Heart muscle, unlike ordinary muscle tissue, is endowed by nature with special properties. It can contract independently of the brain signal and the regulatory influence of the neurohumoral system.
The correct path (nomotopic) for receiving information begins in the right atrium (in the sinus node) and passes to the border atrioventricular node with subsequent distribution along the septum. All other contractions occur arbitrarily and are called ectopic rhythm (heterotopic).
According to the classification of arrhythmias, ectopic rhythm disturbances are divided into:
- by localization of foci of excitation;
- their numbers;
- time in relation to the phases of heart contractions;
- types and nature of manifestations.
Ectopic arrhythmia accompanies many heart diseases in children and adults. It often occurs without symptoms and does not require treatment. The main detection method is electrocardiography (ECG). It allows you to detect “unruly” lesions and monitor the results of treatment. If long-term monitoring is necessary, Holter monitoring is used.
What is atrial rhythm
Myocardial contractions normally occur regularly and do not depend on consciousness: even when the brain dies, the heart still works for some time.
This process is very important for maintaining life. Failures occur due to serious damage to the cell structure or metabolic disorders. If the main pacemaker is affected, its function passes to the underlying sections located in the atria, atrioventricular zone, and bundle branches. In this case, the normal impulse becomes too weak or absent. If the generation of myocardial contractions comes from the atria, then in this case an atrial ectopic rhythm is recorded on the ECG.
Diagnosis of ectopic rhythm
The leading diagnostic method is the electrocardiogram. If an ectopic rhythm is detected on the ECG, the doctor should prescribe a further examination plan, which includes cardiac ultrasound (ECHO-CS) and daily ECG monitoring. In addition, patients with myocardial ischemia are prescribed coronary angiography (CAG), and patients with other arrhythmias are prescribed transesophageal electrophysiological examination (TEPE).
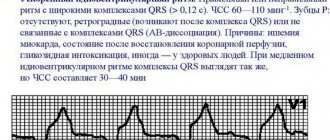
ECG signs for different types of ectopic rhythm differ:
- With an atrial rhythm, negative, high, or biphasic P waves appear, with a right atrial rhythm - in additional leads V1-V4, with a left atrial rhythm - in V5-V6, which may precede or overlap the QRST complexes.
accelerated ectopic atrial rhythm
- The rhythm from the AV junction is characterized by the presence of a negative P wave, superimposed on the QRST complexes, or present after them.
AV nodal rhythm
- Idioventricular rhythm is characterized by a low heart rate (30-40 per minute) and the presence of altered, deformed and widened QRST complexes. There is no P wave.
idioventricular (ventricular) ectopic rhythm
- With atrial extrasystole, premature, extraordinary, unchanged PQRST complexes appear, and with ventricular extrasystole, altered QRST complexes appear followed by a compensatory pause.
atrial and ventricular ectopia (extrasystoles) on the ECG
- Paroxysmal tachycardia is characterized by a regular rhythm with a high frequency of contractions (100-150 per minute), P waves are often quite difficult to determine.
- Atrial fibrillation and flutter on the ECG are characterized by an irregular rhythm, the P wave is absent, and fibrillation f waves or flutter waves F are characteristic.
Causes and types
The main causes of atrial, as well as any ectopic (displaced) rhythm, are:
- Changes in the structure of the myocardium - as a result of inflammation, ischemia, cardiosclerosis, hypertrophy or dystrophy.
- Valve defects and other congenital anomalies.
- Violation of electrolyte and water levels. This happens with a sudden loss of fluid (vomiting, diarrhea, taking diuretics).
- Metabolic changes in diseases of the endocrine organs.
- Internal or external intoxication (impaired kidney and liver function, smoking, alcoholism, drug addiction, ingestion of heavy metal salts, etc.).
- Overdose of cardiac glycosides.
- Traumatic chest injury.
All these reasons are characteristic of ectopic atrial impulses in an adult. In children and adolescents, they most often occur against the background of impaired autonomic innervation.
Depending on the frequency of contractions, slow and accelerated atrial rhythms are distinguished. The lower the pacemaker is located in the conduction system, the rarer the pulse - up to 45–60 beats per minute. An increase of up to 130 or more occurs when, under the influence of inflammation or other pathology, hyperexcitation and excessive activity of the ectopic focus develop.
The displaced rhythm may be permanent or temporary. According to localization, it can be left or right atrial, but this division has no particular clinical significance and does not affect the prescribed treatment regimen.
