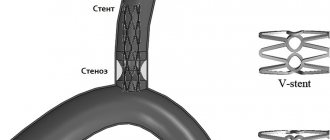
Every fourth stroke develops in the posterior parts of the brain in the area of responsibility of the vertebral arteries. Atherosclerosis and narrowing of the vertebral artery
can occur in any part of it and can cause ischemic stroke. Unlike narrowing of the carotid arteries, the role of which in the development of stroke has been known for a long time and methods for their treatment have been developed, the pathology of the vertebral arteries has not yet been sufficiently studied. However, modern technologies for diagnostic testing and endovascular treatment methods have opened up new opportunities for intervention in this disease.
Vertebral artery syndrome is a condition associated with obstruction of the patency manifested by symptoms of cerebrovascular insufficiency in the posterior part of the brain.
The causes of impaired patency can be very different, so the main task in the management of patients is an accurate diagnosis, so that as soon as the identification of the exact cause will allow it to be eliminated and the symptoms that are painful for patients to be removed. Every year the disease becomes younger, which is associated with an increase in the number of young people who sit for long periods at computers and have a sedentary lifestyle.
Timely diagnosis guarantees a favorable result of treatment of vertebral artery syndrome in our clinic.
Causes of vertebral artery syndrome
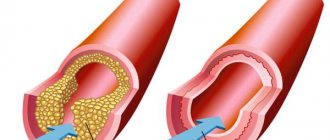
The most common cause of vertebral artery circulatory disorders is atherosclerotic plaque. Less common are stratification (dissection) of the artery, compression of it in the neck or at the entrance to the skull, and inflammatory diseases (vasculitis). It is quite difficult to accurately determine the likelihood of developing a stroke with such a localized lesion. According to anatomical studies, damage to the vertebral arteries during death from ischemic stroke was observed in 12% of cases.
Damage to the intracerebral parts of the vertebrobasilar system more often leads to ischemic strokes than narrowing of the artery in the neck. The risk of developing ischemic events with such lesions is about 7% per year. Symptoms of vertebral artery syndrome are being diagnosed more and more often. Many factors influence the development of the syndrome. It usually represents a combination of cerebrovascular arteriosclerosis and cervical spondylosis (degenerative changes in intervertebral disc tissue) as the main clinicopathological components.
GBOU "NIKIO im. L.I. Sverzhevsky" of the Moscow Department of Health
Developer institution:
State budgetary healthcare institution "Scientific and Practical Center of Otorhinolaryngology" of the Moscow Department of Health and the Department of Otorhinolaryngology of the Medical Faculty of the State Educational Institution of Higher Professional Education "Russian State Medical University".
Compiled by:
Doctor of Medical Sciences prof. A.I. Kryukov ; Doctor of Medical Sciences, Prof. V.T.Palchun ; Doctor of Medical Sciences prof. N.L. Kunelskaya ; Doctor of Medical Sciences M.V. Tardov ; Ph.D. HER. Zagorskaya; Ph.D. E.S.Yanyushkina, Ph.D. E.V. Baibakova; Ph.D. M.A. Chugunova; Ph.D. Yu.V. Levin ; Ph.D. A.L. Guseva; Z.O.Zaoeva.
Reviewers:
Doctor of Medical Sciences, Professor I.D. Stulindoctor of Medical Sciences, Professor S.V. Morozova
Purpose:
The methodological recommendations describe a diagnostic algorithm for central dysfunction of the vestibular analyzer, a pathology manifested by dizziness - one of the most common complaints during outpatient visits. The methodological recommendations are intended for otorhinolaryngologists, neurologists, otoneurologists and general practitioners.
This document is the property of the Moscow Department of Health and may not be reproduced without appropriate permission.
Introduction
When examining a patient with complaints of dizziness, it is first necessary to differentiate between peripheral and central vestibular syndromes.
The role of nystagmus in topical diagnosis is limited, but some of its types may correspond to certain local brain damage. It should also be noted that there is no nosological specificity of various types of nystagmus.
It is generally accepted that horizontal nystagmus most often corresponds to damage to the peripheral part of the vestibular analyzer. A pronounced rotatory component of nystagmus indicates involvement of central structures in the process.
