Blood pressure during a heart attack
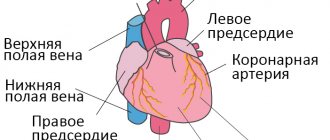
Blood pressure is the force with which blood is pumped in the circulatory system. When blood flow is restricted or completely blocked, the heart muscle lacks oxygen - leading to a heart attack.
.
During a heart attack, blood pressure can rise, fall, or remain constant, depending on how the body responds.
Increased blood pressure
Blood pressure may rise during a heart attack as hormones such as adrenaline
. Hormones are released when the fight-or-flight response is triggered during times of extreme stress or danger. This automatic reaction can make the heart beat faster and stronger.
Lower blood pressure
Blood pressure may drop if a person has a heart attack and the heart is too weak to support it because the muscles may be damaged. The intense pain a person may feel during a heart attack can also trigger an automatic reaction that can lead to low blood pressure and fainting.
Nausea
Nausea is a peculiar unpleasant sensation in the epigastric region, chest, and oral cavity, which often precedes vomiting and is often accompanied by general weakness, sweating, increased salivation, cold extremities, pale skin, and decreased blood pressure.
Causes of nausea
Possible causes not related to any disease:
1. Overeating and/or regularly eating foods that are very high in fat;
2. Side effects of medications and penetration of toxic substances into the body;
3. Psychogenic reactions: fear and anxiety, hysteria;
4. Kinetosis (seasickness), accompanied by a feeling of nausea and motion sickness;
5. Pregnancy (morning sickness normally goes away by the end of the first trimester);
6. Exposure to smoke, toxic fumes and various harmful substances;
7. Sunstroke, hyperthermia.
Diseases accompanied by nausea
Diseases that cause nausea are very diverse and can be associated with the digestive, nervous, reproductive, cardiovascular and endocrine systems.
Most often, nausea develops due to pathologies of the gastrointestinal tract, including:
1. acute surgical diseases: peritonitis, appendicitis, acute pancreatitis, acute intestinal obstruction, gastrointestinal bleeding, acute cholecystitis;
2. chronic diseases: gastroesophageal reflux disease (GERD) and hiatal hernia, gastritis, peptic ulcer of the stomach and duodenum, enterocolitis, duodenitis, cholelithiasis, inflammatory bowel disease (Crohn's disease, ulcerative colitis), irritable bowel syndrome, chronic pancreatitis ;
3. malformations of the gastrointestinal tract: narrowing of the pylorus (stenosis), fusion of a section of the gastrointestinal tract (atresia), developmental defects of the pancreas;
4. gastrointestinal tract infections: viral gastroenteritis, food toxic infections, helminthiases;
5. foreign bodies of the stomach, esophagus, intestines;
6. functional disorders accompanied by impaired motor function of the stomach and intestines;
7. liver diseases (hepatitis, cirrhosis of the liver);
8. food intolerances or food allergies.
In addition to disruption of the gastrointestinal tract, nausea can be caused by diseases of other organs and systems:
1. Diseases of the central nervous system: brain tumors and injuries, brain infections (encephalitis, meningitis), increased intracranial pressure.
2. Diseases of the cardiovascular system: hypertension, heart failure, myocardial infarction.
3. Diseases of the inner ear: Meniere's disease, labyrinthitis.
4. Diseases of the endocrine system: in diabetes mellitus – ketoacidosis; thyrotoxicosis, adrenal insufficiency, phenylketonuria.
5. Kidney diseases (urolithiasis, renal failure);
Nausea is associated with cancer treatment (chemotherapy and radiation therapy), imbalance of blood electrolytes, and migraines.
Nausea can be a manifestation of such emergency conditions as poisoning, diabetic ketoacidosis, intestinal obstruction, cerebral hemorrhage, acute cardiovascular pathology, renal failure, liver failure, sepsis.
Most often, nausea does not appear independently, but in combination with other symptoms: abdominal pain, belching, diarrhea, increased gas formation, dyspepsia, vomiting, muscle pain, dizziness, severe fatigue, fever and chills, headache, yellowing of the skin and sclera.
Particular attention should be paid to the combination of nausea with the following symptoms: black stools or the presence of blood in the stool, the presence of blood in the vomit, severe abdominal pain, difficulty breathing, fainting, impaired consciousness, high body temperature (more than 38.5 ° C), rapid pulse, frequent shallow breathing, severe headache, stiff neck. The appearance of these symptoms indicates the development of a life-threatening condition, if detected, you should immediately consult a doctor. You should also definitely see a doctor if you feel sick after a head injury.
Examination of a patient with nausea.
Nausea is a nonspecific symptom of many diseases; therefore, it has diagnostic value only in conjunction with other signs of the disease (for example, with signs of peritoneal irritation in acute appendicitis).
To determine the direction of the examination, it is necessary to conduct an active interview with the patient. So, if nausea is accompanied by other dyspeptic manifestations (belching, a feeling of heaviness in the epigastric region, etc.) and a relationship is identified between the occurrence of nausea and food intake, diseases of the digestive system should be assumed (gastritis, cholecystitis, pancreatitis, stomach tumor, etc.) and conduct a gastroenterological examination; when nausea is combined with headache, sensitivity or movement disorders, a neurological examination, etc. is necessary.
