Heart failure (HF) is a complex clinical syndrome resulting from any structural or functional abnormality of the heart that leads to a weakening of the ability of the ventricles to fill and release blood. [1]
Evolutionary origins of HF
. Researchers have noted the importance of blood pressure in the evolution of land animals.[2] High blood pressure is of fundamental importance because it ensures: perfusion of tissues of a large organism outside the aquatic environment; increased body speed; the function of excreting waste and high-level by-products arising from a large, fast-moving body. The body's response to a decrease in blood pressure due to bleeding is similar to those that occur due to heart failure.
Causes of AHF
The loss of the heart's ability to contract can be caused by overload of the heart muscle, for example, due to increased blood pressure, a decrease in the number of functioning muscle fibers, heart rhythm disturbances, or the inability to adapt to physical and emotional stress.
The leading causes of AHF are cardiac, associated with pathologies of the heart itself:
- Acute coronary syndrome (ACS) is a condition caused by a sudden disruption of the blood supply to the heart. It develops with thrombosis of the arteries that supply blood to the heart muscle, narrowing of the heart vessels caused by the presence of atherosclerotic plaques or spasm. It manifests itself as myocardial infarction - irreversible necrosis of the heart muscle and a pre-infarction state, which is not accompanied by a complete cessation of blood supply to the myocardium, but can result in a heart attack. The leading symptoms of ACS are severe chest pain and specific changes in the electrocardiogram (ECG).
- Hypertensive crisis. It is caused by a persistent increase in blood pressure (BP) and is accompanied by certain symptoms: headache, nausea and vomiting, shortness of breath, visual disturbances, sometimes convulsions, chest pain due to insufficient blood supply to the myocardium.
- Sudden arrhythmias and heart blocks. The following are considered life-threatening: complete inability to conduct a cardiac impulse to the ventricles of the heart from the atria, when each of them contracts in its own rhythm (AV block), a decrease in the heart rate (HR) to 40 beats/min and below, paroxysmal tachycardia, cardiac arrest . “Precursors” of dangerous arrhythmias are heart rate less than 50 and more than 110 beats/min, frequent extraordinary heart contractions, atrial fibrillation.
- Severe heart valve defects. They appear against the background of rheumatism and other connective tissue pathologies, atherosclerosis, coronary artery disease (IHD) and severe infections. Various defects lead to overload of the heart with pressure or volume, which creates an obstacle to the release of blood into the circulatory system. With myocardial infarction, ruptures of the tendon structures of the mitral and tricuspid valves are possible with the formation of valvular insufficiency.
- Acute myocarditis. These are severe inflammatory lesions of the heart muscle caused by viruses or bacteria.
- Cardiac tamponade. This is the accumulation of blood or other fluid between the layers of the outer lining of the heart, which prevents adequate heart contractions and filling the heart with blood. Tamponade occurs with wounds and trauma to the heart, dissection and rupture of an aortic aneurysm (protrusion), myocardial infarction with rupture of the heart wall (transmural infarction), pericarditis due to infections and cancer. The accumulation of 500 ml of fluid in the pericardial cavity leads to cardiac arrest.
- Chronic heart failure (CHF) in the stage of decompensation.
Extracardiac causes of AHF are:
- Thromboembolism of the pulmonary artery (PE) and its branches. The source of pulmonary embolism is thrombosis of the veins of the lower extremities with thrombophlebitis, in the postoperative period, with prolonged immobility of the body and limbs due to injuries (most often).
- Acute circulatory disorders of the brain, in which the release of vasoactive hormones occurs (they maintain high pressure in the vessels of the lungs).
- Pneumothorax is the accumulation of air in the chest cavity due to lung diseases and due to chest injuries. With tension pneumothorax, with each inhalation and exhalation, the volume of air in the chest increases, the lung on the affected side collapses, and the heart moves to the opposite side. In this case, the venous return to the heart and the contractile function of the myocardium are disrupted.
Risk factors
Factors that increase the risk of developing acute heart failure include:
- failure to comply with recommendations for the treatment of CHF;
- physical stress and emotional stress;
- severe acute infections and pneumonia;
- an increase in BCC (circulating blood volume) with excessive intravenous drips of drugs (for kidney disease, in patients with CHF);
- renal failure;
- alcohol abuse;
- overdose of drugs with cardiotoxic effect;
- bronchial asthma.