Vertical nystagmus with a downward fast phase direction may correspond to damage to the cervicomedullary region and inferior cerebellar peduncles, and with an upward fast phase direction it can be recorded with damage to the anterior parts of the vermis or superior cerebellar peduncles (Arnold-Chiari malformation type I). Also associated with pathological processes in the area of the craniovertebral junction is periodic alternating nystagmus - a cyclic disorder in which horizontal jerky nystagmus spontaneously acquires the opposite direction with a periodicity of 1 to 3 minutes.
Retraction nystagmus, characterized by irregular twitching of the eyes into the orbit, is associated with lesions of the midbrain tegmentum or quadrigeminal. This type of nystagmus can be combined with pulsating, as well as convergent nystagmus, which is characterized by slow divergent movements of the eyeballs, interrupted by fast convergent impulses.
Lesions of the caudal parts of the pons sometimes cause floating movements of the eyeballs - rapid downward movements of the eyeballs followed by a return to their original position. Nystagmoid twitching of one eye occurs with severe damage to the midbrain and lower parts of the pons.
Sawtooth nystagmus develops with lesions of the caudal parts of the brain stem and consists of rapid unfriendly eye movements, in which one eyeball turns upward and inward, and the other downward and outward.
A rare, unusual movement disorder of the eyeballs, called opsoclonus, consists of a bout of sequential saccades that are associated with damage to the cerebellum, and less commonly, the brainstem or thalamus. In cases where such saccades occur in the horizontal plane, the terms “ocular myoclonus” or “dancing eyes syndrome” are used.
If a peripheral syndrome is diagnosed, it may be necessary, in addition to audiological and vestibulological studies, to conduct: multislice computed tomography (MSCT) of the temporal bone to assess the pathology of the labyrinth; magnetic resonance imaging (MRI) to verify the formation of the cerebellopontine angle and vaso-neural conflict.
If a violation of the functions of balance and coordination of the central type is diagnosed, then a neurological examination should determine the areas of damage: the vestibular nuclei of the brainstem, the upper brainstem structures, the cerebellum and its pathways, the frontal or parietal cortex. Confirmation of the topical diagnosis is provided by MRI of the brain, and to clarify the etiological factors, radiography of the cervical spine and cranio-vertebral junction, as well as ultrasound examination of blood flow in the main arteries of the neck and head are used.
Anatomy and physiology of the vertebrobasilar system
The paired vertebral artery (VA), arising from both sides of the subclavian artery, is its first and largest branch (Fig. 1). According to A.V. Pokrovsky, the following segments of PA are distinguished:
Figure 1. Trajectory of the vertebral artery.
1) The first segment (V1) from the mouth to the entry into the canal of the transverse processes of the cervical vertebrae. As a rule, the artery enters the transverse process of the sixth or fifth cervical vertebra.
2) The second segment (V2) – before the exit from the foramen of the transverse process of the second cervical vertebra. In the absence of vertebral pathology, the course of the vessel in this segment is relatively straightforward: each vertebral artery is held almost exactly in the center of the opening of the transverse process with the help of thin connective tissue trabeculae and remains intact during any movement in the cervical joints within the limits of physiological mobility.
3) The third segment (V3) – before entering the cranial cavity. After leaving the opening of the transverse process of the axis, the vertebral artery deviates outward and enters the opening of the transverse process of the atlas. Further in the horizontal plane, heading dorsally, it bends around the lateral mass of the atlas, turns up and forward and, piercing the atlanto-occipital membrane, penetrates into the cranial cavity through the foramen magnum. In this segment, the artery makes four bends in different planes, including two at right angles, which, in accordance with the laws of hydrodynamics and similar to the siphon of the internal carotid artery, ensures smoothing of the pulse wave and uniformity of blood flow.
4) The fourth segment (V4) - to the confluence of the right and left vertebral arteries on the lower surface of the medulla oblongata or the bridge into the basilar artery (BA).
At the level of the first cervical vertebra, the VA is surrounded by the atlanto-occipital sinus, in which it is “suspended” by fibrous cords. The walls of the sinus are unyielding; As a result, the pulsation of the artery in the sinus cavity stimulates the outflow of venous blood, being an important regulatory mechanism of cerebral hemocirculation.
