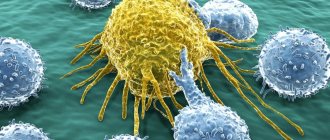
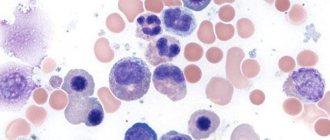
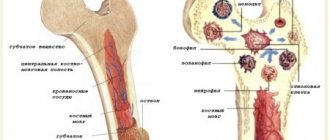
Lymphocyte / National Human Genome Research Institute is a type of white blood cell (leukocyte). Like all white blood cells, lymphocytes are produced in the bone marrow and are an essential element of the immune system T and B Lymphocyte and Natural Killer Cell Profile / University of Rochester Medical Center.
Some lymph cells are able to remember pathogens that the body has encountered before, and thus form cellular immunity. The second type of lymphocytes produces antibodies to infections already familiar to the body and is an important element of immunity. The third type is engaged in the destruction of diseased cells of one’s own body—those affected by a virus, cancer, or other damage.
Causes of lymphocytopenia
Physiological processes
Lymphocytopenia is not necessarily a sign of any disease. The cause may be various physiological conditions, for example, prolonged stress. When stressed, adrenal hormones (glucocorticosteroids) are released into the blood, which have a destructive effect on lymphocytes. Lymphocytopenia can also occur with protein deficiency, so it often occurs during fasting or in people following a vegetarian or vegan diet.
Viral infections
Under the influence of some lymphotropic viruses, accelerated death of lymphocytes occurs. The most common and dangerous infectious cause of lymphocytopenia is the human immunodeficiency virus (HIV). It binds to special receptors (CD4) on the surface of T-lymphocytes (T-helpers), penetrates into the cell, where it actively multiplies and leads to its death. A decrease in the number of T helper cells occurs both due to the direct damaging effect of the virus and due to the activation of apoptosis (programmed cell death) and autoimmune damage.
At the very beginning of infection, the level of lymphocytes can, on the contrary, increase with the development of leukocytosis as an immune reaction to a foreign microorganism, but then there follows a rapid drop in the concentration of white blood cells until their complete absence, which is associated with the development of acquired immunodeficiency syndrome, the increased susceptibility of the patient’s body to various infections, including opportunistic ones. Lymphocytopenia may begin to regress only after long-term antiretroviral therapy.
In addition, the following viral infections contribute to the destruction of lymphocytes, in which lymphocytopenia is much less pronounced than with HIV:
- Measles.
It is a common cause of lymphocytopenia in children. The measles virus causes the death of follicular B lymphocytes. Even after recovery, immunosuppression may persist for several weeks or months. The measles virus also damages immunological memory cells, causing temporary “immune amnesia.” - Respiratory syncytial infection.
It is considered the leading cause of lower respiratory tract disease in infants and young children. - Flu.
The development of lymphocytopenia often occurs in adults with severe influenza A1, swine and bird flu. Its occurrence is a predictor of serious complications and poor prognosis. - SARS (acute respiratory syndrome, atypical pneumonia).
The causative agent is coronavirus. It is assumed that the cause of lymphocytopenia is the induction of cytokine release syndrome (cytokine storm) by the virus, leading to the death of immune cells.
Bacterial infections
Lymphocytopenia can also be caused by some bacterial infections - leptospirosis, ehrlichiosis, legionellosis. Lymphopenia is of greatest importance in such common infections as tuberculosis (miliary, disseminated). With this disease, there is a decrease in T-helper cells and T-suppressor cells (CD4, CD8 cells). Pathology occurs in septic conditions (bacterial blood infection). Absolute lymphocytopenia indicates an unfavorable course of any bacterial infection. The indicators quickly return to normal after antibacterial and anti-tuberculosis therapy.
Autoimmune diseases
Another cause of lymphocytopenia is chronic inflammatory diseases of an autoimmune nature. Numerous studies have revealed two main pathogenetic mechanisms of lymphopenia in these pathologies: the release of antilymphocyte antibodies and a decrease in the expression of special proteins (CD55, CD59) on the membranes of immune cells that protect cells from complement-mediated cytolysis. Lymphocytopenia is usually moderate, may correlate with the severity of the disease, and regresses during remission or under the influence of pathogenetic treatment.