Ectopic impulses can vary in frequency, regularity and strength. But in the absence of normal sinus rhythm, they allow the heart to continue pumping.
Migration of the pacemaker (MPM) through the atria is a well-known phenomenon consisting of varying the shape of the P wave, mainly in the limb leads, which, in turn, is caused by changes in the localization of the cardiac pacemaker. According to the mechanism of occurrence, escape (ectopic or heterotopic) complexes and rhythms from the lower parts of the right atrium, the atrioventricular (AV) junction, as well as rarely observed ectopic rhythms from the left atrium are closely related to MVR. Along with these centers of automaticity in the atria, obviously, there are mid-atrial centers of automaticity (MACA), localized in the middle sections of the right atrium [3,9,19], which probably do not play a significant backup role, since in the development of heart disease they, along with with the sinus node will be involved in the pathological process, and with the development of complete AV block, the manifestation of their activity will be meaningless. However, the term “mid-atrial rhythm” (MAR) is not very common in cardiology, which is probably due to the lack of clear electrocardiographic criteria to distinguish it from sinus rhythm. On the other hand, the structure of the conduction system localized in the atria is currently an incompletely resolved issue. According to the most common opinion [6,18], the propagation of the impulse from the sinus to the AV node occurs along specialized internodal tracts. At the same time, some histological studies [1,21] indicate that in the atria, except for the sinus and AV nodes, localized respectively in the upper part and the so-called “half” of the right atrium, there are no cells at all that can be attributed to the conduction system - propagation of the impulse from the sinus node to the AV junction occurs along the contractile myocardium, and the inferior atrial rhythm (IAR) or coronary sinus rhythm actually originates from the AV junction. However, some researchers believe that cells in many areas of the heart are normally capable of spontaneously generating impulses. These areas include the sinus node, specialized atrial fibers, coronary sinus, AV junction and valves, and the specialized ventricular conduction system; in heart diseases, the occurrence of an impulse can be observed almost everywhere, even in the working myocardium of the atria and ventricles [2]. One way or another, the concepts of “MVR” and “escaping supraventricular rhythms” have become firmly established in clinical cardiology. Such arrhythmias are generally considered to be relatively benign conditions that do not require special antiarrhythmic treatment, but their prevalence and clinical significance, including in adolescents, have not been studied.
Purpose of the study
The purpose of this work is to assess the prevalence and clinical significance of MVR and supraventricular escape rhythms in adolescents.
Materials and methods
We conducted an epidemiological clinical and electrocardiographic examination of 1242 adolescents aged 13.5-18.5 years in St. Petersburg (597 boys and 645 girls). All teenagers were students of schools, secondary and higher educational institutions in various districts of the city, and medical selection to the educational institutions where the survey was carried out was minimal, which, in our opinion, makes the surveyed sample representative. The examination included ECG recording in 12 standard leads (about 100 cardiac complexes were recorded), height and weight measurement, clinical examination, laboratory tests, echocardiography, and exercise testing if necessary. Due to the fact that there is a widespread opinion that MVR and slipping complexes can be associated with vegetative-vascular (neurocirculatory) dystonia (VSD) and to standardize the diagnosis, all adolescents were surveyed using a specially designed questionnaire for the presence of complaints characteristic of VSD (irritability, poor sleep, cardialgia, headaches, etc.). The diagnosis of VSD was established in the presence of corresponding subjective sensations, but in the absence of objective symptoms indicating organic damage to internal organs.
Results and its discussion
Escape complexes from the AV connection, combined with the phenomena of AV dissociation (Fig. 1), were found in 1 young man actively involved in sports - sports acrobatics (candidate for master of sports). This type of arrhythmia was diagnosed by the absence of a preceding P wave associated with the QRS complex. The teenager trained 4-5 times a week, the training duration was about 3 hours. This young man did not make any complaints about his health; no pathological abnormalities were identified during an objective examination. According to the recommendations for assessing the ECG of athletes, proposed by American and European cardiologists [15], such a rhythm disturbance should be considered as a normal variant in athletes. At the same time, in domestic sports cardiology there is an opinion that this type of arrhythmia should be regarded as a manifestation of myocardial dystrophy due to physical overexertion [4,12]. This is mainly due to the fact that this type of arrhythmia is rarely seen among athletes. We also adhere to this point of view. In addition, in this teenager, the intervals of slippage of nodal complexes were 1.04-1.08 s, which corresponds to a nodal rhythm frequency of 56-58 beats/min, and, therefore, such complexes must be considered accelerated [9]. In this regard, the presence of such arrhythmia in this young man was regarded as a manifestation of myocardial dystrophy of the 1st degree. The young man was recommended to change the nature of his training - temporarily limit the intensity of physical activity, increase the warm-up period and the final stage of training. The teenager complied with these recommendations. After 2 weeks, sinus arrhythmia was recorded on the ECG; no escape node complexes were recorded.
