weak base). The bicarbonate buffer is effective because the concentrations of its components can be independently adjusted. Its key components are CO2 and HCO3—.
- The lungs regulate the partial pressure of CO2 in the blood (pCO2) by regulating alveolar ventilation
- The kidneys regulate HCO3 concentrations by regulating renal carbonic acid excretion and bicarbonate reabsorption
Henderson-Hasselbach EquationBlood gas analyzers directly measure pH and pCO2 levels. HCO3 level—calculated using the Henderson-Hasselbach equation. This equation shows that the pH value is determined by the ratio of the concentration of HCO3- to pCO2, and not just the value of one of the components.
The simplified version of the equation below shows the relationship between these three quantities. If you remember this option, it will help you understand compensatory changes, which are described later in the module.
Definitions
Acidemia
Occurs when the blood pH is below 7.35.
Alkalemia
Occurs when the blood pH is above 7.45.
Acidosis
- This is the process that causes acids to build up in the blood
- Does not necessarily lead to abnormal pH levels
- From the Henderson-Hasselbach equation, you can see that acidosis can be caused by a decrease in HCO3—or an increase in pCO2:
- Occurring in isolation it leads to acidemia
- When developing simultaneously with alkalosis, the resulting blood pH may be normal, increased or decreased
Alkalosis
- This is a process that causes alkali to accumulate in the blood
- Does not necessarily lead to abnormal pH levels
- From the Henderson-Hasselbach equation you can see that alkalosis can be caused by an increase in HCO3—or a decrease in pCO2:
- Occurring in isolation it leads to alkalemia
- When developing simultaneously with acidosis, the resulting blood pH may be normal, increased or decreased
Base excess
Base excess is the amount of base or acid required to titrate one liter of blood to a pH of 7.4 at a constant pCO2 of 5.3 kPa. In the context of acidosis, a negative base excess value indicates the presence of a metabolic component.
Why and how to measure ABG
Why measure arterial blood gas composition?
You should determine your blood gas composition in order to:
- Determine acid-base balance
- Determine oxygenation level (arterial pO2 provides information about the efficiency of gas exchange and is more accurate than determining peripheral oxygen saturation)
- Diagnose and establish the severity of respiratory failure (pCO2 level provides information regarding ventilation of the lungs)
- Decide on treatment, such as oxygen or noninvasive ventilation for patients with chronic obstructive pulmonary disease (COPD) or therapy for patients with diabetic ketoacidosis.
The four main acid-base disorders are:
- Respiratory acidosis
- Metabolic acidosis
- Respiratory alkalosis
- Metabolic alkalosis.
Interpretation of ABG results
A step-by-step approach to interpreting arterial blood gas results
The following approach is a systematic way to help you correctly interpret arterial blood gas results (Table 1).
Table 1. Five steps for interpreting arterial blood gas results
| Step 1 | Is acidemia or alkalemia present? |
| Step 2 | Is the primary disorder respiratory or metabolic? |
| Step 3 | In cases of metabolic acidosis, is an increased anion gap present? |
| Step 4 | Is there compensation available? If so, is it appropriate? |
| Step 5 | What is the alveolar-arterial gradient? Look at arterial pO2 in the context of inspired oxygen concentration and arterial pCO2 |
First of all, you need to know the normal values (Table 2). Please note that these rates vary slightly between hospitals, so always use your hospital's normal rates.
Table 2: Normal arterial blood gas values
| Arterial pCO2 | 4.5-6.0 kPa |
| Arterial pO2 | 11.0-13.0 kPa |
| HCO3— | 22.0-28.0 mmol/l |
| Base excess | -2.0 to +2.0 |
| Anion gap | 8.0-16.0 mmol/l |
| Chlorides | 98.0-107.0 mmol/l |
Step 1: Acidemia or Alkalemia?
Look at the pH. If he:
- below 7.35, then the patient has acidemia
- above 7.45 - the patient has alkalemia.
