Consultation with a cardiologist – RUB 1,750.
- What is extrasystole?
- Classification
- Signs of arrhythmic syndrome
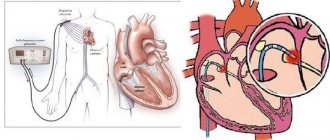
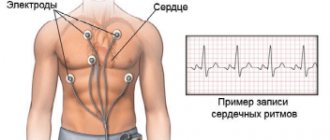
- Diagnostics
- Treatment of extrasystole
Extrasystole
– the most common type of arrhythmias, in which an extraordinary contraction of the entire heart or its parts occurs. It occurs when the mechanism of transmission of a nerve impulse from the sinus node to the ventricles of the heart is disrupted and is characterized by the presence of a focus of activity outside the main pacemaker of the heart - the sinus node.
It is believed that extrasystole is observed in every person at some periods of life. With a single ECG recording in a group of healthy individuals, it is detected in 1.5-5% of cases. Daily monitoring reveals supraventricular extrasystoles in 14-91% and ventricular extrasystoles in 46-89% of healthy individuals Source: Oslopova Yu.V. Treatment of extrasystole / Yu.V. Oslopova [and others] // Practical medicine. - 2010. - No. 5 (44). — P. 16-26. . Although most of them are represented by single extrasystoles, complex forms can also be detected.
The clinical significance of extrasystole is almost completely determined by the nature of the underlying disease, the degree of organic damage to the myocardium, and its functional state. In organic heart diseases, even the presence of more than 10 ventricular extrasystoles per hour significantly increases the risk of sudden death from fatal ventricular arrhythmias Source: Oslopova Yu.V. Treatment of extrasystole / Yu.V. Oslopova [and others] // Practical medicine. - 2010. - No. 5 (44). — P. 16-26. . In the absence of organic heart disease, extrasystole does not pose a threat to life.
Types of extrasystole
Extrasystole is classified according to the location of the abnormal focus of activity:
- ventricular;
- ventricular-atrial;
- atrial.
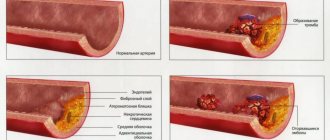
Due to the occurrence:
- extrasystole of functional origin - as a result of the use of nicotine, alcohol, nervous overstrain;
- extrasystole of organic origin - myocardial infarction, cardiomyopathy, heart defects, coronary heart disease;
- extrasystole of toxic origin - as a result of the use of certain medications, during a prolonged febrile state.
Also distinguished:
- bigeminy - characterized by the occurrence of extrasystole immediately after a normal contraction;
- trigeminy - one normal contraction is followed by two extrasystoles, or two normal cardiac complexes are followed by one extrasystole;
- quadrigeminy - three normal contractions occur, followed by an extraordinary contraction.
M.A. Gurevich Department of Therapy, Faculty of Internal Medicine, MONIKI, Moscow
The goals of treatment for arrhythmias are to eliminate abnormal heart rhythms, improve quality of life, and prevent sudden cardiac death. If cardiac arrhythmias are present, the arrhythmia should be carefully analyzed and its clinical significance determined. Based on this analysis, first of all, the issue of the need to treat arrhythmia should be decided. Many rhythm disorders - sinus bradycardia, sinus arrhythmia, pacemaker migration, rare monotopic late extrasystoles, slow ectopic rhythms and some others do not require specific treatment. In some cases, for example, in case of rhythm disturbances in patients with thyrotoxicosis, myocarditis, acute coronary syndrome, etiotropic and pathogenetic therapy of the underlying disease can lead to relief of arrhythmia. Correction of arrhythmias in metabolic, electrolyte, sympathetic and parasympathetic disorders is carried out with the help of drugs that act on the factor that caused the arrhythmia - potassium, magnesium, anticholinergics, beta-blockers, etc. The most common heart rhythm disturbances include extrasystoles. They do not always require the appointment of active antiarrhythmic therapy. Thus, extrasystoles that occur without clinical symptoms, do not have pronounced subjective manifestations, do not threaten transformation into severe forms of arrhythmias, rare monotopic and late ventricular extrasystoles do not require antiarrhythmic therapy. It should also be taken into account that most modern antiarrhythmic drugs negatively affect the contractile function of the myocardium. This, first of all, must be remembered in patients with severe heart pathology and high class heart failure. Most patients with ventricular extrasystoles do not have organic heart pathology. In such cases, arrhythmia usually develops against the background of psycho-neurotic asthenia or an imbalance between sympathetic and parasympathetic innervation. Such patients need to be explained the benign nature of the arrhythmia. They are prescribed sedatives and tranquilizing drugs (valocordin, corvalol, rudotel, phenibut, atropine-like drugs, etc.). In addition, it is necessary to identify diseases and conditions against which extrasystole developed, and, if possible, eliminate provoking factors (hypokalemia, hypomagnesemia, drug intoxication, extracardiac diseases, etc.). Indications for prescribing antiarrhythmic therapy to patients with extrasystoles are: • frequent polytopic, group or