Determine what medications the patient took. Drugs that often cause nausea and vomiting include analgesics, cardiovascular drugs, hormonal agents, antibiotics, drugs that primarily act on the central nervous system, and antineoplastic agents. Drug use or withdrawal may also cause nausea or vomiting. If discontinuation of a drug is accompanied by the disappearance of nausea, we can assume that this disorder is associated with taking the drug, but it is necessary to ensure that there are no symptoms for a significant period of time after discontinuation of the drug.
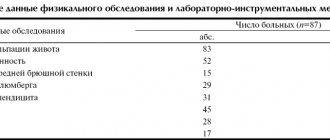
An objective examination reveals an “acute abdomen” and other life-threatening conditions. If the cause of nausea has not been established, a laboratory examination is performed:
1. general blood test (possible anemia, leukocytosis, accelerated ESR in case of gastric ulcer, duodenal ulcer, ulcerative colitis, etc.);
2. electrolytes, urea, creatinine (studied to diagnose kidney function and assess fluid and electrolyte disorders);
3. biochemical indicators of liver function: ALT (alanine aminotransferase), AST (aspartate aminotransferase), gamma glutamyl transpeptidase, total protein level in the blood, blood albumin, bilirubin);
4. blood glucose (normal values are 3.3-5.5 mmol/l, an increase in glucose levels indicates the likelihood of diabetes mellitus);
5. biochemical indicators of pancreatic function: alpha-amylase enzyme, lipase enzyme;
6. antibodies to Helicobacter pylori (to detect gastric ulcers associated with Helicobacter pylori infection);
7. In the analysis of stool when diagnosing diseases of the digestive system, the quantity, consistency and shape, color, smell, impurities, presence of mucus, pH are assessed; at the chemical level, the content of blood, bilirubin, stercobilin, and protein is determined;
8. The study of intestinal microflora is carried out when diagnosing intestinal dysbiosis.
The plan for further examination depends on the patient’s age and clinical manifestations. It should be especially careful if nausea and vomiting occur for a long time.
Pregnancy tests should be performed in women of childbearing age.
Sometimes a general urine test, a toxicological study, cultures, and a study of the function of the endocrine glands (TSH and thyroid hormone levels, morning fasting cortisol levels) are needed.
To exclude diseases of the gastrointestinal tract, diseases of the liver and biliary tract, a survey radiography of the abdominal cavity, examination of the stomach and intestines with barium, ultrasound of the abdominal organs, CT and endoscopic examinations are performed.
FEGDS (fibrogastroduodenoscopy) is intended primarily to exclude obstruction, gastric or duodenal ulcers or other organic pathology.
Colonoscopy is necessary to identify nonspecific ulcerative colitis, Crohn's disease, chronic non-ulcerative colitis, if a tumor process is suspected.
pH-metry is carried out to study the secretory function of the stomach if gastritis or gastric ulcer is suspected.
Rectomanoscopy is used for diseases of the rectum.
If a neurological disorder is suspected (migraine, increased intracranial pressure, pathology of the inner ear), which can cause constant or periodic nausea, a clinical neurological examination should be performed, to exclude increased intracranial pressure by examining the fundus of the eye or conducting magnetic resonance imaging of the brain.
Sometimes esophageal manometry, 24-hour esophageal pH-metry, a study of gastric motility and evacuation function, and sometimes electrogastrography and a study of small intestinal motility are required to make a diagnosis.
If psychiatric illnesses that cause constant or recurrent nausea, anxiety disorders, depression, or eating disorders are suspected, a consultation with a psychiatrist is prescribed.
Treatment of nausea
Since nausea is a symptom, its treatment method depends on the cause or underlying disease. If you suspect a disease, it is important not to self-medicate, since nausea may be associated with emergency conditions or the initial manifestation of severe pathology, which require immediate consultation with a doctor and the initiation of specific treatment under medical supervision.
If the cause is not related to the disease, it is necessary to eliminate the harmful factor (sun, smoke, excess food) as quickly as possible.
For seasickness, it is possible to use scopalamine in the form of a skin patch 5-6 hours before the start of the trip.
During pregnancy, rest and rest are recommended; it is possible to use meclozine orally 25 mg 2 times a day or in suppositories 50 mg.
To eliminate nausea in such cases, it is possible to use folk remedies:
• For nausea and vomiting in pregnant women, it is recommended to eat little and often. In the morning, drink only water with lemon or slightly sweetened juice, and eat crackers.
• A proven remedy for nausea is green tea.
• Grate ginger root and add to dishes.
• Before meals, drink 0.25-0.5 tablespoons of fresh potato juice.
• Pour a glass of boiling water over a tablespoon of peppermint leaf. Let it brew for two hours. Take the tincture one tablespoon three times a day.
• Boil a teaspoon of dill seeds in 200 ml of water. Take in case of poisoning or stomach upsets.
• Pour a glass of boiling water into 4 teaspoons of dry crushed lemon balm herb. Leave for several hours. Drink ½ cup four times a day before meals.
• Pour 400 ml of cold water into two teaspoons of three-leaf watch, leave for eight hours. Use within 24 hours. Used for nausea to stimulate digestion.