If the pH is normal, then look at the pCO2 level and the HCO3- concentration. If one or two indicators deviate from the norm, then the patient may have a mixed disorder.
Step 2: Respiratory or Metabolic?
Is the primary disorder respiratory or metabolic?
Look at pH, pCO2 and HCO3- concentration.
- If the pH is below 7.35 then acidosis causes acidemia and: if the pCO2 level is elevated then it is primary respiratory acidosis
- if the concentration of HCO3- is reduced, then this is primary metabolic acidosis.
- if the pCO2 level is reduced, then this is primary respiratory alkalosis
Step 3: Causes of Acidosis
In the case of metabolic acidosis, is there an increased anion gap?
Determining the type of acidosis will help you narrow down possible underlying causes.
What is an anion gap?
In the body, the number of cations and anions is the same. Blood tests measure most cations and only a few anions. Therefore, when all the measured anions and cations are added, an interval remains that represents unmeasured anions such as plasma protein, albumin.
Since Na+ is the main cation measured and Cl- and HCO3- are the main anions measured, the anion gap is calculated using the following formula:
Na+ — (HCO3— +Cl—)
Normally, the anion gap is 8-16 mmol/l.
Some hospital laboratories include K+ when calculating the anion gap. If K+ is included, the normal range is 12-20 mmol/L.
The main causes of acidosis with a high anion gap (more than 16 mmol/l) are given in Table 3.
Table 3. Main causes of acidosis with a high anion gap (more than 16 mmol/l)
| Increased production of endogenous acids |
|
| Increase in the amount of exogenous acids |
|
| Inability to excrete acids |
|
The main causes of acidosis with a normal anion gap (8-16 mmol/l), as a rule, are associated with an increase in plasma Cl- levels and are presented in table 4.
Table 4. main causes of acidosis with normal anion gap (8-16 mmol/l)
| Loss of bicarbonate |
|
| Impaired renal acid excretion |
|
How to correct the anion gap in patients with low albumin concentration?
Of the 8-16 mmol/L anion gap, as a rule, 11 mmol/L is due to albumin. Decreasing albumin concentration may reduce the initial anion gap. A patient with a low albumin concentration may have a normal anion gap in the presence of pathology that is usually accompanied by an increased anion gap.
The anion gap decreases by approximately 2.5 mmol/L for every 10 g/L decrease in albumin levels.
Step 4: Is there compensation?
Compensation means the body's reaction aimed at restoring normal acid-base balance. Standard compensation measures are:
- Buffers that include hemoglobin, plasma proteins, bicarbonate and phosphate. This reaction occurs within a few minutes.
- A respiratory response that develops over a period of minutes to several hours
- A kidney reaction that may develop over several days.
Why is recognizing compensation important?
Recognizing compensation will help you differentiate between the primary disorder and blood gas abnormalities that arise only from the primary disorder. For example, a hyperventilating patient who reduces pCO2 levels solely to compensate for metabolic acidosis likely has partially compensated metabolic acidosis rather than primary respiratory alkalosis.
Although patients with isolated mild disorders and fully compensated patients may have a pH in the normal range (7.35-7.45), a normal pH and abnormal HCO3- and pCO2 should lead you to suspect a mixed acid-base disorder.
It may be difficult for you to decide whether acid-base abnormalities are caused by a mixed disorder or just compensation. It is advisable to be aware of the possible degree of compensation for the primary disorder. If the change in one parameter is beyond the expected changes, then there is likely a mixed disorder (see Table 5). Compensatory reactions in metabolic disorders are not as predictable as in respiratory disorders.