early extrasystoles that threaten transition to more severe arrhythmias (ventricular tachycardia, atrial and ventricular fibrillation, etc.); • deterioration of hemodynamics, appearance of symptoms of heart failure. General principles for the treatment of arrhythmias, along with eliminating factors contributing to their occurrence before prescribing therapy, include: • establishing an accurate diagnosis before starting therapy and obtaining a baseline ECG to monitor the effectiveness of treatment; • monitoring during the treatment period not only the effectiveness of antiarrhythmic drugs, but also their side effects; • monitoring the concentrations of antiarrhythmic drugs in the blood, including the determination of non-protein-bound fractions. The latter, due to the narrow therapeutic index of most antiarrhythmic drugs, is necessary to prevent their serious complications. For the treatment of ventricular extrasystole there is a wide choice of antiarrhythmic drugs. From a theoretical point of view, almost all drugs of class I, II and III can be effective (according to the classification of E. Vaughan-Williams as modified by DC Harrison, 1985). However, a detailed analysis of drugs for the treatment of ventricular extrasystole made it possible to divide them into drugs of the first, second and third order (Doshitsyn V.L. et al., 1983, 1993; Smetnev A.S. et al., 1988). First-line drugs with an effectiveness of more than 70% include amiodarone, mexiletine, propafenone, Etatsizin and some others. One of the most active among them is amiodarone. It belongs to class III antiarrhythmic drugs and, like all other drugs in this class, is able to block potassium channels and prolong the action potential, slowing down repolarization. However, amiodarone also has additional mechanisms of action - blockade of fast sodium channels (mechanism of class I drugs) and slow calcium channels (mechanism of class IV drugs), sympatholytic action, including antagonism with b-adrenergic receptors. Thus, amiodarone has the properties of all four classes of antiarrhythmic drugs. Compared to most other antiarrhythmic drugs, its negative inotropic effect is negligible. In addition, it has an antianginal effect. Prospective randomized clinical trials conducted in the 1990s. last century, demonstrated a decrease in mortality in the post-infarction period in patients receiving amiodarone. The effectiveness of the drug for ventricular extrasystoles of various origins is 70-90% (Ardashev V.N., Steklov V.I., 1998; Mazur N.A., Abdalla A., 1995; Meshkov A.P., 1999), however use is limited by the high frequency of undesirable effects (bradycardia, prolongation of the QT interval with the possible occurrence of ventricular tachycardia of the “pirouette” type, symptoms of “iodism” with impaired thyroid function, hyperpigmentation, interstitial pneumonitis, etc.), especially with long-term use. Side effects develop in approximately 75% of patients receiving the drug, and their frequency increases after one year of treatment. The long half-life of amiodarone (25-110 days) also contributes to increased toxicity. Some of the side effects are potentially fatal. For example, toxic effects on the lungs may be irreversible and may be fatal in 10% of affected individuals. Severe arrhythmias that develop against the background of prolongation of the QT interval, such as ventricular fibrillation or paroxysmal ventricular tachycardia of the “pirouette” type, also pose a threat to life. If they occur, intravenous administration of lidocaine, mexityl, and magnesium preparations is necessary. Due to the risk of developing serious, including life-threatening, side effects, amiodarone is recommended to be prescribed for malignant forms of arrhythmia that are resistant to drugs of other classes [27]. The use of amiodarone is most important for the prevention of life-threatening ventricular arrhythmias. Arrhythmogenic action is the most common serious cardiac side effect of not only class III drugs, but also class I, which includes mexiletine (class IB), propafenone and etacizine (class I C). Class I A drugs (quinidine, procainamide, etc.), like amiodarone, increase the QT interval and can provoke torsade de pointes (TdP). Class I C drugs often induce monomorphic ventricular tachycardias. In addition, the CAST 1 and 2 studies showed that in patients with myocardial infarction and in patients with chronic circulatory failure, suppression of ventricular extrasystoles using class I drugs flecainide, encainide and moricizine leads to a significant increase in the risk of sudden and all-cause mortality ( Epstein AE, et al, 1991). A negative effect on the life prognosis of post-infarction patients was also noted when treated with drugs of class I A and I B (Teo KK, et al, 1993). However, it must be emphasized that in all studies that showed a negative effect of class I drugs on life prognosis, they were used for a long time and in large doses. A retrospective analysis of the CAST studies showed that the use of low doses of antiarrhythmic drugs may help reduce the risk of sudden death (Goldstein S., et al, 1995). In patients with non-coronary diseases and without a