The radicular arteries depart extracranially from the VA, supplying the lower cervical (C4-C8) and upper thoracic (Th1-Th3) segments. The four upper cervical segments (C1-C4) are supplied by the anterior spinal artery, which is formed by the fusion of the anterior spinal arteries, branches of the vertebral arteries. The PA and anterior spinal arteries on the anterior surface of the medulla oblongata form an anastomotic rhombus.
Intracranially, the vertebral and basilar arteries give off small branches that supply blood to the medulla oblongata and the pons, respectively.
The largest branch of the VA is the posterior inferior cerebellar artery, which provides vascularization to the inferior surface of the cerebellum. It also gives branches to the villous plexus of the fourth ventricle, the ventrolateral surface of the medulla oblongata, and to the roots of the X, IX, VIII and VII cranial nerves. The same artery is the source of the posterior spinal artery.
From the caudal segment of the basilar artery arises the anterior inferior cerebellar artery, which supplies the inner ear (Fig. 2), part of the inferior peduncles and the ventral part of the cerebellum.
| 1 – main artery; 2 – anterior inferior cerebellar artery; 3 – anterior vestibular artery; 4 – artery of the labyrinth; 5 – common cochlear artery; 6 – main cochlear artery; 7 – posterior vestibular artery |
Figure 2. Blood supply to the inner ear.
The oral portion of the basilar artery gives rise to the superior cerebellar artery, which carries blood to the convexital surface of the cerebellar hemispheres.
The main artery in its normal development is divided into the right and left posterior cerebral arteries, the branching area of which extends to the lower surface of the temporal and occipital lobes to the parieto-occipital sulcus. The area of the artery's blood supply includes the hypothalamus, cerebral peduncles, posterior parts of the corpus callosum, hippocampus, ependyma of the lateral ventricles, choroid plexuses and, most importantly, the visual cortex.
Intravasal factors influencing
on the vertebrobasilar blood flow
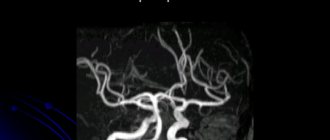
In addition to regulatory factors, the features of cerebral vascular architecture have a huge impact on blood flow in the vertebrobasilar system. Analysis of the structure of the arterial system of the brain showed that its typical structure (Fig. 3) occurs in no more than 50% of cases. It is important to emphasize that the variability in the development of the arteries of the posterior basin significantly exceeds the variety in the structure of the branches of the carotid system: thus, posterior trifurcation is recorded with a frequency of up to 25% of cases, and variants of the structure without fusion of the vertebral arteries are also found. The diameters of the vertebral arteries are often different - in 25-30% of cases the right vertebral artery predominates, and the left one can predominate with the same frequency.
| 1 – intracranial part of the internal carotid artery; 2 – middle cerebral artery; 3 – anterior cerebral artery; 4 – anterior communicating artery; 5 – posterior communicating artery; 6 – posterior cerebral artery; 7 – main artery; 8 – superior cerebellar artery; 9 – anterior inferior cerebellar artery; 10 – posterior inferior cerebellar artery; 11 – vertebral artery. |
Figure 3. Structure of the large arterial circle of the brain.
The variant of the origin of the vertebral artery from the subclavian artery is important. There are frequent cases where the mouth of the vertebral artery is located not on the upper, but on the posterior and even lower wall of the subclavian artery, which leads to deformation of the initial segment of the VA with a high probability of the formation of a local hemodynamic difference, limiting the blood flow in the vessel.
Separately, mention should be made of such important intracranial anastomoses as the posterior communicating arteries: the absence of one posterior communicating artery is recorded in 6-10% of cases, and the absence of both posterior communicating arteries is not uncommon - complete separation of the posterior sections of the circle of Willis.
Intravascular factors affecting the vascularization of the brain include various types of stenotic processes in the vertebral and basilar arteries: atherosclerotic, inflammatory, fibromuscular hyperplasia.
Extravasal effects on vertebrobasilar blood flow
Persistent or transient compression of the vertebral artery in the canal of the transverse processes or, less frequently, in the intermuscular spaces can cause a decrease in blood supply to the vertebrobasilar region, as well as a narrowing of the lumen of the artery due to a plaque or thrombus. The clinical picture of suffering develops depending on the development of collaterals and the structure of the arterial circle at the base of the brain. In the latest version of the International Classification of Diseases, 10th revision, such a symptom complex is defined as “vertebrobasilar arterial system syndrome” within the framework of “transient transient cerebral ischemic attacks (attacks) and related syndromes” (G 45.0).