- Joint diseases.
Rheumatoid arthritis. - Diffuse connective tissue diseases (collagenoses).
Systemic lupus erythematosus, Sjögren's syndrome. - Systemic vasculitis.
Granulomatosis with polyangiitis, Takayasu nonspecific aortoarteritis. - Inflammatory bowel diseases (IBD).
Nonspecific ulcerative colitis, Crohn's disease. - Multiple sclerosis.
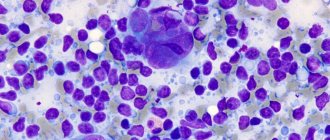
Lymphoproliferative diseases
Oncohematological pathologies, such as lymphogranulomatosis (Hodgkin's lymphoma), T-B cell lymphomas, lymphosarcoma, can also cause lymphocytopenia. It usually develops in the later stages of the disease and is considered one of the criteria for an unfavorable outcome. The drop in the level of lymphocytes is due to the depletion of lymphoid tissue and the replacement of hematopoietic tissue with atypical malignant cells.
Rare causes
- Inhibition of lymphocyte formation
: hereditary immunodeficiencies (Wiskott-Aldrich syndrome, DiGeorge syndrome), diseases accompanied by the replacement of lymphoid tissue with epithelioid granulomas (sarcoidosis, histiocytosis X), exposure to ionizing radiation, aplastic anemia. - Lymph loss:
damage to large lymphatic ducts during trauma and abdominal surgery, massive burns, primary intestinal lymphangiectasia (Waldmann's disease). - Accelerated destruction of lymphocytes
: endocrine disorders (Cushing's disease and syndrome, type 1 diabetes), end-stage chronic renal failure. - Use of medications:
glucocorticosteroids, immunosuppressants (methotrexate, azathioprine), monoclonal antibodies. - Diseases with an unknown mechanism of lymphocytopenia:
malignant neoplasms - breast, thyroid, rectal cancer.
Why is lymphopenia dangerous?
This is not a disease in itself, but simply a deficiency of a certain type of blood cell. Some people have low lymphocytes from birth. In this case, lymphopenia is considered a variant of the norm: the immune system works perfectly on the available “reserves”.
But more often it happens differently. A decrease in the level of lymphocytes leads to the fact that a person’s immunity sharply decreases. The body begins to produce antibodies worse, loses memory of previous infections and cannot stop the spread of diseased cells in time.
All this leads to the fact that a person begins to get sick often. And any infections, even harmless ones like ARVI, quickly develop complications and turn into bronchitis, pneumonia or dangerous inflammatory processes in other organs.
Diagnostics
The level of lymphocytes is measured by calculating the leukocyte formula in a clinical blood test. Since the range of diseases that can cause lymphopenia is quite wide, if it is detected, you should consult a doctor for a detailed examination. Based on clinical and anamnestic data, the specialist draws up a program of diagnostic studies, which includes:
- Lab tests.
Both the total number and percentage of different types of leukocytes are studied. The level of inflammatory markers - ESR, CRP - is determined. The presence of autoantibodies (ACCP, antibodies to DNA, to the cytoplasm of neutrophils) is checked. If sepsis is suspected, procalcitonin and presepsin are measured. In inflammatory bowel pathologies, the content of fecal calprotectin in the stool increases. The concentration of serum immunoglobulins (IgG, IgM, IgA) is examined. - Microbiological research.
To confirm tuberculosis, bacteriological culture and microscopy of sputum, tuberculin diagnostics (Mantoux test, Diaskin test) are performed. The enzyme immunoassay method identifies antibodies to pathogens (viruses, bacteria). A verification test for HIV infection is the detection of viral envelope proteins (gp120, gp41) by immunoblotting. - Instrumental research.