pronounced decrease in myocardial contractility, the use of class I drugs for the treatment of ventricular arrhythmias is not associated with an increased risk of mortality and is quite safe. In our country, among class I C drugs for the treatment of ventricular extrasystoles, Etatsizin and propafenone are widely used. Their effectiveness for this rhythm disorder is 54-90 and 52-70%, respectively (Mazur N.A., Abdalla A., 1995; Meshkov A.P., 1999). These drugs are comparable in tolerability. The incidence of side effects that necessitated discontinuation of treatment in clinical trials was 8.0-24.9% when using propafenone [Yakovleva N.V. et al., 1996; Hohnioser SH, 1999] and 4-31.8% – when using Etatsizin [Smetnev A.S. et al., 1990; Korneeva O.A., 1995). It should be noted that Etatsizin is an original domestic development, and in accordance with the criteria for the rational use of medicines, in case of equal effectiveness/safety with alternative foreign drugs, it should be given preference. Ethacizine is a diethylamine derivative of ethmosine. Its antiarrhythmic effect is associated with the blockade of sodium channels, which leads to a slowdown in the conduction of excitation in all parts of the conduction system of the heart. Ethacizine causes a negative inotropic effect, which, however, does not contribute to the appearance of clinical signs of heart failure. It also has a local anesthetic and antispasmodic effect. Etatsizin has a wide spectrum of antiarrhythmic action. It is used not only for ventricular, but also for atrial extrasystoles and tachyarrhythmias, paroxysms of atrial fibrillation, early ventricular repolarization syndrome. The effectiveness of the drug has been shown in clinical studies and with many years of use in widespread medical practice. The antiarrhythmic effect when taken orally usually appears on the first or second day. Treatment usually begins with three doses of one tablet (150 mg/day) under ECG monitoring; after achieving a stable clinical effect (usually after several days of therapy), a gradual reduction in the dose to the minimally effective (maintenance) dose is possible. The duration of treatment with Etatsizin is selected individually; the drug does not accumulate in the organs and tissues of the body, which allows, if necessary, to recommend long-term continuous courses of therapy. Etatsizin is quite well tolerated, including during pregnancy. In a study that included 14 pregnant women who were prescribed Etatsizin in the second half of pregnancy for polymorphic ventricular extrasystole for 3-12 weeks, its safety for the mother and fetus was shown (Kryuchkova O.N. et al.). Like other antiarrhythmic drugs, Etatsizin can cause cardiac side effects: decreased myocardial contractility, worsening coronary circulation, arrhythmogenic effect, ECG changes, including prolongation of the PQ interval, expansion of the P wave and the QRS complex. Unlike antiarrhythmic drugs of other classes, the extracardiac side effects of Etatsizin do not lead to serious dysfunction of other organs and systems and are not irreversible. Phenomena such as tinnitus, dizziness, numbness of the lips and tip of the tongue, sensation of heat, diplopia and nausea only cause slight subjective concern in particularly sensitive patients in the first days of taking the drug. To prevent serious complications, Etatsizin should be used in the minimum effective dose, and treatment should be carried out only under the supervision of a physician with careful monitoring of effectiveness and side effects. The risk of arrhythmogenic effects of Etatsizin increases when used simultaneously with other quinidine drugs and MAO inhibitors, and therefore such combinations should be avoided. On the contrary, Etatsizin combines well with amiodarone and beta-blockers; these combinations make it possible to halve the effective dose of both antiarrhythmic drugs, which improves tolerability and reduces the risk of side effects. The combined administration of Etatsizin with these drugs allows many patients to reduce the doses of the components of the combination and, consequently, the risk of side effects while maintaining or increasing the effectiveness of antiarrhythmic therapy. Thus, on the modern pharmaceutical market there is a fairly large number of effective antiarrhythmic drugs for the treatment of ventricular extrasystoles, but the approach to therapy must be strictly individual. Many patients can do without specific treatment. If it is necessary to prescribe an antiarrhythmic drug, the balance between its effectiveness and safety should be carefully weighed and treatment should be carried out under strict medical supervision.
Symptoms of arrhythmic syndrome
The clinical picture of extrasystole mainly consists of subjective sensations and is characterized by such symptoms as:
- a feeling of interruptions in the work of the heart, its fading;
- feeling of heart hitting chest;
- anxiety, lack of air;
- weakness, decreased performance;
- pallor, sweating, feeling hot.
The main danger of extrasystoles lies in their ability to develop into more serious rhythm disturbances, such as paroxysmal tachycardia and atrial fibrillation.