Table 5. Summary: Compensatory Responses
| Acid-base imbalance | Primary chemical change | Compensatory reaction | Amount of compensation |
| Respiratory acidosis | ↑ pCO2 | ↑ HCO3— | For every 1.3 kPa increase in pCO2 above 5.3 kPa in acute respiratory acidosis:
For every 1.3 kPa increase in pCO2 above 5.3 in chronic respiratory acidosis:
|
| Respiratory alkalosis | ↓pCO2 | ↓HCO3— | For every 1.3 kPa decrease in pCO2 level below 5.3 kPa in acute respiratory alkalosis:
For every 1.3 kPa decrease in pCO2 level below 5.3 kPa in chronic respiratory alkalosis:
|
| Metabolic acidosis | ↓HCO3— | ↓pCO2 | |
| Metabolic alkalosis | ↑ HCO3— | ↑ pCO2 |
Compensation always occurs in the same direction as the primary chemical change. This is because compensatory reactions are based on maintaining the ratio of HCO3- to pCO2 concentration. Remember the Henderson-Hasselbach relationship: pH ~ HCO3-/pCO2.
In chronic disorders, the amount of compensation is greater, with further more effective pH maintenance. Knowing about possible changes in the metabolic compensation of primary respiratory disorders, it will be easier for you to diagnose mixed acid-base imbalances.
Metabolic compensation
Metabolic compensation takes several days. It occurs in two stages:
- Cellular buffering that occurs within minutes or hours. This only slightly increases plasma bicarbonate (HCO3—) levels.
- Renal compensation, which occurs within three to five days.
As a result, different types of responses are observed in acute and chronic disorders.
- In respiratory acidosis, renal excretion of carbonic acid and reabsorption of bicarbonate are increased.
- Respiratory alkalosis of the kidney is compensated by reducing bicarbonate reabsorption and ammonium excretion
Respiratory compensation
Respiratory compensation lasts for hours. Maximum respiratory compensation for metabolic disorders lasts from 12 to 24 hours. This reaction begins within the first hour and ends within 12 to 24 hours.
- In metabolic acidosis, stimulation of central and peripheral chemoreceptors that control breathing leads to an increase in alveolar ventilation. This, in turn, causes compensatory respiratory alkalosis
- In metabolic alkalosis, it is difficult to provide hypoventilation for the purpose of compensation. With hypoventilation, oxygenation is also impaired. Therefore, the respiratory system rarely maintains pCO2 above 7.5 kPa. A large value indicates a mixed disorder: it is more likely a metabolic alkalosis with respiratory acidosis, rather than a compensated metabolic alkalosis
Mixed acid-base balance disorders
Mixed acid-base imbalance occurs when more than one primary acid-base imbalance is present at the same time. They often occur in patients in hospital. With a good knowledge of compensatory mechanisms and the degree of compensation, you will be able to identify these disorders. Please note. that it is impossible to have both respiratory alkalosis and respiratory acidosis.
You should suspect mixed acid-base imbalance when:
- A compensatory reaction develops, but the level of compensation is insufficient or too pronounced
- pCO2 and HCO3- concentration deviate from the norm in opposite directions (one increases while the other decreases). In simple acid-base imbalances, the direction of the compensatory response always coincides with the primary chemical pathological change
- The pH is normal, but the pCO2 or HCO3 concentration is abnormal. In simple acid-base imbalances, the compensatory response rarely returns the pH to normal levels. In this case, a mixed disorder should be suspected
As a general rule:
- When pCO2 is elevated and HCO3- concentration is decreased, respiratory acidosis and metabolic alkalosis occur simultaneously.
- If pCO2 is reduced and the concentration of HCO3 is increased, then there is simultaneously respiratory and metabolic alkalosis.
Step 5: Ahh Gradient
What is the alveolar-arterial gradient?
A-and the gradient is the difference between the calculated alveolar pO2 and the measured arterial pO2. Arterial pO2 is a function of gas exchange and fractional inspired air O2 concentration (FiO2). Therefore, the normal range varies.
Calculation of Aa allows you to determine whether the measured arterial oxygen value is normal for the patient:
- Height
- Percentage of inspired oxygen
- Breathing rate.
This provides bedside assessment of gas exchange.
This allows you to calculate the efficiency of oxygen getting from the alveoli into the arterial bloodstream. Alveolar pO2 is always higher than arterial pO2. In healthy people, the gradient is 2-4 kPa. An increased gradient indicates a violation of gas exchange, since values above 4 kPa are pathological.