Possible complications
In some cases, if left untreated, nausea can lead to complications such as dehydration (impaired water and electrolyte balance in the body) and nutritional deficiencies in the body. As a rule, this is due to the inability to retain water or food in the body, as well as a lack of appetite.
Which doctor should I contact if I have nausea?
Depending on the accompanying symptoms, you may need to consult a therapist, gastroenterologist, neurologist, psychiatrist, toxicologist, endocrinologist, or allergist.
Blood pressure and heart attacks
If high blood pressure is left unregulated, it can increase the risk of a heart attack. High blood pressure can be an indicator of how hard the heart has to work to pump blood throughout the body through the arteries, so doctors keep an eye on it. The accumulation of fat, cholesterol and other substances in the arteries is called plaque. Over time, the plaque hardens, causing the arteries to narrow. This narrowing means that more pressure is required to push blood through the network of blood vessels. When plaque breaks away from the artery wall, a blood clot forms around it. Heart attacks can occur because plaques or blood clots disrupt or block the blood supply to the heart.
However, high blood pressure is not always a serious health problem. Even healthy people can experience high blood pressure from time to time due to exercise or stress.
Heart failure and gastrointestinal tract
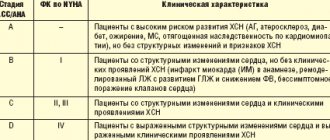
Pathology of the gastrointestinal tract develops in people with clinically manifested heart failure (HF) in a clinically significant percentage of cases, while the quality of life of patients sometimes significantly deteriorates regardless of the underlying disease. It seems appropriate to us to reflect the entire spectrum of “gastroenterological” symptoms, arranging them according to the organ principle.
Oral cavity . An increase in the volume of the tongue is often the only “dental” symptom pathognomonic for heart failure. Although this condition correlates with the severity of heart failure, it is currently extremely rare. Other symptoms—pathological elements on the mucous membrane, tongue, and lips—are associated with decreased immunity, nutritional deficiency, or are independent diseases not causally related to HF [1].
Oropharyngeal dysphagia (OD) is a complication of the early postoperative period in cardiac surgery [2]. Thus, in a study of 1042 patients who underwent heart surgery for various reasons, OD was detected in more than 4% of patients. At the same time, oral dysphagia was identified in 6.4% of cases, pharyngeal dysphagia in 22.6%, and in the remaining patients dysphagia was of a mixed nature [3]. Independent risk factors for the occurrence of OD in the postoperative period are: old age, diabetes mellitus, renal failure, hyperlipidemia and the presence of clinical symptoms of chronic heart failure before surgery. It is noted that the cost of treating one case of OD is the highest in the presence of CHF [3].
Esophagus and stomach . Episodes of gastroesophageal reflux (GER) can be divided into 2 groups: daytime, or vertical GER, and nighttime, or horizontal GER.
In 2001, a large study was conducted in the USA, the purpose of which was to identify the frequency of episodes of nocturnal GER and its impact on the quality of life of patients with various diseases.
It has been shown that in cardiac patients, 74% of GER episodes occur at night. At the same time, physical (p < 0.001), mental (p < 0.001) well-being and overall quality of life (p < 0.001) significantly worsened. It is also noted that the decrease in quality of life in patients in this group due to nocturnal episodes of GER is greater than with symptoms of arterial hypertension, and is comparable to the change in this indicator associated with the presence of angina and chronic heart failure [4].
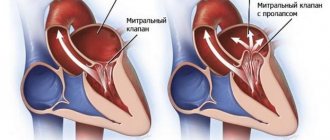
Dysphagia in patients with heart failure is also of esophageal origin. The reasons for this are: thoracic aortic aneurysm, atherosclerotic deformation of the aorta, changes in the configuration of the subclavian arteries, dilatation of the left atrium [5].
An endoscopic examination of dysphagia of esophageal etiology usually reveals pulsations of its wall, coinciding with the peripheral pulse, and compression of the lumen of the digestive tube in the middle parts of the esophagus. Changes in the mucous membrane are usually not observed, and the endoscope passes freely through the narrowed area. The presence of such stenotic changes in the distal and proximal parts indirectly indicates dilatation of all chambers of the heart [6].
When examining with barium during dilatation of the left atrium, a posterior deviation of the esophagus is determined simultaneously with a violation of the passage of suspension through the lumen of the tube.
Esophageal manometry reveals an area of high pressure that occurs at a cyclic rate depending on the heart rate. Periodic oscillations are characteristic of patients with sinus rhythm, irregular oscillations are characteristic of patients with atrial fibrillation [7].
Before and after the high-pressure zone, peristaltic waves are usually not changed, which, according to some authors, indicates a causal relationship between compression and dysphagia [8]. However, ischemia of the Meissner and/or Auerbach plexuses, as well as compression of the vagus nerve trunk, can significantly alter esophageal motility [9].
Liver . Liver cells are very sensitive to lack of oxygen, and in the presence of low blood pressure and decreased cardiac output, changes in the morphology and functional capacity of liver tissue are observed. Due to anatomical features, the left lobe of the liver is most sensitive to hypoxia [10].
Hypoxia causes degeneration of hepatocytes in zone 3, dilation of sinusoids and slower bile secretion. This occurs despite the high oxygen absorption coefficient, due to the characteristics of the blood circulation. The absorption of oxygen from the blood of the sinusoids increases compensatoryly. A slight impairment of oxygen diffusion may result from sclerosis of the space of Disse [11].