Certain difficulties were caused by electrocardiographic assessment of changes in heart rhythm associated with the manifestation of the activity of atrial centers of automaticity. In most ECG manuals, the criteria for MVR are usually taken to be a gradual change in the polarity of the P wave in lead II (and, accordingly, III, aVF) from positive to negative. Indeed, when the pacemaker is displaced from the sinus node to the lower atrial centers of automaticity (ICA), the impulses generated by the ICA will cause retrograde excitation of the atria, which will naturally lead to the appearance of negative P waves. Inferior atrial rhythms and complexes will also be characterized by negative P waves in leads II ,III,aVF. At the same time, when analyzing ECGs recorded during a population study, a certain part of adolescents showed a change in the P wave in lead II from positive to isoelectric and, accordingly, the configuration of the P wave in leads III, aVF changed from positive to slightly negative (Fig. 2).
Rice. 1. ECG of a young man M., 14 years old; continuous recording (in this and other figures, continuous recording is marked with a horizontal arrow); Lead II, recording speed 25 mm/s. Escape complexes from the AV junction (2, 5, 6, 8, 11, 12 complexes) with an escape interval of 1.04-1.08 s (corresponding to a heart rate of 56-58 beats/min.). In the 1st, 3rd, 4th, 7th, 9th, 10th, 13th and 14th complexes, normal AV conduction is noted; the heart rate in these cases is 60-88 beats/min.
Rice. 2. ECG of a young man D., 15 years old, recording speed 50 mm/s. MVR between the sinus node and SPCA: change in the shape of the P wave - from positive to smoothed in lead II, from positive to isoelectric in lead aVF, from positive to slightly negative in lead III; pronounced irregularity of heart contractions - fluctuations in the duration of the RR interval from 0.66 s to 1.04 s.
Such a change in the P wave is sometimes considered as MVR [10], sometimes as a variant of sinus arrhythmia [16,20]. In the latter case, the change in the morphology of the P wave is usually not explained or is associated with positional changes or variability in the conduction of the impulse through the atria during breathing. Indeed, changes in the amplitude and shape of waves during normal ECG recording are well known and are often observed in healthy adolescents [7]. They arise due to changes in the position of the heart in the chest during breathing and primarily concern the waves of the QRS complex. However, such a clear change in the P wave with a rhythm emanating from the sinus node is difficult to explain only by the above reasons without invoking the concept of SPCA. Obviously, with sinus arrhythmia, a slight change in the shape of the P wave is possible, due to a change in the position of the heart in the chest during breathing or variability in the conduction of the impulse from the sinus node to the AV junction. However, changes in the P wave in the form of its flattening often appear when holding the breath (Fig. 3).
Rice. 3. ECG in lead II of girl A., 15 years old, recording speed 25 mm/s. Complexes 1-4 were recorded during quiet breathing - sinus arrhythmia with fluctuations in the duration of the RR interval from 0.8 s to 0.98 s (the P wave does not change). Complexes 5-8 were recorded at the moment of inspiration (marked with a vertical arrow). Complexes 9-19 were recorded during breath-holding at the height of inspiration, of which complexes 9-16 are of sinus origin (the P wave does not change and remains identical in comparison with the P wave during quiet breathing and at the moment of inspiration); complexes 17-19 – midatrial – the P wave is flattened.
A more detailed examination of adolescents who showed flattened P waves on the resting ECG (more precisely, provided that ∠ α of the P wave ranges from 30° to -30°) made it possible to confirm the assumption that in fact they have an SPR, although according to formal signs such the rhythm is traditionally regarded as sinus.
Rice. 4. ECG of a young man L., 16 years old - before (a), immediately after (b) and after 6 minutes. after physical activity (c). Recording speed 50 mm/s. Explanation in the text.