Models of the disease[edit]
Hemodynamic model of the development of heart failure[edit]
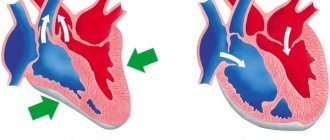
The body responds to initial cardiac injury, for example due to decreased blood pressure and decreased renal perfusion, by making hemodynamic changes to ensure tissue perfusion. Edema (salt and water retention) help ensure output volume according to the Frank-Starling law (systolic blood volume increases due to an increase in the volume of blood filling the heart, end-diastolic volume), through end-diastolic pressure; and vasoconstriction (narrowing of blood vessels) maintains blood pressure but at the cost of afterload on the ventricular muscle. An increase in end-diastolic pressure and afterload of the ventricular muscle aggravates cardiac dysfunction.
Treatments based on the hemodynamic model of heart failure have not been proven to be highly effective: inotropic (changing the force of muscle contraction) drugs have been shown almost without exception to be ineffective and sudden changes in hemodynamics (both with the help of vasodilators and even with heart transplantation) do not lead to immediate improving heart functions.
Neurohormonal model[8][edit]
This model is being used in new treatments for HF. The operating principle according to this model is the sympathetic nervous system and the renin-angiotensin system. The hormonal factor has a more widespread effect than just hemodynamic changes, causing direct harm to the heart causing programmed cell death and fibrosis. Based on the neuro-hormonal model, modern treatment methods with ACE inhibitors, beta-blockers, and aldosterone receptor antagonists are being developed.
Peripheral model[edit]
The model emphasizes the consequences of HF in the periphery, especially in skeletal muscle. To a certain extent, skeletal muscle myopathy develops due to poor perfusion, as a consequence of poor health, and also due to neurohormonal and cytokine activation. Myopathy is the main cause of symptoms such as fatigue and shortness of breath, but also leads to activation of the sympathetic nervous system, which leads to further damage to the heart. Treatments aimed at preserving skeletal muscle function or even reversing myopathy may help treat HF.
- ACC and AHA Task Force on Practice Guidelines. 2009 Focused Update Incorporated into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults. Circulation 2009; 119:e391–e479
- Harris P. Evolution and the cardiac patient. Cardiovascular Research 1983; 17
- Fonarow GC, Abraham WT, Albert NM, et al. ; OPTIMIZE-HF Investigators and Hospitals. Factors identified as precipitating hospital admissions for heart failure and clinical outcomes: fi ndings from OPTIMIZE-HF. Archives of Internal Medicine 2008; 168.
- Killip T 3rd, Kimball JT. Treatment of myocardial infarction in a coronary care unit. A two year experience with 250 patients. American Journal of Cardiology 1967; 20
- Cowie MR, Wood DA, Coats AJ, et al. Survival of patients with a new diagnosis of heart failure: a population based study. Heart 2000; 83
- Stewart S, MacIntyre K, Hole DJ, Capewell S, McMurray JJ. More 'malignant' than cancer? Five-year survival following a first admission for heart failure. European Journal of Heart Failure 2001; 3
- Anguita M, Arizón JM, Bueno G, Concha M, Vallés F. Spontaneous clinical and hemodynamic improvement in patients on waiting list for heart transplantation. Chest 1992; 102
- Packer M. The neurohormonal hypothesis: a theory to explain the mechanism of disease progression in heart failure. J Am Coll Cardiol 1992; 20
Forms of the disease
The following forms of left ventricular AHF are distinguished:
- Acute decompensated heart failure is an extreme degree of heart failure that appears for the first time.
- Hypertensive AHF. It is characterized by high blood pressure and venous congestion in the lungs, which is visible on x-ray.
- Pulmonary edema is a high degree of blood stagnation in the capillaries of the lungs with the release of the liquid part of the blood with red blood cells into the lumen of the alveoli, the formation of foamy sputum and impaired gas exchange. Blood oxygen saturation in pulmonary edema before treatment is less than 90% (normally 96–99%).
- Cardiogenic shock is a sudden decrease in cardiac output and systolic pressure to 90 mmHg. Art. and below, which lead to a significant decrease in blood supply to organs and tissues. The main causes of cardiogenic shock are severe rhythm disturbances and myocardial infarction.