A decrease in blood pressure with low cardiac output leads to necrosis of hepatocytes. The increase in pressure in the hepatic veins and the associated stagnation are determined by the level of central venous pressure [7, 11, 12]. Moreover, even minor adverse changes in hemodynamics (hypotension, embolic complications, physical activity) lead to increased damage to hepatocytes [7].
Patients are usually slightly icteric. Severe jaundice is rare and is found in patients with chronic heart failure due to ischemic heart disease or mitral stenosis. In hospitalized patients, the most common cause of elevated serum bilirubin concentrations is heart and lung disease. Long-term or recurrent heart failure leads to increased jaundice. No yellowness is observed in edematous areas, since bilirubin is bound to proteins and does not enter the edematous fluid with a low protein content [11].
The patient may complain of pain in the right abdomen, most likely caused by stretching of the capsule of the enlarged liver. The edge of the liver is dense, smooth, painful, and can be determined at the level of the navel.
Increased pressure in the right atrium is transmitted to the hepatic veins, especially with tricuspid valve insufficiency. When using invasive methods, the curves of pressure changes in the hepatic veins in such patients resemble the pressure curves in the right atrium. Palpable expansion of the liver during systole can also be explained by pressure transmission. In patients with tricuspid stenosis, presystolic pulsation of the liver is detected. Liver swelling is detected by bimanual palpation. In this case, one hand is placed in the projection of the liver in front, and the second - on the area of the posterior segments of the lower right ribs. An increase in size will make it possible to distinguish liver pulsation from pulsation in the epigastric region, transmitted from the aorta or hypertrophied right ventricle. It is important to establish pulsation with the phase of the cardiac cycle [7, 11].
In patients with heart failure, pressure on the liver area leads to increased venous return. The impaired functionality of the right ventricle does not allow it to cope with the increased preload, which causes an increase in pressure in the jugular veins. In patients with occlusion or block of the hepatic, jugular or main veins of the mediastinum, reflux is absent.
Pressure in the right atrium is transmitted to the vessels up to the portal system. Pulsed duplex Doppler can detect increased portal vein pulsation; in this case, the amplitude of pulsation is determined by the severity of heart failure [13]. However, phasic fluctuations in blood flow are not found in all patients with high pressure in the right atrium [14].
A connection has been established between ascites and significantly increased venous pressure, low cardiac output and severe necrosis of hepatocytes in the area of the worst blood circulation. This combination is found in patients with mitral stenosis, tricuspid valve insufficiency or constrictive pericarditis. In this case, the severity of ascites may not correspond to the severity of edema and clinical manifestations of congestive heart failure.
Signs of portal hypertension (except for splenomegaly) are usually absent, except in patients with severe cardiac cirrhosis in combination with constrictive pericarditis.
Liver failure is rare, but this syndrome may be the only clinical manifestation of unrecognized cardiac pathology [15].
Biochemical changes are usually moderate and are determined by the severity of heart failure. Alkaline phosphatase activity may be slightly elevated or normal. There may be a slight decrease in serum albumin concentration, which is facilitated by protein loss through the intestine [11].
Small intestine. In a study of 187 patients with myocarditis, antiendomysial antibodies were identified in 9 (4.4%) cases, which are a specific marker of gluten enteropathy (intestinal sprue). In all cases, endoscopic and histological evidence of intestinal damage was obtained. In this group of patients, 55% had clinical signs of chronic heart failure [16]. Therapy with immunosuppressants and the prescription of a specific diet made it possible to achieve a simultaneous improvement in the functional capacity of the heart and the immunological activity of the process.
The presence of right ventricular failure is associated with an increase in central venous pressure, a factor that causes significant loss of protein from the digestive tube. This occurs due to unfavorable changes in the lymphatic vessels (congestion) of the intestinal wall. Considering the fact that in most cases, even with severe heart failure, no clinically significant loss of protein is observed, a number of authors come to the conclusion that for the development of protein-losing enteropathy, a special premorbid background is required - in particular, the presence of changes in the lymphatic vessels not related to cardiac function intestines (for example, congenital intestinal lymphangiectasia) [7].
Intestinal protein loss occurs most frequently with constrictive pericarditis, but other causes include congenital pulmonary stenosis, tricuspid regurgitation, carcinoid syndrome, and atrial septal defect [7, 17]. Diarrhea develops in approximately 50% of cases, steatorrhea is extremely rare. We should not forget that hypoalbuminemia may be associated with a general increase in fluid in the body (the “dilution” phenomenon).
The diagnosis is based on clinical and laboratory parameters (hypoproteinemia and hypoalbuminemia) and is confirmed by one of the 3 methods listed below: studying the excretion of albumin labeled with 51Cr; biopsy of the small intestinal mucosa; determination of fecal α1-antitrypsin (molecular weight and total amount, carried out in parallel with the study of albumin).
Colon . Although there are reports of the simultaneous presence of chronic heart failure and a number of diseases of the large intestine, especially its rectosigmoid region, there have been no studies of this issue that meet the requirements of evidence-based medicine. At the moment, it is impossible to speak with confidence about the presence of specific or associated changes in the final part of the digestive tube in chronic heart failure.