In Fig. Figure 4 shows the ECG of a healthy teenager before and after physical activity (load power 75 W, duration 3 minutes). To exclude the influence of body position, ECGs were recorded in the supine position. On the initial ECG (a) – SPR∠ α P wave 10°: smoothed P in leads II, aVF; weakly negative P in lead III; heart rate (HR) – 81 beats/min. On the ECG (b), taken immediately after physical activity - sinus rhythm - ∠ α P wave 70°: positive P in leads II, III, aVF; Heart rate – 120 beats/min. On the ECG (c), recorded after 6 minutes. after the load – SPR, similar to that recorded before the load, heart rate – 65 beats/min. In Fig. Figure 5 shows ECG recorded during a clinoorthostatic test also in a healthy teenager. On the initial ECG, taken in the supine position (a), the SPR was recorded – ∠ α P wave 25°; Heart rate – 66 beats/min. In a standing position (b) there is a clear increase in the amplitude of the P wave, obviously due to the transition to sinus rhythm with a heart rate of 88 beats/min. On the ECG taken after returning to a horizontal position (c) - the first 2 complexes are of sinus origin (P waves of large amplitude), 4, 5, 6, 7 and 8 complexes are mid-atrial (P waves are flattened and correspond to the P waves on the original ECG).
Rice. 5. ECG of a young man V., 16 years old, during a clinoorthostatic test: a) in a supine position; b) in a standing position; c) after returning to a horizontal position; recording speed 50 mm/s. Explanation in the text.
It must be recognized that the increase in the amplitude of the P wave in these cases can be explained by an increase in the tone of the sympathetic nervous system, which is naturally observed during physical activity or transition to a vertical position, however, the increased tone of the sympathetic system in itself is not capable of causing a significant (60°) change position of the total vector of atrial depolarization. At the same time, this fact can be easily explained using the concept of SPR - with a rhythm emanating from the middle sections of the right atrium, the depolarization of the upper and partially middle sections of the atria will be carried out retrograde, which will lead to a deviation of the total vector of atrial depolarization up and to the left. To confirm this position, 16 adolescents whose resting ECG ∠ α P wave was more than 30° underwent exercise testing. On ECGs taken after exercise, there was a slight increase in the P wave and sometimes a slight increase in ∠α of the P wave, not exceeding 20°, which indicates a single pacemaker - the sinus node. On the contrary, when performing exercise tests on adolescents whose initial ECG ∠ α P wave was less than 30° (28 people were examined), a sharp deviation of the total vector of atrial depolarization to the right (more than 30°) was observed for a more or less long period of time .
In connection with the above, the following types of atrial heterotopic arrhythmias have been identified in adolescents.
1. MVR between the sinus node and the NPCA (between the sinus node and the lower parts of the atria) - was diagnosed when an ECG detected a change in the polarity of the P wave in lead II (and, accordingly, in leads III, aVF) from positive to negative.
2. Inferior atrial rhythms and complexes - were diagnosed in the presence of a negative P wave in leads II (and, accordingly, in leads III, aVF) before the QRS complex, ∠ α of the P wave in such a rhythm was respectively less than -30°, but more than -90°.
3. MVR between the sinus node and SPCA (between the sinus node and the middle parts of the atria) - was diagnosed when the shape of the P wave in lead III changed from positive to (weakly) negative; Accordingly, in lead II, the amplitude of the P wave also changed - from positive to smoothed or isoelectric, in lead aVF - to isoelectric or slightly negative.
4. SPR – was diagnosed if ∠ α of the P wave was less than 30°, but ≥ -30°. This was manifested in the presence of negative P waves in lead III, smoothed P waves in lead II, and smoothed or weakly negative P waves in lead aVF.
The first 2 types of arrhythmias can be combined into a group of arrhythmias associated with the manifestation of NPCA activity, the second 2 types - into the group of arrhythmias associated with the manifestation of SPCA activity. There are no changes in the P wave in the chest leads during arrhythmias associated with the manifestation of SPCA activity; in case of arrhythmias associated with the manifestation of NPCA activity, changes in the P wave in the chest leads are inconsistent and unexpressed - weakly negative P waves may appear in leads V4 - V6 or in all chest leads. No left atrial rhythms were detected in our study.
Arrhythmias associated with the manifestation of NPCA activity were found in 12 people among all examined adolescents (0.97%). In 1 young man, MVR was detected between the sinus node and the NPCA (Fig. 6). The teenager complained of cardialgia, sometimes a feeling of “lack of air.” To clarify the diagnosis, he was hospitalized at Children's City Clinical Hospital No. 5, where he was diagnosed with mild infectious-allergic myocarditis and chronic tonsillitis.