Getting Aa gradient
When breathing air at sea level, the partial pressure of inhaled oxygen is 21 kPa. It decreases to 20 kPa when saturated with water vapor from the upper respiratory tract (PiO2). In the alveoli, O2 is absorbed and replaced by CO2, which further reduces alveolar pO2 to ~13-14 kPa.
The ratio of pCO2 produced to pO2 consumed is determined by the respiratory coefficient. Its value is 0.8. Therefore, alveolar pO2 is calculated by subtracting alveolar pCO2 from PiO2. The pCO2 value increases slightly due to the respiratory coefficient.
Alveolar pO2 = inspiratory pO2 - alveolar pCO2 / 0.8 = inspiratory pO2 - alveolar pCO2 x 1.2
Since alveolar pCO2 is approximately equal to arterial pCO2, then:
Alveolar pO2 = inspiratory pO2 - arterial pCO2 x 1.2.
Since the Aa gradient is the difference between the calculated alveolar pO2 and the measured arterial pO2, you can calculate the gradient in kPa by subtracting the arterial pO2 from the calculated alveolar pO2:
- Alveolar pO2 = PiO2 - arterial pCO2 x 1.2
- Aa gradient = alveolar pO2 - arterial pO2
- PiO2 = effective inspiratory pO2.
Common acid-base disorders
Respiratory acidosis
It is a clinical disorder caused by alveolar hypoventilation (i.e., respiratory failure). Ineffective ventilation quickly leads to elevated arterial pCO2. The main reasons are presented in Table 6.
Table 6. Main causes of respiratory acidosis
| Central depression of the activity of the respiratory center |
|
| Neuromuscular disorders that cause weakness of the respiratory muscles |
|
| Pathologies of the chest wall or chest |
|
| Diseases that affect gas exchange |
|
| Airway obstruction |
|
Respiratory alkalosis
It is a clinical disorder that is caused by alveolar hyperventilation. Respiratory alkalosis can be acute or chronic. The main reasons are presented in Table 7.
Table 7. Main causes of respiratory alkalosis
| Central nervous system stimulation |
|
| Hypoxemia or tissue hypoxia |
|
| Lung disease |
|
| Medicines (respiratory stimulants) |
|
Metabolic acidosis
It is a clinical disorder characterized by a relative increase in the total acid content in the body. You should consider conditions that may be a sign of an underlying disease that is affecting the body. Determining this underlying disease is key to initiating appropriate therapy.
There are two types of metabolic acidosis:
- With high anion gap
- With normal anion gap.
Metabolic alkalosis
It is a relatively common clinical problem. It is characterized by high levels of bicarbonate. The main reasons are presented in Table 8.
Table 8. Main causes of metabolic alkalosis
| Loss of hydrogen ions |
|
| Intracellular redistribution of hydrogen |
|
| Excretory alkalosis |
Note:
|
List of sources
- bmj learning
- Martin L. All you really need to know to interpret arterial blood gases. Lippincott, Williams, and Wilkins, 1999.
- Thillai M & Hattotuwa K. Pocket Tutor Understanding ABGs & Lung Function Tests. JP publishing, 2011.
- Hennessey I & Japp A. Arterial blood gases made easy. Elsevier, 2015.
5 1 vote
Article rating
Pressure standards
The rate of partial pressure of oxygen in the blood is a relative concept, since it can vary depending on many factors. In order to correctly determine your diagnosis and receive treatment, you must contact a specialist with test results who can take into account all the individual characteristics of the patient. Of course, there are also reference standards that are considered ideal for a healthy adult. So, in the patient’s blood without abnormalities there is:
- carbon dioxide in the amount of 44.5-52.5%;
- its pressure is 35-45 mm Hg. Art.;
- liquid oxygen saturation 95-100%;
- O2 in the amount of 10.5-14.5%;
- partial pressure of oxygen in the blood is 80-110 mm Hg. Art.
In order for the results to correspond to reality during the analysis, it is necessary to take into account a number of factors that can affect their correctness.