For questions regarding literature, please contact the editor.
S. N. Tereshchenko , Doctor of Medical Sciences, Professor I. V. Zhirov , Candidate of Medical Sciences MGMSU, Moscow
Signs and symptoms of a heart attack
The most common symptoms of a heart attack are:
- chest pain
- discomfort in the upper body
- dyspnea
Other signs and symptoms include:
- sweating
- nausea
- anxiety
- swelling in the legs
Symptoms may vary by gender, but the most common heart attack symptom for both women and men is chest pain or discomfort.
Doctors believe women may experience different symptoms. For example, they may experience shortness of breath, nausea, and back and jaw pain.
Heart disease is the leading cause of death in women. Despite this, many women believe their symptoms are caused by less serious illnesses, including acid reflux, the flu, or simply aging.
Nausea and heart pain
Pain and discomfort appearing in the heart area are an alarming sign. In this way, diseases often appear that pose a serious danger to human health and life. Heart pain and nausea often occur together. How should one act in such a situation, and what pathologies can these symptoms indicate?
Causes of nausea and pain in the heart area
It should be remembered that pain and discomfort in the heart area primarily signals that a vital organ is in danger. Often the appearance of symptoms such as nausea and heart pain requires immediate medical attention. Along with the above symptoms, patients often experience shortness of breath, severe weakness, anxiety, and fear.
Nausea and heart pain can occur simultaneously when the gastrointestinal or cardiovascular system is affected. The most common causes of such symptoms are the following pathologies:
- heart failure;
- attack during myocardial infarction;
- hypertensive crisis;
- vegetative-vascular dystonia;
- acute diseases of the pancreas or liver;
- bronchitis and pneumonia in acute severe form.
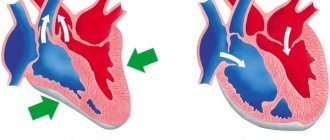
Heart failure may include chest pain and nausea. These symptoms are caused by several factors: disturbances in the anatomy of the muscle tissue of the heart, deterioration in the functioning of this organ, the appearance of swelling in the abdominal cavity and chest, as well as increased intracardiac pressure. All this leads to nausea and pain in the heart.
During myocardial infarction, pain and painful, prolonged nausea may appear some time before the attack. This period can be several days. The same symptoms are observed with the acute development of pathology. In addition to these two signs, during an attack caused by myocardial infarction, others are noted: weakness, vomiting, tachycardia, a sharp rise in blood pressure followed by a decline, gradually increasing shortness of breath and an increasing feeling of burning and pain in the chest space. Patients often complain of an unreasonable feeling of fear and anxiety; cases of fainting during an attack are widespread. It is also possible for the pathology to be asymptomatic, in which its only manifestation is nausea.
A hypertensive crisis is a sudden rise in blood pressure. Symptoms of this condition include severe pressing pain in the heart, nausea that leads to vomiting but does not bring relief, and dizziness.
The diagnosis of “vegetative-vascular dystonia” is quite common in our country, but in many other countries it is not made. According to the international classification, similar conditions in which there are signs of disruption of the normal functioning of the autonomic nervous system are called somatoform dysfunctions or disorders. Symptoms that indicate vegetative-vascular dystonia are insomnia, pressure instability, tachycardia, vomiting, nausea and heart pain. All these signs, most often, are of a psycho-emotional nature. There were practically no complications or consequences observed. However, the appearance of such symptoms requires careful attention, a comprehensive examination and, if necessary, proper treatment.
In some cases, pathologies of the gallbladder, pancreas and liver are manifested by pain that is localized or radiates to the heart area. With such diseases, frequent nausea may occur that does not lead to vomiting. Pain can affect the hypochondrium and abdomen. A symptom of gallbladder damage is bitterness in the mouth.
Sharp pain in the chest and nausea are frequent companions of inflammatory diseases of the lower respiratory system. Pain with pneumonia and bronchitis is caused by strong constant overstrain of the intercostal muscles, which occurs with prolonged painful coughing. Nausea is associated with general damage to the body by toxins released by pathogenic microorganisms. In addition, this phenomenon can be a side effect of medications taken. You can determine whether pneumonia or bronchitis is the cause of chest pain and nausea by paying attention to the presence of other symptoms. Thus, increased temperature, increased sweating, chills, runny nose and other signs of damage to the upper respiratory system indicate respiratory diseases.
What to do for heart pain, nausea and dizziness
The appearance of nausea, heart pain, vomiting, weakness must be treated carefully; these symptoms should not be left to chance, as they can have the most dire consequences. A qualified doctor and the modern level of diagnostics allow you to quickly determine the cause of the problem, and then prescribe the necessary course of treatment. In each specific case, a different treatment is prescribed, so you cannot be treated on the advice of friends and neighbors.
The specialist must, in addition to recommendations for treating the underlying disease, prescribe therapy in order to cope with unpleasant symptoms. In addition, he gives advice on organizing a daily routine, necessary rest, opportunities for physical activity and a diet that should be followed.
Urgent medical help should be sought if the following warning signs are present:
- heart pain and nausea do not subside after taking nitroglycerin tablets;
- in addition to nausea and pain in the heart, there is severe shortness of breath, very high blood pressure, the appearance of cold sweat, inexplicable anxiety, fear and restlessness;
- the duration of pain in the heart exceeds a quarter of an hour.