- AHF with high cardiac output. A rare form of deficiency. Accompanies those pathologies in which the heart rate increases: severe anemia, thyrotoxicosis, arrhythmias, sepsis.
The main forms of acute left ventricular failure are listed above. The first three are the most common. These include up to 90% of all cases of hospitalization with AHF. Acute right ventricular failure is less common. It develops mainly in severe lung diseases, right ventricular myocardial infarction and pulmonary embolism.
Heart rhythm disturbances
A wide variety of cardiac arrhythmias occur in ACS and MI. 70% of patients with myocardial infarction die in the first 6 hours! Ventricular fibrillation, ventricular tachycardia, is the most common cause of death. After 12 hours, ventricular fibrillation rarely develops. In case of ventricular fibrillation, defibrillation is carried out with an initial discharge power of 150-200 J for a biphasic defibrillator, and 360 J for a monophasic one. And, if necessary, extensive CPR is carried out according to accepted rules.
To prevent recurrence of fibrillation, amiodarone 150-300 mg is administered intravenously over 20-30 minutes. The daily dose of the drug is 800-1200 mg orally or intravenously. Usually used in combination with beta-blockers. Frequent (more than 5 per 1 minute) polytopic extrasystoles, especially early ones, can lead to ventricular fibrillation. In such cases, amiodarone can be used according to the above scheme.
Why is heart failure dangerous? Complications
AHF is a life-threatening condition. The risks of death are especially high with cardiogenic shock (about 80%). If the patient survives after the development of acute heart failure, his quality of life may deteriorate: poor exercise tolerance occurs, any excessive emotions can provoke a heart attack, and severe arrhythmias are possible. To prevent repeated decompensation of cardiac activity, the need for medications usually increases, which increases the drug load on the body. In some cases, serious surgical interventions are required, which are also accompanied by life-threatening risks.
Symptoms of AHF
The symptoms of acute left ventricular and right ventricular failure are different.
Symptoms of left ventricular AHF
Acute left ventricular failure almost never occurs in healthy people. It is preceded by undetected or inadequately treated hypertension, heart defects, ischemic heart disease with cardiosclerosis, arrhythmias, and myocardial infarction.
Provoking factors may be physical activity, stress, intravenous infusion of an excess volume of dissolved drugs. In some cases, symptoms develop at night due to increased pulmonary congestion or heart rhythm disturbances.
The main manifestations of left ventricular AHF are cardiac asthma, pulmonary edema and cardiogenic shock. These conditions are a consequence of severe stagnation of venous blood in the lungs. They can develop sequentially, accompanied by the following symptoms:
- severe shortness of breath, which can cause suffocation;
- fear of death, dizziness, weakness;
- persistent chest pain;
- forced sitting position with support on hands to facilitate breathing - orthopnea;
- cough is dry, then wet, with foamy pink sputum;
- the skin is pale, covered with cold sweat, there may be a bluish discoloration of the lips, ears, nose;
- pulse is frequent (more than 90 beats/min), weak filling, often arrhythmic;
- Blood pressure may be elevated or normal and decreases as symptoms progress.
Symptoms of right ventricular AHF
With this pathology, “acute cor pulmonale” (ACP) develops. Causes of ULS:
- acute severe diseases of the bronchopulmonary system - a prolonged attack of bronchial asthma, extensive acute pneumonia, total right-sided pleurisy, tension pneumothorax;
- blockage of large branches of the pulmonary artery by blood clots, fat and tumor cells, and air;
- extensive infarction of the interventricular septum with transition to the right ventricle.
Symptoms of acute right ventricular failure include:
- signs of causative diseases;
- sudden shortness of breath and an increase in respiratory rate of more than 20 in one minute;
- pain in the right hypochondrium (when pressure is applied to the liver, the neck veins dilate);
- cyanosis of the skin, rapidly developing swelling of the legs;
- frequent weak pulse, possible bradycardia and decreased blood pressure.
When should you see a doctor?
In case of acute heart failure, you need to urgently consult a cardiologist to receive help in a hospital setting.
You should not expect dangerous complications from diseases that can lead to AHF. Dyspnea on exertion and at rest, increased blood pressure, any heart rhythm disturbances, chest pain, cough, peripheral edema should alert anyone who has not sought medical help for a full examination and treatment (Fig. 1).