In 4 adolescents, constant NPR was registered, in 3 - episodes of NPR against the background of sinus or SPR, in 3 - single escape complexes from the lower parts of the right atrium. The incidence of ADR in the described cases was 59-98 beats/min. None of these adolescents had any health complaints and no organic heart damage was detected; none of them actively participated in sports. 5 of these teenagers were considered healthy; these teenagers did not smoke. The remaining 5 had concomitant diseases that could potentially affect the state of the cardiovascular system: chronic tonsillitis, obesity, borderline blood pressure, or combinations thereof; two of them also smoked. VSD was not detected in the group of adolescents under consideration.
Rice. 6. ECG of a young man V., 15 years old; recording speed 50 mm/s. MVR between the sinus node and the NPCA: change in the shape and polarity of the P wave in leads II, III, aVR, aVF; changing the duration of the RR interval from 0.58 to 0.84 s. Average heart rate – 80 beats/min.
As a percentage, the number of healthy and non-smoking adolescents with NPD and slipped lower atrial complexes was slightly lower than in the surveyed general population (50.0% and 71.9%, respectively), but the differences turned out to be statistically insignificant (χ2 – 3.84; p = 0.12 [11]).
In addition to the described cases, 1 18-year-old boy had episodes of NPR in combination with ventricular extrasystoles (Fig. 7). It can be assumed that the source of the rhythm in question with inverted P waves before the QRS complexes in this case is probably localized in the AV junction, and not in the lower parts of the right atrium. Indeed, restoration of sinus rhythm in this teenager was observed after a ventricular extrasystole, which can be explained by the fact that the ventricular extrasystole spreads to the AV junction. causes temporary inhibition of nodal centers of automatism and thereby contributes to the manifestation of activity of the sinus node. After some time, the activity of the AV centers is restored and the heterotopic rhythm is recorded again. During the initial examination, the young man had no complaints, no obvious organic pathology of the cardiovascular system was detected, but chronic tonsillitis was diagnosed. In addition, the teenager smoked, sometimes drank alcohol and, possibly, used psychoactive substances. He refused in-depth examination and further observation.
Rice. 7. ECG of a young man K., 18 years old; Lead II, recording speed 25 mm/s. NPR with heart rate 65-71 beats/min. (1, 2, 9-14, 16, 17 complexes). Ventricular extrasystoles (3rd and 18th complexes), after which episodes of sinus rhythm are recorded with a heart rate of 68-78 beats/min. (4-8, 19-22 complexes). The P wave in the 15th complex is confluent.
Arrhythmias associated with the manifestation of SPCA activity were detected much more often - in 26.4% of adolescents, including in 17.6% of adolescents MVR between the sinus node and SPCA or a combination of sinus and midatrial rhythms was recorded (it is difficult to distinguish between these conditions using an ECG), in 8.8% of cases, permanent SPR was found. The frequency of detection of chronic tonsillitis, VSD, obesity, borderline blood pressure and other concomitant diseases, as well as smoking in adolescents with arrhythmias associated with the manifestation of SPCA activity, and adolescents in whom sinus rhythm (or sinus arrhythmia) was recorded on the ECG did not differ significantly . In the examined population, organic diseases of the cardiovascular system were occasionally found - 4 adolescents had congenital heart defects (including 2 hemodynamically significant ones), 2 had current mild myocarditis, 2 had a history of myocarditis, confirmed by medical documentation, but without signs of myocardial cardiosclerosis at the time of examination, 1 had effective radical correction of congenital heart disease at the age of 6 years. Only 2 of these adolescents (22.2%) had arrhythmias associated with the manifestation of SPCA; in 1, the above-described MVR between the sinus node and SPCA was observed; in the rest, sinus rhythm was recorded.
After examination, 3 adolescents were diagnosed with paroxysmal supraventricular arrhythmias [8]. All of these adolescents showed sinus rhythm on the initial ECG.
