Paroxysmal supraventricular tachycardia, abbreviated as PVT, is a type of arrhythmia. Accompanied by a heart rate (HR) from 140 to 220 or more beats per minute. It arises spontaneously and ends unexpectedly. The duration of PNT is at least three cardiac cycles, while maintaining a regular heart rhythm. The attack itself can last from a few seconds to several days.
PNT occurs due to disruption of the nervous regulation of cardiac activity or damage to other organs.
In the first case, excessive nerve stimulation leads to an increase in heart rate.
PNT can also occur in healthy people under the influence of certain factors:
- prolonged physical activity;
- stress;
- consumption of energy and stimulant drinks;
- bad habits.
In the case of organic damage, paroxysmal supraventricular tachycardia can be caused by:
- damage to the heart muscle due to ischemia, inflammation, intoxication;
- myocardial infarction;
- heart disease;
- pathology of the cardiac conduction system.
In addition to heart disease, other organs can affect paroxysmal supraventricular tachycardia. It is worth checking the functioning of the kidneys, lungs and gastrointestinal tract, especially if there are chronic or acute diseases.
What is paroxysmal tachycardia?
As a rule, attacks of paroxysmal tachycardia begin and end suddenly and have different durations.
They make the heart work uneconomically, reduce the efficiency of blood circulation, and lead to its failure. According to the mechanism of development and etiology, paroxysmal tachycardia resembles extrasystole. Therefore, cardiologists regard successive extrasystoles as a short attack of tachycardia.
Classification of paroxysmal tachycardia
1. Based on the location of ectopic impulses, doctors distinguish:
- atrial paroxysmal tachycardia;
- atrioventricular (atrioventricular) paroxysmal tachycardia;
- ventricular paroxysmal tachycardia.
In turn, atrioventricular and atrial tachycardia are combined into a supraventricular or supraventricular form.
2. Taking into account the nature of the course, the following types of paroxysmal tachycardia are distinguished:
- chronic (constantly recurrent);
- spicy;
- continuously relapsing (lasts for years, can cause circulatory failure and dilated, arrhythmogenic cardiomyopathy).
3. According to the characteristics of the development mechanism, paroxysmal supraventricular tachycardia is classified into:
- focal (ectopic);
- reciprocal (associated with the re-entry mechanism in the sinus node);
- multifocal (multifocal).
In children, paroxysmal tachycardia manifests itself in the same way as in adults.
Tachycardia and the army
To receive a deferment from service or even release, tachycardia alone is not enough. It is necessary to establish its cause.
A physiological heart rate disorder does not pose a health hazard and therefore cannot serve as an obstacle to military service. Another thing is pathological tachycardia.
Pathological heart rhythm disturbances occur in conscripts in 14% of cases. When passing a medical commission, a young person is assigned a heart electrocardiogram, but this may not be enough to make an accurate diagnosis. The fact is that tachycardia is not a regular phenomenon and can occur at any time during the day.
For a more accurate result, the conscript may be prescribed a Holter ECG procedure - 24-hour monitoring. The doctor will give the conscript a special device, which he will need to wear for 24 hours without removing it from his body.
This small device is most often attached to the arm, and many wires go from it to the chest, which read the heart rhythm. The procedure is absolutely painless, but may cause some discomfort to the conscript.
A day later, the data recorded on the device is transferred by the doctor to a computer and analyzed. Any, even the slightest, disturbances in the functioning of the heart that occur during the day will not go unnoticed.
Preparatory activities
The military registration and enlistment office is interested in receiving young conscripts, so they can simply turn a blind eye to minor (according to the medical board) tachycardia. But pathological disorders of the heart can be extremely dangerous to the health of a young man.
Before starting the medical examination, the conscript is advised to independently visit the necessary doctors and obtain certificates that could confirm his illness.
Causes of paroxysmal tachycardia
Supraventricular paroxysmal tachycardia occurs as a result of increased activation of the sympathetic nervous system. Ventricular is a consequence of necrotic, inflammatory, sclerotic or dystrophic damage to the heart muscle.
In the ventricular form, the focus of ectopic excitation is located in the His bundle, its legs and Purkinje fibers, that is, in the ventricular sections of the conductive nervous system. Most often, the pathology is diagnosed in elderly men who have suffered a myocardial infarction, coronary heart disease, or suffer from hypertension, myocarditis, or heart defects.
The main causes of the development of paroxysmal tachycardia also include:
1. The presence of additional innate impulse pathways in the myocardium. That is:
- Kent's bundle between the atria and ventricles, bypassing the atrioventricular node;
- Macheim fibers between the atrioventricular node and the ventricles.