Methodological manual on pulse oximetry. Part 1
This article presents information from a manual on pulse oximetry: “Diagnostic capabilities of non-invasive monitoring of arterial blood hemoglobin oxygen saturation in the clinic of internal diseases: method.recommendation. / D.V. Lapitsky [and others]. – Minsk: BSMU, 2015. – 71 p.”
Intended for doctors of therapeutic specialties, 5th-6th year students of the Faculty of Medicine, clinical residents, interns.
1. Basics of the pulse oximetry method.
In the physiology of respiration, it is customary to distinguish two key processes: cellular (tissue) respiration and external respiration (gas exchange) [1,2]. Cellular respiration is the process by which the cell releases energy from carbohydrates, fats and proteins [3]. External respiration ensures the supply of oxygen to the body for use in the biological oxidation of organic substances (i.e., in the process of cellular respiration), and the removal of the product of this oxidation, carbon dioxide, from the body. Thus, arterial blood can be represented as a link between external and internal respiration. The gas composition of arterial blood reflects the efficiency of external respiration and allows us to indirectly predict the risk of developing tissue hypoxia. Based on these positions, the diagnostic value of assessing the gas composition of arterial blood becomes clear.
The study of the gas composition of alveolar gas and arterial blood was initiated by the English physiologist John Scott Haldane at the beginning of the 20th century. Advances in science and technology over the past century have made it possible to formulate a coherent theory of gas exchange and to design instruments (for example, Radiometer Medical ApS, Denmark) for determining gases in samples of exhaled air, arterial and venous blood [4,5]. However, this examination requires stationary equipment and is invasive.
For the needs of practical and applied medicine, a method for quickly and non-invasively assessing the oxygen status of arterial blood is required. The search for such a method has been carried out since the 30s of the 20th century. In 1940, the first hemoximeter was designed to detect hypoxemia in pilots during flight. The developed equipment was bulky and required complex maintenance. These circumstances were the reason for the limited use of hemoximeters in clinical practice. The development of technology made it possible already in 1975 to launch the first mobile non-invasive pulse oximeter on the market, allowing long-term monitoring of arterial blood hemoglobin oxygen saturation.
The pulse oximetry method is based on two key physiological phenomena:
- The ability of hemoglobin, depending on its oxygenation, to absorb light of a certain wavelength to varying degrees when this light passes through a section of tissue (oximetry).
- Ripple of arteries and arterioles in accordance with the stroke volume of the heart (pulse wave).
The principle of oximetry is as follows. Deoxyhemoglobin (non-oxygen hemoglobin - RHb) absorbs red light intensely and weakly blocks infrared light. Oxyhemoglobin (fully oxygenated hemoglobin, each molecule of which contains four molecules of oxygen - HbO2) absorbs infrared radiation well, weakly retaining red radiation. Based on the ratio of red (R) and infrared (IR) fluxes that reached the photodetector from the radiation source through a section of tissue (for example, earlobe, finger), the degree of saturation of blood hemoglobin with oxygen is determined - saturation, SO2 (Fig. 1).
Rice. 1 The principle of oximetry (explanations in the text).
A pulse wave is formed as a result of pulsation of arteries and arterioles caused by the release of a certain volume of blood (stroke volume) into the aorta by the left ventricle. Each pulse wave leads to a rhythmic, in time with the heartbeat, change in blood supply to the tissue area under study. The result of recording such fluctuations in blood supply is a photoplethysmogram (PPG). PPG analysis allows you to determine the heart rate and assess the quality of peripheral blood flow (Fig. 2). In various clinical situations, the PPG amplitude can change tens of times. PPG allows you to get a fairly accurate impression of local blood flow. A decrease in PPG amplitude is a sign of peripheral vasoconstriction and/or a decrease in stroke volume, while an increase in amplitude indicates the opposite. Vascular tone is the main factor determining the height of PPG waves.
Rice. 2 Photoplethysmogram.