Conclusion
Thus, when analyzing ECG in adolescents, it is advisable to distinguish arrhythmias associated with the manifestation of SPCA and arrhythmias associated with the manifestation of NPCA activity. These conditions are easily distinguishable from a conventional ECG and have varying prevalence and diagnostic significance. If arrhythmias associated with the manifestation of SPCA activity are a variant of the norm, then arrhythmias associated with the manifestation of SPCA can be classified as “borderline” conditions - they can be observed in healthy adolescents, occasionally in organic diseases of the cardiovascular system, sometimes in chronic tonsillitis and obesity, which does not exclude the possibility of the development of myocardial dystrophy in these adolescents, which contributes to the appearance of these arrhythmias. The feasibility of distinguishing two groups of heterotopic atrial arrhythmias is also associated with a unified approach to ECG analysis. Some investigators have reported a higher prevalence of MVR in adolescents [10], likely including both MVR between the sinus node and the AC and MVR between the sinus node and the AC. It should be noted that the frequency of detection of MVR and SPR is influenced by the duration of ECG recording in limb leads and the thoroughness of deciphering electrocardiographic films. However, we are well aware that the concept of SPCA remains speculative to a certain extent, because There is no clear histological evidence for the presence of such centers, although other areas of initiation of atrial depolarization have been documented outside the sinus and AV nodes in the atria [17]. At the same time, researchers who have studied the structure of the conduction system of the heart are mainly based on the criteria of Aschoff and Menckeberg (L. Aschoff, 1910; JG Monckeberg, 1910), which make it possible to histologically distinguish between contractile fibers and cells of the conduction system. It should be noted that only His bundle cells and Purkinje fibers satisfy all Aschoff and Mönckeberg criteria. No structure within the atria meets all of these criteria, including Bachmann's bundle, sinus node, and AV node (which are non-insulated tissues). The need to clarify these postulates is quite obvious for some histologists. It is likely that new criteria will be proposed based on histomolecular methods that will better define the uniqueness of the specialized structures of the cardiac conduction system [17].
In most English-language manuals, the ECG picture of MVR between the sinus node and SPCA is considered as sinus arrhythmia, which is an unconditional variant of the norm in adolescents. True, as noted above, the reasons for the significant variation of the P wave (but without the appearance of negative P in lead II) are not explained. In the Minnesota code, intended for decoding ECG in adults in epidemiological studies [13], the criteria for MVR are not specified, and supraventricular rhythm includes all cases when the P wave is absent or there is a pathological P wave - negative or flat in leads II, III and aVF , that is, in fact, nodal and all ectopic atrial rhythms are included in a single concept. In addition, such a rhythm, as indicated in the Minnesota code, is characterized by a shortening of the PQ interval of less than 0.12 s, although in clinical electrocardiography when assessing atrial rhythms there is no strict requirement for the PQ duration [13].
In the cardiological literature, the term “MVD within the sinus node” is sometimes used [5]. However, in our opinion, this term will be identical to the term “sinus arisupraventricular rhythm (complexes) with preceding negative P waves in lead II” and “migration of the atrial pacemaker with the appearance of negative P waves in lead II.” Such rhythm changes are rarely detected during population surveys; they can occur in healthy adolescents, but always require additional examination to exclude organic diseases of the cardiovascular system or concomitant diseases that contribute to the occurrence of such arrhythmias. At the same time, the use of the concepts “SPCA” and “NPCA” (and corresponding arrhythmias) when deciphering an ECG seems quite logical to us.
Escaping complexes and rhythms from the AV junction are an extremely rare situation observed in population-based examinations of adolescents. Such arrhythmias always require clinical interpretation and dynamic monitoring of the adolescent.
What is the danger
Active generation of heart rhythm from an atypical focus is most often a symptom of pathology of the myocardium or other organs and systems. I recommend that you undergo additional examinations and identify the cause of ectopia.
Rhythm and hemodynamic disturbances, especially with a high frequency of contractions and concomitant diseases, can lead to the formation of blood clots, angina attacks, the development of a heart attack, flicker, flutter and the gradual formation of heart failure.
Why does ectopic rhythm appear?
Ectopic rhythm occurs due to a weakening of the rhythmic functioning of the sinus node, or a complete cessation of its activity.
In turn, complete or partial inhibition of the sinus node is the result of various diseases and conditions:
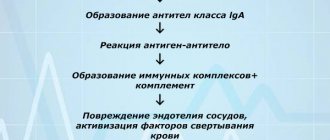
- Inflammation. Inflammatory processes in the heart muscle can affect both the cells of the sinus node and the muscle fibers in the atria and ventricles. As a result, the ability of cells to produce impulses and transmit them to underlying sections is impaired. At the same time, the atrial tissue begins to intensively generate excitation, which is supplied to the atrioventricular node at a frequency higher or lower than usual. Such processes are caused mainly by viral myocarditis.