With tuberculosis, radiographs of the lungs show an increase in lymph nodes (hilar, mediastinal), and infiltration of the upper lobes of the lungs. Images of joints in rheumatoid arthritis reveal narrowing of the joint space, marginal erosions, and osteoporosis. During fibrocolonoscopy in patients with IBD, hyperemia of the mucous membrane and areas of ulceration are found. MRI of the brain in multiple sclerosis shows oval-shaped foci of demyelination measuring 1-2 mm. - Histological studies.
When examining material obtained by biopsy of a lymph node, diffuse proliferation of lymphoid cells with blast morphology, Berezovsky-Sternberg cells, is noted in patients with lymphoproliferative diseases. In case of systemic vasculitis, perivascular infiltration with plasma cells and histiocytes is detected in the biopsy specimen.
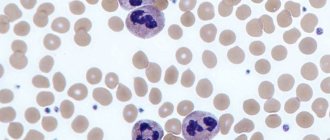
Complete blood count - a method for detecting lymphopenia
Normal lymphocyte count for women
In adult patients, the component indicators have a conditionally stable value. Measurements of the number of lymphocytes are carried out according to two parameters:
- by absolute value - indicates the number of cells in the blood;
- relative - the percentage of lymphocytes in the total number of leukocytes is calculated.
The norm for the female body is considered to be 1-1.45 billion cells per liter of blood, which is equal to almost 40% of the leukocytes contained. Differences from the specified value may indicate hidden pathologies.
Correction
There are no ways to independently relieve lymphocytopenia. To normalize the level of lymphocytes, it is necessary to eliminate the cause, namely, treat the underlying pathology. If lymphocytopenia occurs due to stress or protein deficiency in the diet, treatment is not required, it is enough to adjust the diet. For persistent, long-term lymphopenia, medical intervention is necessary. Depending on the reason, the following measures are applied:
- Fighting infection.
To treat HIV infection, antiretroviral therapy is prescribed - nucleoside reverse transcriptase inhibitors, protease inhibitors (saquinavir). Oseltamivir is indicated for influenza. For the treatment of other viral infections, there are no etiotropic medications; symptomatic methods are used (antipyretics, detoxification therapy). For nonspecific bacterial infections, antibiotics are recommended; for tuberculosis, combinations of antituberculosis drugs (isoniazid, rifampicin). - Anti-inflammatory therapy.
To achieve remission of autoimmune diseases, medications are used that suppress the inflammation process - glucocorticosteroids, synthetic derivatives of aminoquinoline and 5-aminosalicylic acid, immunosuppressants (methotrexate, cyclophosphamide). - Treatment of lymphoproliferative diseases.
For lymphogranulomatosis and non-Hodgkin's lymphomas, polychemotherapy (vincristine, dacarbazine, etoposide) is indicated. Irradiation of tumor-affected lymph nodes is effective.
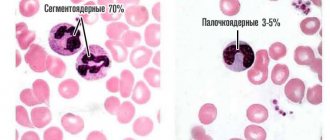
Interpretation of analyzes
When deciphering a blood test, all indicators are assessed together. When diagnosing, special attention is paid to the leukocyte formula, which reflects the ratio of all types of white blood cells. In diseases, the content of some leukocytes may change due to an increase or decrease in others. Using the leukocyte formula, one can judge the development of complications, how the pathological process proceeds, and also predict the outcome of the disease.
According to leukogram data, it is possible to distinguish a viral disease from an infectious one. With a viral infection, the total number of all leukocytes does not change or is slightly increased, but there are changes in the leukocyte formula: lymphocytes are increased, neutrophils are decreased. At the same time, ESR (erythrocyte sedimentation rate) increases slightly, with the exception of acute pronounced processes of viral origin. As for bacterial damage, the level of leukocytes increases due to the growth of granulocytes, the relative content of lymphocytes decreases. ESR during bacterial infections reaches very high values.
Forecast
Lymphocytopenia is quite often a predictor of an unfavorable prognosis and is associated with an increased risk of infectious diseases and activation of opportunistic microflora. The outcome and life expectancy of patients are determined by the underlying pathology against which the lymphopenia occurred. The most benign is lymphocytopenia, which develops after prolonged stress or protein starvation. Hereditary immunodeficiency conditions and oncohematological diseases are characterized by a high probability of death in the early stages.