2. The presence in the myocardium of additional impulse pathways resulting from myocardial damage (infarction, myocarditis, cardiomyopathy).
3. Additional pathways cause pathological movement of excitation throughout the myocardium.
Cardiology knows cases when longitudinal dissociation appears in the atrioventricular node, causing uncoordinated functioning of the fibers of the atrioventricular connection. Then some of the fibers function normally, while the other, on the contrary, conducts excitation in the retrograde (opposite) direction and acts as the basis for the circular circulation of impulses from the atria to the ventricles and along the opposite fibers back to the atria.
In young children, essential (idiopathic) paroxysmal tachycardia of unknown etiology is sometimes diagnosed.
Features of passing a medical examination
At the military registration and enlistment office, the medical commission does not diagnose diseases. They only identify pathologies and send the person to the hospital for a detailed examination. Therefore, it is better to prepare for visiting the military registration and enlistment office and collect the maximum package of documents confirming the presence of the disease.
IMPORTANT. The issue of deferment or complete exemption from the army can be resolved only if there is an established diagnosis, which is included in the list approved by Government Decree No. 565 of the Russian Federation.
Ivan Golubkin
Legal specialist and manager. Experience in the legal field - more than 10 years, in the field of assistance to conscripts - more than 3 years. Writes useful articles for conscripts.
Symptoms of paroxysmal tachycardia
An attack of paroxysmal tachycardia always begins and ends suddenly. Its duration can range from several minutes to several days. The patient feels an incomprehensible “push” in the area of the heart. Then the heartbeat increases sharply and reaches 120-220 beats/min. The correct heart rhythm is maintained.
Paroxysm may be accompanied by:
- noise in the head;
- dizziness;
- a feeling of squeezing of the heart.
In some cases, neurological focal symptoms occur - hemiparesis, aphasia.
Paroxysm of supraventricular tachycardia is often manifested by autonomic dysfunction, which is characterized by:
- nausea;
- sweating;
- flatulence;
- low-grade fever.
When the attack ends, polyuria (increased urine production) is observed after a few hours. If paroxysmal tachycardia is prolonged, blood pressure may decrease, severe weakness, and fainting may occur.
If you notice similar symptoms, consult a doctor immediately. It is easier to prevent a disease than to deal with the consequences.
Diagnosis of paroxysmal tachycardia
Paroxysmal tachycardia is recognized by the typicality of the attack (sudden onset and sudden end) and data obtained from a cardiac examination. The supraventricular and ventricular forms differ in the degree of increase in heart rate:
- with ventricular tachycardia, the heart rate is up to 180 beats/min, tests with excitation of the vagus nerve are negative;
- with supraventricular tachycardia, the heart rate is about 220-250 beats/min, the attack is easily stopped by excitation of the vagus nerve.
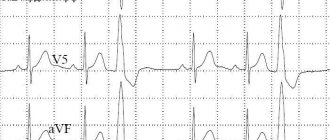
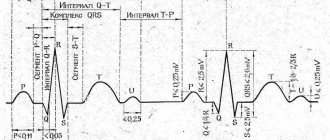
An ECG with paroxysmal tachycardia shows a change in the polarity and shape of the P wave, as well as a violation of its location in relation to the ventricular QRS complex. These signs allow us to judge what form of the disease we are talking about.
Thus, an ECG with atrial paroxysmal tachycardia shows the location of the positive/negative P wave in front of the QRS complex. If the paroxysm comes from the atrioventricular junction, a negative P wave is recorded, located behind/merging with the QRS complex. An ECG with ventricular paroxysmal tachycardia registers expansion and deformation of the QRS complex, and an unchanged P wave can also be recorded.
Paroxysmal tachycardia cannot always be detected using an ECG. Then cardiologists resort to daily ECG monitoring, which allows them to observe short episodes of attacks that are not subjectively felt by the patient.
In order to exclude organic cardiac pathology, the following are additionally carried out:
- MRI;
- Ultrasound of the heart;
- MSCT of the heart (layer-by-layer scanning of cardiac structures).
In some cases, an endocardial electrocardiogram is recorded by inserting electrodes into the heart.
Do they hire someone with tachycardia?
Whether a young man can be drafted into the armed forces or should be released from service for health reasons is decided by a military medical commission. It operates on the basis of the Schedule of Diseases - a document containing a list of pathologies that, from a medical point of view, are incompatible with the harsh everyday life of the army. Based on the results of the examination, each conscript receives a fitness category, which reflects his ability to serve in the army as a whole and to be drafted into one or another branch of the military.