- Ischemia. Acute and chronic myocardial ischemia also contributes to impaired activity of the sinus node, since cells deprived of sufficient oxygen cannot function normally. Therefore, myocardial ischemia occupies one of the leading places in the statistics of the occurrence of rhythm disturbances, including ectopic rhythms.
- Cardiosclerosis. The replacement of normal myocardium with growing scar tissue due to previous myocarditis and infarctions interferes with the normal transmission of impulses. In this case, in persons with ischemia and post-infarction cardiosclerosis (PICS), for example, the risk of ectopic heart rhythm increases significantly.
In addition to pathology of the cardiovascular system, vegetative-vascular dystonia, as well as hormonal imbalances in the body - diabetes mellitus, pathology of the adrenal glands, thyroid gland, etc., can lead to ectopic rhythm.
Possible symptoms
Ectopic left and right atrial rhythms manifest themselves in the same way. A person often does not notice changes, and the symptoms of the underlying disease that caused the deviation come first. The only way to detect a violation is to take an electrocardiogram.
In other cases, the patient makes the following complaints:
- feeling of pulse unevenness and interruptions;
- heart sinking;
- dyspnea;
- weakness, decreased ability to work;
- pain or discomfort in the heart area.
In the presence of temporary jumping atrial complexes, symptoms usually either do not appear or are transient. According to my observations, they do not pose any particular danger and do not affect hemodynamics.
With prolonged attacks, the patient’s condition worsens, in addition to the main complaints, signs of circulatory disorders and cardialgia of ischemic origin appear.
Sometimes ectopic rhythm occurs due to dysfunction of the autonomic system:
- If the influence of the sympathetic department predominates, a person’s pulse quickens, the skin becomes cool and pale, and hypertension is observed. This condition is characterized by chills, headache, and often a panic attack.
- When vagotonia (parasympathetic) comes first, the frequency of contractions decreases, sweat is released, blood pressure decreases, and digestion is disrupted.
Symptoms of ectopic rhythm
The clinical picture of replacement heart rhythms can be clearly expressed or not manifested at all. Usually, the symptoms of the underlying disease come first in the clinical picture, for example, shortness of breath on exertion, attacks of burning pain in the chest, swelling of the lower extremities, etc. Depending on the nature of the ectopic rhythm, the symptoms may be different:
- With ectopic atrial rhythm , when the source of impulse generation is located entirely in one of the atria, in most cases there are no symptoms, and disturbances are detected by the cardiogram.
- With a rhythm from the AV junction, a heart rate close to normal is observed - 60-80 beats per minute, or below normal. In the first case, no symptoms are observed, but in the second, attacks of dizziness, a feeling of lightheadedness and muscle weakness are noted.
- With extrasystole, the patient notes a feeling of fading, cardiac arrest, followed by a sharp jolt in the chest and a further absence of sensations in the chest. The more often or less often the extrasystoles, the more varied the symptoms in duration and intensity.
- With atrial bradycardia , as a rule, the heart rate is not much lower than normal, within 50-55 per minute, as a result of which the patient may not notice any complaints. Sometimes he is bothered by attacks of weakness and sudden fatigue, which is caused by a reduced flow of blood to the skeletal muscles and brain cells.
- Paroxysmal tachycardia manifests itself much more clearly. During paroxysm, the patient notes a sharp and sudden sensation of accelerated heartbeat. According to many patients, the heart flutters in the chest like a “hare’s tail.” The heart rate can reach 150 beats per minute. The pulse is rhythmic, and may remain around 100 per minute, due to the fact that not all heartbeats reach the peripheral arteries at the wrist. In addition, there is a feeling of lack of air and chest pain caused by insufficient oxygen supply to the heart muscle.
- Atrial fibrillation and flutter can be paroxysmal or permanent. The basis of atrial fibrillation is a chaotic, non-rhythmic contraction of different parts of the atrium tissue, and the heart rate in the paroxysmal form is more than 150 per minute. However, there are normo- and bradysystolic variants, in which the heart rate is within the normal range or less than 55 per minute. The symptoms of the paroxysmal form resemble an attack of tachycardia, only with an irregular pulse, as well as a feeling of irregular heartbeat and interruptions in heart function. The bradysystolic form may be accompanied by dizziness and lightheadedness. With a permanent form of arrhythmia, the symptoms of the underlying disease that led to it come to the fore.