Patients with cardiovascular pathologies and concomitant respiratory infections also need to consult a doctor to prevent severe complications.
Figure 1. When to suspect heart failure and see a doctor. Source: MedPortal
Emergency PCI
Emergency PCI, performed within the first two hours of hospital admission, is indicated in the following group of patients with non-ST segment elevation acute coronary syndrome:
1. The presence of ongoing or recurrent myocardial ischemia;
2. Dynamic changes in the ST segment (depression more than 1 mm or transient elevation (less than 30 minutes) more than 1 mm from the isoline);
3. The presence of deep ST segment depression in leads V2-V4, indicating ongoing transmural damage to the posterior myocardium of the left ventricle;
4. Acute heart failure (III-IV class according to Killip);
5. The presence of life-threatening arrhythmias (ventricular fibrillation, ventricular
tachycardia);
Diagnostics
To establish a diagnosis of AHF, you need an examination by a cardiologist with an assessment of complaints, objective examination data, measurement of blood pressure, pulse, listening to the heart and lungs, and palpation. To select the correct treatment, the doctor needs to identify the causative factors of the pathology, its type and severity. For these purposes the following are prescribed:
- ECG in 12 leads. An electrocardiogram must be performed as quickly as possible to determine rhythm disturbances, conduction disturbances and exclude a heart attack.
- Determination of blood saturation (oxygen saturation) using a pulse oximeter.
- Chest X-ray. In some cases, it confirms venous congestion in the lungs and edema, pleural effusion, pneumonia.
- Echo-KG. This is an ultrasound of the heart, which makes it possible to clarify the size of the heart chambers, the thickness of the myocardium, the condition of the valves, as well as determine myocardial contractility and cardiac ejection fraction.
- Holter monitoring is a daily continuous recording of an ECG using a special device to detect dangerous rhythm disturbances.
- Coronary angiography, computed tomography, MRI, transesophageal echocardiography are additional instrumental studies that are prescribed before cardiac surgery.
- Laboratory diagnostic methods.
Laboratory diagnostic methods most often determine:
- general blood characteristics - platelets, leukocytes, erythrocytes, hemoglobin and blood sugar levels, microelements (potassium, sodium and magnesium), biochemical metabolic parameters (urea, creatinine, bilirubin and transaminases);
- blood clotting indicators, including D-dimer and INR, which characterize the risks of thrombosis and the adequacy of therapy with anticoagulants;
- specific markers of damage to the heart muscle: level of troponins T and I, creatine phosphokinase (CPK-MB fraction);
- the level of specific natriuretic peptides to confirm the diagnosis of HF (acute and chronic, systolic and diastolic);
- blood gas composition (oxygen, carbon dioxide).
Treatment
AHF is an indication for emergency hospitalization. At the prehospital stage, before the ambulance arrives, it is important to provide assistance on the spot and eliminate additional stress. The patient needs to be seated comfortably, make sure there is an influx of fresh air, and measure blood pressure. When blood pressure is not lower than 100 mm Hg. Art. Give a nitroglycerin tablet under the tongue. To reduce venous return and stress on the heart, you can immerse your legs and arms in hot water. It will be useful to chew an aspirin tablet, and in case of a hypertensive crisis, take an antihypertensive drug.
In a hospital setting, treatment is carried out under constant monitoring of blood pressure, pulse, respiratory rate, saturation, ECG, diuresis, temperature until the condition stabilizes. Monitoring of many indicators in intensive care conditions is carried out through a special device - a cardiac monitor.
The approach to the treatment of AHF is always individual and depends on the form, cause and severity of heart failure, as well as pressure, pulse, saturation, heart rate and other important parameters. In case of cardiac arrest, cardiac massage and defibrillation are performed - “starting” the heart muscle using a high-voltage hardware current pulse.
Oxygen therapy for AHF
Oxygen therapy is the use of oxygen in treatment. It is indicated for insufficient saturation of blood and tissues with oxygen (hypoxia), which is often present in various forms of AHF. In this case, a moistened oxygen-air mixture is used, the composition and flow rate of which is determined by the doctor. In case of pulmonary edema, oxygen is supplied through alcohol or special substances that suppress foaming.