Why might neutrophils be low?
Low blood levels are characteristic of some diseases and conditions:
- infections of viral origin (chickenpox, hepatitis, influenza);
- inflammatory processes;
- radiation sickness;
- taking certain medications (usually cytostatics or immunosuppressants in the treatment of autoimmune diseases or malignant tumors, as well as antimicrobials - penicillin, cephalosporin, sulfonamide);
- chemotherapy for cancer;
- agranulocytosis;
- anemia (aplastic and hypoplastic);
- exposure to radiation.
The norm of lymphocytes in the blood in adults and children
Unfortunately, there are often situations when lymphocytes in the blood can deviate from the norm - increase or decrease. This can happen in various situations. Before we talk about when the number of lymphocytes changes in the blood, we need to talk about how much is their normal component.
If we talk about cell clones, then:
T cells make up 75% of the total number of lymphocytes;
B cells about 15%;
Natural killers are about 10%.
And speaking about the norms of lymphocytes, it must be said that at different periods of a person’s life the norms differ.
Lymphocytes begin to be produced by the bone marrow already in utero, and this process continues throughout life. The lifespan of these cells also varies - from several months to sixty years. And these will all be lymphocytes.
- Up to 1 year, the content of lymphocytes in the blood of the total number of all cells is 45-70%.
- From 1-2 years, the concentration of lymphocytes should decrease - somewhere around 39-60%.
- From 2-4 then somewhere from 33-50% of all white cells.
- From 4-10 years, already 30-50%.
- From 10-18 years old, then this is already 30-44%.
- In an adult, lymphocytes in the blood should range from 19-37%.
The table shows the values of acceptable norms of lymphocytes (individual subpopulations) in the blood of children and adults.
| Age | Proportion of the total number of lymphocytes, % | Absolute cell count, *106/l |
| CD 3+ (T lymphocytes) | ||
| Up to 3 months | 50 – 75 | 2065 – 6530 |
| Up to 1 year | 40 – 80 | 2275 – 6455 |
| 1 – 2 years | 52 – 83 | 1455 – 5435 |
| 25 years | 61 – 82 | 1600 – 4220 |
| 5 – 15 years | 64 – 77 | 1410 – 2020 |
| Over 15 years old | 63 – 88 | 875 – 2410 |
| CD3+CD4+ (T helper cells) | ||
| Up to 3 months | 38 – 61 | 1450 – 5110 |
| Up to 1 year | 35 – 60 | 1695 – 4620 |
| 1 – 2 years | 30 – 57 | 1010 – 3630 |
| 25 years | 33 – 53 | 910- 2850 |
| 5 – 15 years | 34 – 40 | 720 – 1110 |
| Over 15 years old | 30 – 62 | 540 – 1450 |
| CD3+CD8+ (T-cytotoxic lymphocytes) | ||
| Up to 3 months | 17 – 36 | 660 – 2460 |
| Up to 1 year | 16 – 31 | 710 – 2400 |
| 1 – 2 years | 16 – 39 | 555 – 2240 |
| 25 years | 23 – 37 | 620 – 1900 |
| 5 – 15 years | 26 – 34 | 610 – 930 |
| Over 15 years old | 14 – 38 | 230 – 1230 |
| CD19+ (B lymphocytes) | ||
| Up to 2 years | 17 – 29 | 490 — 1510 |
| 25 years | 20 – 30 | 720 – 1310 |
| 5 – 15 years | 10 – 23 | 290 – 455 |
| Over 15 years old | 5 – 17 | 100 – 475 |
| CD3-CD16+CD56+ (NK cells) | ||
| Up to 1 year | 2 – 15 | 40 – 910 |
| 1 – 2 years | 4 – 18 | 40 – 915 |
| 25 years | 4 – 23 | 95 – 1325 |
| 5 – 15 years | 4 – 25 | 95 – 1330 |
| Over 15 years old | 4 – 27 | 75 – 450 |
| Over 15 years old | 1 – 15 | 20-910 |