- Idioventricular rhythm is almost always a sign of serious cardiac pathology, such as severe acute myocardial infarction. In most cases, symptoms are noted, since the myocardium in the ventricles is capable of generating electricity at a frequency of no more than 30-40 per minute. In this regard, the patient may experience Morgagni-Edams-Stokes (MES) episodes - attacks of loss of consciousness lasting several seconds, but no more than one or two minutes, since during this time the heart “turns on” compensatory mechanisms and begins to contract again. In such cases, they say that the patient is “massing.” Such conditions are very dangerous due to the possibility of complete cardiac arrest. Patients with idioventricular rhythm are at risk of developing sudden cardiac death.
How to make a diagnosis
At the moment, the only objective way to detect ectopic atrial rhythm is an ECG. In the case when the impulses are temporary and interspersed with full myocardial contractions, Holter monitoring is used for diagnosis.
An electrocardiogram will reveal not only rhythm disturbances, but also indicate the localization of pathological impulses based on the state of the P wave. For clarity, you can give a table that shows how different types of ectopia manifest themselves:
| Localization in the atria | Leads | Signs (P wave) |
| Left | Right pectorals (V1-2) | two-phase, the first part is domed, the second is pointed, positive |
| Left pectorals (V5-6) | negative | |
| Standard (I, II) | smoothed out | |
| Right (photo 2) | I, II | positive |
| II, III | negative | |
| V1-6 and aVF | smoothed out | |
| Inferior atrial rhythm (Fig. 1) | I, III, aVF | negative |
Atrial rhythm in its pure form is not accompanied by a change in the electrical axis of the heart (EOS), and it is also not characterized by the appearance of deformation of the ventricular complexes.
As additional research methods and to identify the cause, I usually recommend:
- General and biochemical analysis of blood and urine. Laboratory results show the presence of inflammatory processes, problems in kidney function, and electrolyte imbalance.
- EchoCG. Ultrasound examination of the myocardium will help detect dilation of the heart, valvular insufficiency, and the presence of structural changes.
- In case of chest injury, an x-ray is taken.
Ectopic rhythms in children
In children, this type of arrhythmia can be congenital or acquired.
Thus, ectopic atrial rhythm occurs most often with vegetative-vascular dystonia, with hormonal changes during puberty (in adolescents), as well as with pathology of the thyroid gland.
In newborns and young children, a right atrial, left or lower atrial rhythm may be a consequence of prematurity, hypoxia or pathology during childbirth. In addition, the neurohumoral regulation of heart activity in very young children is immature, and as the baby grows, all heart rate indicators can return to normal.
If the child does not have any pathology of the heart or central nervous system, then the atrial rhythm should be considered a transient, functional disorder, but the baby should be regularly monitored by a cardiologist.
But the presence of more serious ectopic rhythms - paroxysmal tachycardia, atrial fibrillation, atrioventricular and ventricular rhythms - require more detailed diagnosis, as this may be due to congenital cardiomyopathy, congenital and acquired heart defects, rheumatic fever, viral myocarditis.
Treatment
If a problem occurs in a healthy person under the influence of external factors, then it is transient and is eliminated when their influence ceases. In this case, no treatment is required. In the presence of a pathological condition, the main therapy should be aimed at eliminating the cause. To directly stop ectopic rhythm from the atria, the following are used:
- beta blockers for frequent contractions (Anaprilin);
- stimulants for bradycardia (Atropine);
- if there is a lack of potassium and magnesium, Panangin is used;
- sedatives for autonomic disorder (Motherwort, Persen);
- soothing herbal infusions.
In case of severe disorders with a pronounced decrease in the frequency of contractions and a high probability of developing a heart attack and other acute conditions, the issue of installing an artificial pacemaker is decided.
Lifestyle restrictions
To prevent rhythm disturbances and the occurrence of ectopic atrial complexes, heart disease should be treated in time and the functioning of the autonomic nervous system should be restored. Following the usual rules will help improve the condition of existing deviations and prevent their development:
- Nutrition plays an important role. It must be balanced and complete. It is necessary to drink 1.5–2 liters of liquid per day, exclude animal fat from the menu, and consume as many vegetables and fruits as possible. You should eat small portions 4-5 times a day.
- Eliminate the possibility of overwork and normalize sleep.
- Breathe fresh air, go hiking, walk in a public garden or park.
- Exercise daily and go to the gym. Swimming, dancing, yoga will be beneficial.
- Studying with a psychologist and meditative practices help to develop stress resistance.
- Do not abuse alcohol, quit smoking.