According to the areas of vascularization of the vertebral basin and the basilar artery, the symptoms associated with impaired blood flow in the VBS are diverse and include cochleovestibular disorders, visual and oculomotor disorders; violations of statics and coordination of movements. It is this symptom complex that occurs in more than 80% of patients with circulatory failure in the posterior circulatory system.
Visual and oculomotor disorders are very common phenomena and are manifested by blurred visual fields, blurred vision of objects, photopsia or scintillating scotomas and loss of visual fields. Oculomotor disorders are expressed by transient diplopia (in different directions of gaze) with mild paresis of the eye muscles and convergence insufficiency.
Static and dynamic ataxia is one of the most common symptoms, manifested by complaints of instability and staggering when walking. Coordination of movements may also be affected.
Cochleovestibular disorders manifest themselves in the form of acutely developing systemic or non-systemic dizziness, sometimes with spontaneous nystagmus, dizziness is often accompanied by nausea and vomiting. There is tinnitus of various timbres: from high (squeaking and whistling) to low tones (surf noise, buzzing). In this case, dizziness as a monosymptom can be regarded as a reliable sign of dyscirculation in the VBS only in combination with other signs of circulatory disorders in it in patients with a relatively persistent otoneurological symptom complex.
Less known, although not uncommon, are optic-vestibular disorders. These include symptoms of “shading shadows” and “convergent vertigo,” when sufferers experience dizziness or unsteadiness when seeing flashes of light and shadow or when looking down. Various types of visual agnosia with impaired optical-spatial perception can be identified, as well as elements of sensory and amnestic aphasia as a result of ischemia in the distal cortical branches of the posterior cerebral artery.
Characteristic symptoms are attacks of sudden falling and immobility without loss of consciousness (drop attacks) and with loss of consciousness (Unterharnsteidt's syndrome), usually occurring with sudden turns or throwing back the head. Manifestations of diencephalic disorders include severe general weakness, irresistible drowsiness, disturbances in the rhythm of sleep and wakefulness, as well as various autonomic-visceral disorders, sudden increases in blood pressure, heart rhythm disturbances, etc.
The basis for the expanded diagnosis of the syndrome of transient circulatory disorders in VBS may be the unjustified inclusion of symptoms related to the initial stages of the well-studied “vertebrogenic vertebral artery syndrome”. Its initial or angiodystonic stage is defined as a syndrome of vertebrogenically caused irritation of the perivascular sympathetic plexus of the vertebral artery with typical pain (vegetalgic) symptoms. These peculiar cervico-occipital pains, spreading to the parietal, temporal regions and orbit, are often described as “removing the helmet.” The predominant pain component is felt as a burning sensation, paresthesia, a feeling of squeezing or fullness in the eyes, ears, and throat. The described phenomena intensify with a sharp change in the tilt of the head or in an uncomfortable position, especially after sleep. Visual and cochleovestibular symptoms are also peculiar and usually arise or worsen not as isolated symptoms, but during attacks of characteristic headache.
Features of the course of the vertebral artery in the intermuscular spaces and in the canal of the transverse processes determine the options for possible extravasal influences on it. The effect of muscles on PA is associated with their segmental tonic tension, usually as part of myofascial syndromes associated with osteochondrosis of the cervical spine.
Before entering the canal of the transverse processes, the vertebral artery may be compressed by the edge of the anterior scalene muscle or the longus colli muscle. A more common option is compression of the VA before entering the cranial cavity by the inferior oblique muscle of the head, which, with a sharp turn and tilt of the head, stretches and can impinge on the greater occipital nerve, branches of the second cervical nerve and the VA itself.
More complex and ambiguous effects on the VA can be exerted by the structures that make up the canal of the transverse processes. Arthrosis of the uncovertebral joints can lead to direct compression with changes in the course of the entire intraosseous segment of the vertebral artery. With ultrasound angioscanning or radiopaque imaging methods, the artery takes on a “tortuous” appearance, bending around the deformed joints.
Excessive mobility (instability) of the motor segments of the cervical spine creates conditions for mechanical effects on the VA: compression of the artery or irritation of the periarterial sympathetic plexus.