You can get rid of nausea and chest pain only after identifying the causes of their occurrence. Since different pathologies require the use of different drugs and treatment methods.
In case of functional disorders of the heart and blood vessels, you should take medications that lower pressure and normalize the functioning of the heart muscle. The therapeutic complex also includes drugs that have a positive effect on the condition of blood vessels and blood composition.
For vegetative-vascular dystonia, complex treatment is prescribed, including medications that improve the functioning of the nervous system and sedatives. Other treatment methods are also prescribed, such as physiotherapy, therapeutic massage and exercise, reflexology, etc.
A disease such as myocardial infarction requires urgent medical care, which can only be provided in a hospital setting. The course of treatment, its duration and the means used depend on the individual data of the patient and the extent of damage to the heart muscles. The chances of a favorable outcome increase significantly if you consult a doctor in a timely manner (less than 10-12 hours).
Treatment of inflammatory pathologies of the respiratory system depends on the nature of the disease: viral or bacterial. In addition to antivirals or antibiotics, it includes vitamins, mucolytics and detoxification therapy. It is important to choose the right antibiotic for treatment. Although there are broad-spectrum antibiotics that are quite effective, drugs prescribed based on the results of microbiological tests are much more effective.
Diseases of the pancreas, liver and gall bladder require specific treatment to restore the affected organs. To get rid of nausea in such cases, take antiemetics, for example, Zoloft, Cerucal or others. A thorough examination of the patient is imperative.
Causes of pain in the heart area
It is necessary to clearly understand that pain in the heart and nausea are, first of all, alarming signals that make it clear to a person that vital organs are in serious danger, and the current situation requires the use of immediate measures. One way or another, pain localized in the chest and nausea are symptoms of serious diseases; they should not be ignored, because along with them shortness of breath, a feeling of weakness, fear, and anxiety may appear.
Nausea and chest pain can appear simultaneously if several pathologies occur at once: cardiovascular and gastrointestinal. However, most often pain and nausea have the following causes:
• vegetative-vascular dystonia
• heart failure
• heart attack (myocardial infarction)
• pneumonia, bronchitis
• hypertensive crisis
• diseases of the liver, pancreas
Vegetative-vascular dystonia is a common diagnosis in Russia, but in Sweden and Europe there is no such diagnosis. Similar conditions that manifest themselves with a large number of symptoms associated with dysfunction of the autonomic nervous system and neuroregulation of the body in Swedish medicine are designated as somatoform disorders or dysfunctions (Somatoforma störningar, in the international classification of diseases has the number F45). Among the common symptoms of vegetative-vascular dystonia, people often find pain in the heart area, nausea, vomiting, insomnia, tachycardia, and unstable blood pressure. The symptoms that arise speak more about a mental than a physical illness, and almost never lead to serious consequences, although they require a thorough examination and, possibly, adequate therapy.
Nausea and chest pain may be signs of heart failure. Anatomical changes in the heart muscle and a decrease in the physiological functions of the organ contribute to the appearance of edema in the chest and abdominal cavity, and the pressure inside the heart increases. All this leads to pain in the chest, as well as nausea.
A heart attack (myocardial infarction) is sometimes preceded several days by the appearance of pain in the heart and painful nausea. Similar symptoms are also characteristic of the acute process of developing the pathology of a heart attack. Vomiting, nausea, weakness, low blood pressure replace hypertension, tachycardia, while shortness of breath, a feeling of fear and burning pain in the chest increase, and cases of fainting are not uncommon. Often nausea is practically the only symptom of myocardial infarction, and the disease develops painlessly.
Sharp chest pains and a feeling of nausea often accompany bronchitis and pneumonia. Pain in such cases occurs after a prolonged unproductive cough due to overstrain of the intercostal muscles. Nausea is a consequence of general intoxication due to the activity of microorganisms and taking medications. A sign that heart pain and nausea are symptoms of inflammatory diseases of the upper respiratory tract is the presence of elevated body temperature, chills, and increased sweating.
A sharp jump in blood pressure characterizes a hypertensive crisis. In this case, patients experience pressing pain in the heart area, nausea, vomiting, which does not bring relief, and dizziness.
With diseases of the liver, gallbladder and pancreas, pain can be localized in the chest area, and frequent nausea without vomiting also occurs. Often pain is felt in the hypochondrium area, and bitterness may appear in the mouth.
What to do
Chest pain, vomiting, nausea, weakness should not be ignored, they cannot be ignored. Timely diagnosis and consultation with a competent specialist can differentiate the cause of symptoms and direct all therapeutic measures to eliminate the disease. Therefore, it is necessary to find out from your doctor what you can take for nausea. In each specific case, the answer to this question will be different.
It is imperative to follow the doctor’s recommendations regarding the treatment of the underlying disease that causes unpleasant symptoms, as well as adhere to the proposed diet, exercise regimen and rest.
There is no need to hesitate to seek emergency help if there are threatening symptoms:
- heart pain does not stop for more than 20 minutes;
- pain does not go away after taking nitroglycerin;
- an attack of nausea and heart pain is accompanied by high blood pressure, cold sweat, shortness of breath, and fear.