Another important advantage of recording a photoplethysmogram is the ability to isolate the portion of the intensity of the light flux that is absorbed directly by hemoglobin in arterial blood. When light passes through a section of tissue, it encounters various obstacles, which can be divided into several layers (Fig. 3). Layer 1 is tissue (skin, subcutaneous tissue, nail, bone), layer 2 is capillary and venous blood, layer 3 is blood remaining in the arterioles at the end of each pulsation, a kind of “end-systolic volume” of the arterial bed, layer 4 - additional volume of arterial blood flowing into the arterioles during cardiac systole.
Rice. 3 Absorption of light fluxes from LEDs by various tissues (explanation in the text).
At the moment preceding cardiac contraction, the weakening of light fluxes is due to the first three layers: radiation falls on the photodiode, which is regarded as background. When the next pulse wave reaches the arteries, the volume of blood in them increases and the absorption of light changes. At the peak of the pulse wave, the difference between the background and current radiation becomes maximum. The photodetector measures this difference and believes that it is caused by the additional amount of arterial blood that appears in the path of the radiation. This information is sufficient to use a special algorithm to calculate the degree of oxygen saturation of hemoglobin in arterial blood - SaO2, which is designated as SpO2 when measured with a pulse oximeter.
Thus, the use of one measurement principle (tissue transillumination) allows one to determine three diagnostic parameters at once: the degree of oxygen saturation of hemoglobin in arterial blood (SpO2), heart rate, and the volumetric amplitude of blood filling of a tissue area. Since the measurement is carried out by transilluminating tissue, this method is called “transmission pulse oximetry”. The vast majority of pulse oximeters used in medical practice operate based on this method.
Medical personnel who use pulse oximeters in daily activities need to be aware of the disadvantages and limitations of the pulse oximetry method. Pulse oximetry is an indirect method of assessing ventilation and does not provide information on the pH level, oxygen tension (PaO2) and carbon dioxide (PaCO2) in arterial blood. For practical work, it is useful to know that SpO2 indicators correlate with the partial pressure of oxygen in the blood: a decrease in PaO2 entails a decrease in SpO2. This dependence is nonlinear, which is explained by the S-shaped shape of the oxyhemoglobin dissociation curve (Fig. 4):
- 80-100 mm Hg. Art. PaO2 corresponds to 95–100% SpO2;
- 60 mmHg Art. PaO2 corresponds to 90% SpO2;
- 40 mmHg Art. PaO2 corresponds to 75% SpO2.
In addition, a number of factors can have a negative impact on the accuracy of measurements:
- bright external light and movements may interfere with the operation of the device;
- incorrect placement of the sensor: for transmission oximeters it is necessary that both parts of the sensor are symmetrical relative to the area of tissue being illuminated, otherwise the path between the photodetector and the LEDs will be unequal, and one of the wavelengths will be “overloaded”;
- a significant decrease in peripheral tissue perfusion leads to a decrease or disappearance of the pulse wave. In this situation, the SpO2 measurement error increases;
- at SaO2 values below 70%, the error in saturation measurements using pulse oximetry – SpO2 – also increases. In this regard, it should be noted that in the practical work of a physician in a therapeutic specialty, the probability of encountering SaO2 values below 70% in a patient is extremely low;
- anemia requires higher levels of oxygen to support oxygen transport. With hemoglobin values below 50 g/l, 100% blood saturation can be observed even with a lack of oxygen;
- carbon monoxide poisoning (high concentrations of carboxyhemoglobin can give a saturation value of about 100%);
- dyes, including nail polish, can cause an underestimated saturation value;
- cardiac arrhythmias may interfere with the pulse oximeter's perception of the pulse signal;
- age, gender, jaundice and dark skin color do not affect the operation of the pulse oximeter.