Drug treatment of AHF
Medicines are administered primarily intravenously. Medications used:
- Narcotic analgesics and sedatives. Suppress pain in acute myocardial ischemia, eliminate panic and fear, promote varicose veins and reduce preload on the heart.
- Vasodilators. They reduce pre- and afterload on the heart by dilating the veins and small arterioles of the capillary bed, and improve blood supply to tissues. These drugs are not used to lower blood pressure.
- Diuretics. They have a diuretic effect. They are able to quickly expand veins, eliminate pulmonary edema and reduce pressure in the arteries of the pulmonary and systemic circulation.
- Fibrinolytic agents for thrombolysis (dissolution of blood clots). Used for myocardial infarction. They are effective during the first 4–6 hours of the development of a heart attack (maximum - up to 12 hours).
- Anticoagulants prevent blood clots. Indicated for acute ischemia, rhythm disturbances, and risks of pulmonary embolism.
- Cardiotonic agents and vasopressors. Prescribed to stabilize pressure and increase myocardial contractility. Indicated for severe hypotension, used short-term. They can cause constriction of peripheral blood vessels and impair oxygenation of tissues; they can increase the need for oxygen in the heart muscle.
- Antiarrhythmic drugs.
- Beta blockers are used for certain conditions with persistent increases in blood pressure and tachycardia.
If AHF develops against the background of severe diseases of the respiratory system, blood, kidneys, or septic conditions, appropriate treatment of the causative pathology is required.
Unstable angina
Unstable angina (UA) is acute myocardial ischemia due to decreased coronary blood flow, the severity and duration of which is insufficient for the development of myocardial necrosis. But at any time, NS can transform into myocardial infarction. Based on symptoms and ECG data, early treatment clinicians are often unable to distinguish between UA and non-ST-segment elevation MI.
With NS, attacks of coronary pain increase in frequency, duration and intensity, exercise tolerance sharply decreases, and the effectiveness of nitroglycerin decreases. Along with this, ECG changes appear that were previously unnoted. NS also includes post-infarction (recurrent) angina (PS) - the occurrence or increase in frequency of angina attacks within 24 hours and up to 8 weeks after the development of MI.
It is divided into early (up to two weeks) and late post-infarction angina . In the presence of early PS, patient mortality; after myocardial infarction, increases from 2 to 17-50% over the course of 1 year. The main complication directly related to PSC is the expansion of the necrosis zone, observed in 20-40% of such patients.
ECG signs of unstable angina recorded during an attack include depression of the ST segment, less often - its rise above the isoelectric line, the appearance of tall T waves in the chest leads, their inversion, or a combination of these changes. Signs of ischemia are unstable and disappear either soon after the cessation of the attack of pain, less often - over the next 2-3 days.
In fairly common cases, the ECG remains within normal limits. In fact, angina pectoris differs from non-ST segment elevation myocardial infarction (NSTEI) only by the absence of an increase in blood biomarkers of myocardial necrosis in quantities sufficient for the diagnosis of myocardial infarction.
Recently, with the advent of highly sensitive tests (troponins, H-FABP) for markers of myocardial necrosis, the frequency of diagnosing non-ST segment elevation myocardial infarction has increased significantly. This suggests that the difference between these two forms of ACS is quite relative. Treatment of UA and non-ST segment elevation MI, at least with medication, should be the same.
Prevention
Primary prevention includes the prevention of major diseases that can lead to heart failure: coronary artery disease, hypertension, atherosclerosis. In addition to a healthy lifestyle, prophylactic low-dose aspirin and statins may be recommended for people at high risk.
In case of cardiovascular diseases, it is important to carry out secondary prevention measures:
- strictly follow the doctor’s recommendations for the treatment of rhythm disturbances, hypertension, coronary artery disease, correction of heart defects and other causative pathologies;
- reduce excess weight;
- normalize or compensate for impaired types of fat and carbohydrate metabolism with the help of diet therapy, rational physical activity and medications;
- carry out adequate monitoring of target blood pressure, lipid and blood sugar levels, blood coagulation system;
- give up alcohol;
- avoid excessive physical activity and emotional stress.
Emergency prevention includes preventing the occurrence of AHF in patients with cardiovascular diseases: with ARVI, anemia, upcoming surgical interventions, before emotional and physical stress.
All such patients should learn about self-care measures from their healthcare provider.