Tachycardia is not considered a separate disease, so it is not on the list of the Schedule of Diseases. For draft board doctors, it represents only a symptom of a possible pathology that still needs to be determined. In other words, people with tachycardia are taken into the army if the reason that provoked it is not considered a serious reason for exemption from service.
Physiological tachycardia is absolutely not an obstacle to recruitment. It happens to everyone, passes quickly and does not pose a threat to health.
If the tachycardia is caused by a medical problem that can be quickly resolved, then the conscript will receive a deferment for treatment and restoration of health. It may also be given for additional examination.
Symptoms of tachycardia
It should be understood that the medical commission at the military registration and enlistment office does not make diagnoses; it only examines the young man’s ability to serve in the army. Therefore, the conscript should support complaints about frequent cases of tachycardia with documents that indicate a clear diagnosis and provide examination results. Without them, the person liable for military service will most likely go to the army. Typically, people with serious heart disease have a significant package of medical documents in hand, allowing them to easily prove their diagnosis.
At the medical commission, conscripts undergo electrocardiography, however, this diagnostic method does not provide a complete picture - the increase in heart rate may be episodic. A more accurate and effective method is daily monitoring of heart function, in which electrodes are attached to the patient’s body, and the cardiogram is recorded on a special device. This method allows not only to identify the slightest disturbances in the functioning of the cardiovascular system, but also to determine the nature of the disease, its severity, and sometimes indicate the cause of the pathology.
Sinus tachycardia and the army
Sinus tachycardia and army are completely compatible concepts. This pathology is not considered a valid reason for release from service. As a last resort, a conscript with a similar diagnosis can count on a “limited” category “B” or a six-month deferment for additional examination.
The verdict of the medical board will be different if tachycardia is a consequence of heart disease, diseases of the endocrine system, or heart failure. In this case, the conscript will most likely be sent for additional examination. If the diagnosis is confirmed and the underlying disease cannot be cured, the young man can count on being released from service with fitness category “B” or “D”.
Paroxysmal tachycardia and emergency service
The paroxysmal form of the pathology is much more dangerous than the sinus one - it manifests itself in the form of severe sudden attacks, which can be accompanied by fainting, pressure surges, heart pain, and general weakness.
Symptoms of paroxysmal tachycardia. It is often the result of dangerous heart problems.
During an attack, a person often needs medical care; to stop it, it is necessary to take medications. In addition, people suffering from such a pathology are required to follow a diet and avoid serious physical activity, which does not fit well with the army regime. But the main thing is different: usually paroxysmal tachycardia is a consequence of severe diseases of the cardiovascular and other body systems, which are indicated in the Schedule of Diseases as incompatible with service. Conscripts with such pathologies, as a rule, are well acquainted with their diagnosis and have documentary evidence of it. Therefore, they have minimal problems with passing the commission and obtaining the necessary fitness categories.
In the army with tachycardia: what to do
If a conscript does not agree with the fitness category that was given to him at the medical examination, he can appeal the verdict to a higher-ranking military commissariat or in court. The decision will be suspended during the trial.
Even while in military service, you can write a report addressed to the unit commander with a request to be sent to a hospital for additional examination. If during its passage a serious pathology is discovered in a serviceman that causes tachycardia, then he should be discharged.
People often ask whether it is possible to “refuse” from service with tachycardia? This is not a good idea. Firstly, it should be said right away that evading military duty is a violation of the law, for which you can be punished, and secondly, this diagnosis is not very suitable for those who want to avoid the army. He is not on the list of the Republic of Belarus; with tachycardia, he can be exempted from conscription only if he has other serious pathologies.
In order for doctors at the medical board to take your complaints of rapid heartbeat seriously, you need documentary evidence of similar problems in the past, preferably several years before conscription. In addition, in the case of heart diseases, doctors make a final verdict based on the results of the examination, which cannot be falsified. We must not forget that examinations of conscripts are carried out by experienced specialists who are well familiar with all the possible tricks of possible draft dodgers.
Bradycardia: is someone hired with such a disease?
Bradycardia is a pathology of heart rhythm in which the contraction frequency decreases to 30-50 beats per minute. The reasons for this condition may be different:
- disruption of the sinus node;
- pathologies of the endocrine system (hypothyroidism);
- increased intracranial pressure;
- poisoning;
- fasting or exposure to cold;
- excessive activation of the parasympathetic nervous system;
- taking medications.