It is the simplicity and non-invasiveness of assessing the quality of peripheral blood flow and oxygen saturation of hemoglobin in arterial blood, as well as the ability of monitor systems to conduct arbitrary long-term monitoring of these parameters, that have contributed to the spread of the pulse kimetry method in departments of anesthesiology and intensive care/resuscitation for monitoring patients in severe conditions. At the same time, specially developed algorithms suppress excessive tissue pulsation, tissue scattering of the light flux and reduce the influence of external lighting and other artifacts on the device readings, making the readings reliable and suitable for systematic analysis.
2. Parameters of arterial blood oxygenation.
The quality of arterial blood oxygenation is assessed by the following indicators [6,7]:
1. PaO 2
– oxygen tension in arterial blood, mm Hg.
Art. PaO2 is the pressure required to keep oxygen in the arterial blood dissolved. The higher this indicator, the more oxygen is contained in the blood and the higher the pressure gradient, which determines the rate of movement of oxygen from capillary blood into tissues. Normally, PaO2 is 92-98 mm Hg. Art. and is measured in laboratory conditions in a microsample of arterial blood;
2. SaO 2
– degree of oxygen saturation of hemoglobin in arterial blood, %.
SaO2 depends on PaO2. The relationship between PaO2 and SaO2 is regulated by several physiological factors (carbon dioxide tension in arterial blood - PaCO2, blood acidity - pH, body temperature, etc.) and is expressed by an S-shaped oxyhemoglobin dissociation curve (Fig. 4). Normal values for this indicator are 95–99% and can be obtained in a microsample of arterial blood. This parameter is measured by a pulse oximeter. It is designated SpO2.
3. P 50
– blood oxygen tension at its half-saturation with oxygen (SO 2 = 50%), mm Hg.
Art. This indicator is determined in a microsample of arterial blood and reflects the affinity of hemoglobin for oxygen. Normal values for this indicator are 26 – 27 mmHg. Art. A decrease in the P50 value corresponds to a shift of the oxyhemoglobin dissociation curve to the left and, accordingly, an increase in the affinity of hemoglobin for oxygen; an increase in P50 indicates a shift of the oxyhemoglobin dissociation curve to the right with a decrease in the affinity of hemoglobin for oxygen (Fig. 4).
4. CaO 2
– oxygen capacity of the blood, reflecting the amount of oxygen in arterial blood, ml/l.
As a rule, this indicator is obtained by calculation. Oxygen is contained in the blood in a dissolved state and in a reversible connection with hemoglobin. The solubility constant of oxygen in arterial blood is 0.031 ml for every 1 mmHg. Thus, the product - 0.031 × PaO2 - represents the amount of oxygen dissolved in arterial blood. One gram of fully oxygenated hemoglobin contains 1.39 ml of oxygen. However, taking into account the correction for pathological hemoglobins (carboxyhemoglobin, methemoglobin), this figure is taken as 1.34 ml/g. The amount of oxygen attached to hemoglobin (Hb) is calculated as 1.34×Hb×SaO2/100 (ml/l). Thus, the oxygen capacity of arterial blood is equal to:
(*) CaO 2
(ml/l) = 1.34 × Hb × SaO 2 /100 + 0.031 × PaO 2 .
Normal values for this indicator are 180 – 204 ml/l.
CaO2 can be estimated using SpO2 values. Due to the fact that the pulse oximetry method does not allow estimating PaO2, the second component of the right side of the equation (*) - 0.031×PaO2 - is ignored. At the same time, CaO2 will decrease insignificantly – from 1.5 to 3.0 ml/l. Thus, equation (*) for a pulse oximeter is written:
CaO 2
(ml/l) = 1.34 × Hb × SaO 2 /100.
Rice. 4. Oxyhemoglobin dissociation curve.
Go to part two
Causes of deviation from the norm, depending on the patient
The partial pressure of oxygen in arterial blood can change very quickly depending on various circumstances, therefore, in order for the test result to be as accurate as possible, the following features should be taken into account:
- the pressure rate always decreases with increasing age of the patient;
- during hypothermia, oxygen pressure and carbon dioxide pressure decrease, and the pH level increases;
- when overheating the situation is reversed;
- the actual partial pressure of gases will only be visible when blood is taken from a patient with a body temperature within the normal range (36.6-37 degrees).