How to Deal with Chest Pain and Nausea
A prerequisite for the successful elimination of chest pain and nausea is an accurate diagnosis of the patient’s condition. After all, to relieve nausea in case of dysfunction of the heart and blood vessels. it is necessary to take medications that lower blood pressure, correct heart function, improve the condition of blood vessels and the rheological properties of the blood. Therapy for vegetative-vascular dystonia is complex and includes sedatives, drugs that optimize the functioning of the nervous system, as well as individual organs and systems. In addition, they also resort to non-drug treatment methods: therapeutic massage, physiotherapeutic procedures, reflexology.
Myocardial infarction requires urgent and competent measures in a hospital setting. Therapy, its duration, and volume directly depend on the area of damage to the heart muscle. The success of treatment is much greater if it is started for the first time 12 hours
Pneumonia and bronchitis, in addition to antimicrobial and antiviral therapy, always includes detoxification agents, vitamins, and mucolytic drugs. Despite highly effective broad-spectrum antibiotics, the most acceptable is the prescription of drugs based on microbiological research data.
For diseases of the liver and pancreas, the use of drugs that restore the function of these organs, as well as antiemetic drugs (Cerucal, Zoloft), helps quite well against nausea. Additional examination methods will not be superfluous; they will help you individually select the necessary therapy.
The causes of heart pain and nausea are varied. By listening to the “voice” of one’s own body, a person is able to timely catch signals of dysfunction of organs and systems, and by consulting a doctor, find the right solution to the problem that has arisen.
Why does my heart hurt?
What is a silent heart attack?
An asymptomatic heart attack, as the name suggests, may have few or no obvious symptoms. In some cases, people may feel tired, have flu-like symptoms, or experience indigestion or discomfort in the chest, back, arms, or jaw. This type of heart attack can sometimes be worse than a normal one, as people who have it may not receive any treatment.
An asymptomatic heart attack can only be diagnosed using an electrocardiogram.
When to see a doctor
People should see a doctor if they experience chest pain, discomfort, or the following symptoms:
- pain in one or both arms
- pain in the back, neck, jaw or stomach
- dyspnea
- sweating
- nausea
- dizziness
If your blood pressure rises, when the systolic pressure is above 180 and the diastolic pressure reaches 110 or more, you should consult a doctor. Blood pressure in this range puts people at greater risk of heart attack.
Related article: High blood pressure and low pulse - what could be the reason?
Serious question: what happens to the heart during an angina attack?
Have you heard of such a diagnosis as “angina pectoris”? Such an unusual term actually existed before. So what was it that “compressed the chest” of a person?
With questions about a common disease of modern civilization - angina pectoris, we visited our regular consultant, general practitioner, cardiologist at the Expert Voronezh Clinic, Angelina Anatolyevna Kalinina.
— Angelina Anatolyevna, what is angina pectoris and what is the danger of this disease?
Angina is a syndrome that is manifested by a feeling of discomfort or pain in the chest, often of a squeezing, burning or pressing nature. In most cases, they are localized behind the sternum and can “give” to the left arm, neck, lower jaw, under the scapula, and to the epigastric region. Usually the pain stops with rest after 3-5 minutes or a few seconds or minutes after taking nitroglycerin under the tongue in the form of tablets or spray.
How to distinguish between heart pain and pain due to intercostal neuralgia? The story is told by neurologist, leading specialist of the neurology department of the Expert Kursk Clinic Natalya Vladimirovna Umerenkova
Angina pectoris is one of the types of coronary heart disease (CHD). It is dangerous because there is a risk of myocardial infarction.
Read material on the topic: Coronary heart disease: diagnosis and treatment
- What are the causes of angina?
The cause of classic angina pectoris in more than 90% of cases is atherosclerosis of the heart arteries. Sometimes angina is caused by vasospasm (vasospasm) or functional disorders at the microcirculation level. Often there is a combination of the above reasons.
Risk factors for the occurrence of angina pectoris are divided into so-called modifiable (i.e., those that a person can influence) and non-modifiable (those that cannot be changed).
Modifiable factors include dyslipidemia, high blood pressure, diabetes mellitus, smoking, excessive consumption of alcohol-containing beverages, physical inactivity, obesity, dietary patterns, etc.
Non-modifiable are male gender, age, hereditary predisposition.
What can cause chest pain? These are cases when a person subjected himself to physical activity, walked quickly, climbed a mountain or stairs, or carried heavy loads. Pain can also appear with increased blood pressure, exposure to low temperatures, overeating, and stress.
Read the material on the topic: It's off scale! Looking for reasons for high blood pressure
— By what signs can angina be recognized?
A detailed interview with the patient is very important. There are typical, probable (or atypical) angina, as well as cardialgia (in which the pain is not associated with a deterioration in the blood supply to the myocardium).
Symptoms of typical angina include chest pain or specific discomfort. Caused by physical activity or psycho-emotional stress. They go away with rest or after using nitroglycerin. With this type of angina, all three manifestations must be present.
In atypical angina, only two of the three are present.
With cardialgia, one or none of the above symptoms are noted.
Taking this into account, either a cardiologist or another specialist works with the patient and further searches for the causes of pain in the heart area.
- What is angina pectoris?