Bradycardia can occur due to natural causes. For example, a low heart rate is the norm for trained athletes. Bradycardia can be caused by taking medications. If a decrease in heart rate is not accompanied by other pathological manifestations, then it is not considered a disease. However, it may be different: a significant decrease in heart rate leads to oxygen starvation of tissues, primarily the brain. Symptoms of pathological bradycardia are:
- weakness;
- decreased performance;
- frequent dizziness;
- difficulty breathing and shortness of breath;
- fainting or lightheadedness.
Bradycardia itself is not grounds for exemption from service. You can get it only if the low pulse is the result of a serious illness: heart failure, thyroid dysfunction and myocarditis. Severe bradycardia is usually accompanied by heart failure, which is poorly combined with physical activity. If a young man experiences shortness of breath and fatigue while performing normal physical exercises, he will be released from conscription and assigned category “B.” For more serious heart rhythm disturbances, in which even light exercise is impossible, the young person receives category “D”.
Heart contractions in normal condition and with bradycardia
It can be added that it is difficult to obtain exemption from service due to bradycardia. Even if the conscript has the appropriate documents proving the presence of this problem in the past, he will still be sent for additional examination. And only after confirmation of the diagnosis can he count on the “non-conscription” category.
Treatment of paroxysmal tachycardia
The treatment regimen for paroxysmal tachycardia depends on:
- forms of arrhythmia (ventricular, atrial, atrioventricular);
- reasons that caused the disease;
- duration and frequency of paroxysms;
- presence/absence of complications.
Attacks of paroxysmal tachycardia require emergency hospitalization (with the exception of idiopathic variants with a benign course, which are easily stopped by administering an antiarrhythmic drug to someone).
For the treatment of the supraventricular form, complicated by cardiovascular or heart failure, patients are hospitalized in the cardiology department. Planned hospitalization is carried out if attacks recur more often than 2-3 times a month. Then the question of the relevance of surgical intervention is decided.
Emergency care for paroxysmal tachycardia includes intravenous administration of antiarrhythmic drugs (Propranolol, Aymalin, Rytmodan, Quinidine, Ethmozin, Cordarone, Isoptin, etc.). If the attack is prolonged and cannot be controlled with medications, electropulse therapy is performed. Then the patient undergoes outpatient cardiological treatment, during which effective antiarrhythmic drugs are selected.
To relieve paroxysmal tachycardia, doctors often use vagal maneuvers - techniques that have a pronounced mechanical effect on the vagus nerve. These include:
- straining;
- Aschner's test (moderate and uniform pressure on the inner upper corner of the eyeball);
- Valsalva maneuver (vigorous exhalation with the mouth and nasal cavity closed);
- irritating the root of the tongue to trigger a gag reflex;
- Chermak-Hering test (uniform pressure on the carotid sinuses in the area of the carotid artery).
If attacks of paroxysmal tachycardia occur several times a month, the patient is prescribed long-term anti-relapse therapy:
- quinidine preparations (Disopyramide, Kinylentine, Amiodarone, Verapomil, etc.);
- cardiac glycosides (Celanide, Digoxin).
The selection of an effective dosage is carried out taking into account the patient’s well-being and ECG results.
Surgical treatment of paroxysmal tachycardia is used only if the disease is severe and cannot be controlled with medications. Among the most common surgical methods are:
- mechanical, laser, electrical, cryogenic, chemical destruction of additional impulse pathways or ectopic foci of automatism;
- RFA;
- implantation of a pacemaker;
- implantation of an electrical defibrillator.
If a patient wants to treat paroxysmal tachycardia using traditional methods, he should first consult with a cardiologist, since failure to take prescribed antiarrhythmic drugs can lead to serious complications.
Prevention
Prevention lies in early diagnosis. Often, success directly depends on the patient and his attitude towards his health. Basic recommendations that should be followed during prevention:
- moderate regular physical activity;
- proper nutrition;
- rejection of bad habits;
- avoidance of situations that lead to stress and cause anxiety;
- compliance with the instructions of the attending physician.
The main thing is to diagnose tachycardia in a timely manner in order to move on to prevention in time. You can get acquainted with the programs of our center by following the link.
Diet for paroxysmal tachycardia
Patients with paroxysmal tachycardia should monitor blood sugar and cholesterol levels and maintain normal body weight. It is recommended that they take food in small portions 4-5 times a day. This is explained by the fact that overeating leads to irritation of the nerve receptors that are responsible for the functioning of the heart, and this is fraught with attacks of tachycardia.
You can't eat late at night. The last meal should be no later than 2-3 hours before going to bed. Exclude from the diet:
- coffee Tea;
- products containing large amounts of sugar, starch;
- sweets, baked goods;
- fatty foods (lard, mayonnaise, fatty meat, butter).