Reasons for deviations from the norm depending on health workers
In addition to taking into account such characteristics of the patient’s body, specialists must also comply with certain standards to ensure correct results. First of all, the partial pressure of oxygen is affected by the presence of air bubbles in the syringe. In general, any contact of the analysis with ambient air can change the results. It is also important, after collecting blood, to carefully mix it in a container so that red blood cells do not settle at the bottom of the tube, which can also affect the test results showing hemoglobin levels.
It is very important to adhere to the time standards allotted for the analysis. According to the rules, all actions must be carried out within a quarter of an hour after collection, and if this time is not enough, then the container with blood must be placed in ice water. This is the only way to stop the process of oxygen consumption by blood cells.
Specialists should also calibrate the analyzer in a timely manner and take tests only with syringes containing dry heparin, which is electrolytically balanced and does not affect the acidity of the sample.
How is the procedure done?
There is no special preparation for the procedure. Patients are not given any restrictions on drinking or eating before the test. The oxygen concentration should remain constant for 20 minutes before analysis; if the test is to be performed without oxygen saturation, the gas should be turned off for 20 minutes before the test is performed. The patient should breathe normally during the test. A blood sample is obtained by arterial puncture (usually in the wrist, although it can be done in the groin or arm). If a puncture is required, the skin over the artery is cleaned with an antiseptic. The healthcare professional then collects the blood using a small, sterile needle attached to a disposable syringe. The patient may feel a short pulsation or cramp at the puncture site. Once the material has been collected, it should be transported to the laboratory for analysis as soon as possible.
After the blood has been drawn, the doctor or patient presses cotton wool against the puncture site for 10-15 minutes to stop the bleeding, and then wraps it tightly with a bandage. The patient should rest quietly after completing the procedure. Health care providers will watch for signs of bleeding or circulation problems. The risks of getting them when the test is performed correctly are very low. Includes bleeding or bruising at the site of blood donation or after some time. Very rarely there may be a problem with circulation in the puncture area.
Test results
As is already clear, the partial pressure of oxygen in the air can have a noticeable effect on the human body, but the level of gas pressure in the blood can be disturbed for other reasons. To determine them correctly, decoding should be trusted only to an experienced specialist who can take into account all the characteristics of each patient.
In any case, hypoxia will be indicated by a decrease in oxygen pressure. Changes in blood pH levels, as well as carbon dioxide pressure or changes in bicarbonate levels, may indicate acidosis or alkalosis.
Acidosis is a process of acidification of the blood and is characterized by an increase in carbon dioxide pressure, a decrease in blood pH and bicarbonate levels. In the latter case, the diagnosis will be announced as metabolic acidosis.
Alkalosis is an increase in blood alkalinity. This will be indicated by an increased pressure of carbon dioxide, an increase in the number of bicarbonates, and, consequently, a change in the pH level of the blood.
What is a blood gas analysis?
The test is performed using blood from an artery. It measures partial pressure and carbon dioxide in the blood, as well as oxygen content, oxygen saturation, bicarbonate content and blood pH. Oxygen in the lungs is transferred to tissues through the bloodstream, but only a small amount can actually be dissolved in arterial blood. The amount of this gas depends on the partial pressure of oxygen (the pressure that the gas exerts on the walls of the arteries). Therefore, partial pressure of oxygen testing actually measures how much of it is delivered to the lungs through the blood.
Carbon dioxide is released as a byproduct of cellular metabolism. Its partial pressure indicates how well the lungs eliminate this carbon dioxide. The rest of the oxygen, which does not dissolve in the blood, combines with hemoglobin, a protein and iron compound found in red blood cells. The oxygen measurement in the ABG assay shows how much oxygen combines with hemoglobin. An important indicator is oxygen saturation, which compares the amount of oxygen actually bound to hemoglobin and the total amount of oxygen.
Content:
- What is a blood gas analysis?
- How is the procedure done?
- Test results
- Analysis efficiency