The following types are distinguished: stable, unstable and spontaneous.
Separately, there is the so-called cardiac X-syndrome (X-syndrome, otherwise known as microvascular angina). With it, there is a combination of classic signs of angina pectoris with unchanged heart arteries. This species has not yet been fully studied.
— What happens to the heart during an angina attack?
The process develops as follows. Initially, the blood supply to the myocardium is disrupted, later metabolic and electrophysiological “shifts” are noted in it. Then the heart’s ability to relax is impaired, and then to contract. And only then does pain appear and corresponding changes on the electrocardiogram.
Read the material on the topic: Why is ultrasound of the heart prescribed?
— How to provide emergency assistance during an angina attack?
The drugs taken are short-acting nitrates (tablets or spray), under the tongue. It is better to take them in a sitting or lying position (to prevent low blood pressure, dizziness and possible falls associated with this). Tablet dosage: 0.5 mg. In total, up to 3 tablets are taken - 1 tablet every 5-7 minutes. You need to focus on the disappearance of pain.
Nitroglycerin should not be used if the “upper” (systolic) blood pressure is less than 90 mmHg. rt. Art.
This blood pressure should also be monitored while taking nitroglycerin, even if it was initially above 90-100 mm. rt. Art.
If the pain does not subside within 15-20 minutes while taking nitroglycerin, you must call an ambulance to rule out myocardial infarction.
— Are angina pectoris and coronary heart disease the same thing or is there a difference between them?
Angina pectoris is one of the types of coronary heart disease.
— Who has angina pectoris more often: men or women?
In general, its frequency increases with age in both sexes.
In middle age, it is angina pectoris (and not ischemic heart disease in general) that occurs more often in women, probably due to the higher prevalence of vasospasm and cardiac syndrome X. For older age groups, the situation is the opposite, i.e. both ischemic heart disease in principle and angina pectoris as a special case are more often observed in men.
- Who is predisposed to developing angina? What risk factors provoke the development of angina?
These are the modifiable or non-modifiable factors that we talked about earlier.
— Angelina Anatolyevna, how is angina diagnosed?
Firstly, a thorough collection of complaints and anamnesis (with clarification of the nature of the pain, its location, duration, conditions of occurrence, the effect of taking various medications - in particular nitroglycerin, if taken).
Upon examination, signs of atherosclerosis, heart failure, high blood pressure, and obesity may be detected as additional risk factors.
A general blood and urine test, lipidogram (total cholesterol and its fractions, triglycerides), glucose, creatinine clearance are performed. In unstable and acute conditions, markers of myocardial destruction (troponins T and I, creatine phosphokinase (CF fraction).
Instrumental diagnostics. Invasive and non-invasive methods are used here.
The first one is an ECG. How is angina visible on it? These are specific ST segment changes.
Echocardiography and ultrasound duplex scanning of the brachiocephalic arteries are mandatory.
Load tests - bicycle ergometry and treadmill test.
Holter monitoring. It is performed when stress tests are contraindicated, if it is impossible to record an ECG at the time of pain, etc.
Read the material on the topic: Holter (24-hour) ECG monitoring - complete instructions for the patient
Stress echocardiography (ultrasound of the heart under stress).
Perfusion scintigraphy with exercise.
Invasive methods. The “gold standard” for imaging diagnosis of atherosclerosis of the heart arteries is coronary angiography (especially in those at high risk of cardiovascular complications and death), as well as multislice computed tomography with assessment of coronary calcium, or calcium scoring.
— What is the purpose of treatment for angina pectoris? Is this diagnosis an indication for surgery?
The main goals are to eliminate manifestations and improve the prognosis.
If symptoms cannot be eliminated with drug therapy, it is recommended to refer the patient for a consultation with a cardiovascular surgeon to determine the possibility of surgical treatment of angina.
— Is angina responding well to treatment? Is it possible to cure it completely?
Treatment of angina pectoris at the present stage of medical development is effective. You can either significantly reduce its manifestations or eliminate them completely. At the same time, even after surgical treatment with complete restoration of adequate blood supply to the myocardium, drug therapy continues indefinitely, because the risk of cardiovascular complications remains very high.
— Can angina be resisted? How to properly prevent this disease and at what age should it start?
The main measures are aimed at preventing the occurrence and progression of atherosclerosis and, accordingly, damage to the arteries of the heart. Those. it is the effect on modifiable risk factors. It is necessary to stop smoking, control weight, and eat rationally. If you have diabetes, you need to achieve your blood glucose targets. Provide rational, regular physical activity. Monitor blood pressure. Regularly take medications prescribed by a cardiologist or cardiac surgeon and be observed by these specialists.
You may also be interested in:
Heart, why don't you want peace? What causes tachycardia?
How to keep your heart healthy?
What do you need to know about health before buying a gym membership?
For reference:
Kalinina Angelina Anatolevna
In 2007 she graduated from the Voronezh State Medical Academy named after. Burdenko.
From 2007 to 2008 she completed an internship in therapy, in 2010 she underwent professional retraining in the specialty “General Medical Practice (Family Medicine)”, and in 2017 – in the specialty “Cardiology”.
Since 2015, he has held the position of general practitioner at Clinic Expert Voronezh. Reception is conducted at the address: st. Pushkinskaya, 11.