Complex effect on the vestibular analyzer
As a rule, individual manifestations of abnormalities of the cervical spine or the vascular system of the brain are not so significant as to cause dizziness or impair coordination. The clinical situation may vary due to a combination of several abnormal and pathological factors.
For example, a combination of hypoplasia of one of the vertebral arteries and incompetence of the contralateral posterior communicating artery (Fig. 4) may not lead to coordination disorders. However, in the case of the development of instability or muscular-tonic phenomena against the background of a violation of the statics of the cervical spine - phenomena that can cause a mechanical effect on the hemodynamically predominant VA - cerebral syndrome may debut with dizziness.
| 1 – right posterior communicating artery; 2 – absence of the left posterior communicating artery; 3 – hypoplastic right vertebral artery; 4 – hemodynamically predominant vertebral artery |
Figure 4. Combination of vertebral artery hypoplasia and contralateral posterior communicating artery incompetence.
A similar situation may arise if the patient has an Arnold-Chiari malformation. This pathology may not manifest itself clinically until a violation of the motor stereotype of the cervical spine is formed or arterial hypertension develops, accompanied by microcirculatory disorders, especially at the level of the venous segment. These processes can ultimately lead to compression of the VA or the cerebellar tonsils themselves, and to liquorodynamic disorders.
Thus, identifying positional (vertebrogenic) nystagmus requires expanded examination: ultrasound examination of blood flow in the VBS and radiation examination of the cervical spine.
Radiation diagnostics of spinal pathology.
Survey radiographs of the spine, in accordance with the recommendations, are necessarily performed in two projections, which makes it possible to study the structure of the vertebral body, the height of the intervertebral spaces, and the condition of the intervertebral and hamate joints. Spot-on images of the atlantoaxial joint demonstrate the features of Cruvelier's joint. If an anomaly of the craniovertebral joint is suspected, a special imaging technique is used to calculate the angles between the components of the skull base and the axis of the odontoid process.
A large group of radiological symptoms of osteochondrosis is associated with impaired static function of the spine. On radiographs, this is manifested by a change in the axis of the spine - straightening of the cervical and lumbar lordosis or increased thoracic kyphosis. When the C5-C7 discs are affected, complete straightening of the cervical lordosis is usually determined; changes in the C3-C5 discs cause only partial straightening of the lordosis. Kyphosis may form. In this case, the distance between the processes at the level of kyphosis increases.
| Figure 5. Spondylolisthesis. |
Objective data on the mobility of the cervical spine are provided by functional x-ray studies with flexion and extension, accompanied by the effect of strengthening or weakening hidden displacements of the vertebrae. Radiographs with functional tests may reveal displacement of the vertebrae (Fig. 5) forward and backward. The simultaneous displacement of two or more vertebrae in the same direction is referred to as scalene displacement. These changes indicate a loss of the fixation ability of the disc and the initial manifestations of osteochondrosis.
Instability of motion segments in the cervical spine is common, which is often associated with posterior extensor subluxation according to Kovacs. A characteristic feature of subluxation according to Kovacs is the presence of displacement of the lower edge of the articular process during extension, which is normalized in a neutral position or during flexion. Such a subluxation appears during extension and indicates pathological mobility of the spinal motion segment (SMS) and the possibility of a direct vertebrogenic effect on the VA. Another symptom of pathological mobility is the bevel of the anterior-superior angle of the vertebra in the lateral projection.
The indicator of instability of the SDS is determined for all segments of the cervical spine. Particularly clinically significant is pendulum-shaped polysegmental instability at the mid-cervical level (the level of passage of the VA in the canals of the transverse processes) with a high degree of instability - the instability index is above 3 mm.
The most important from a clinical point of view and studied in detail in relation to X-ray diagnostics are the following forms of degenerative-dystrophic lesions of the spine: osteochondrosis, spondylosis deformans, fixing ligamentosis (Forestier disease), disc herniation (posterior cartilaginous node), Schmorl's hernia, spondyloarthrosis.
It is important to identify, using radiography, anomalies of the craniovertebral junction - congenital or acquired disorders of the structure of the base of the skull or the upper cervical spine. The abnormal structure of bone structures leads to a narrowing of the bone spaces containing the lower parts of the brain stem and the cervical spinal cord, which can lead to hemo- and liquorodynamic disorders, as well as compression of the brain elements themselves, manifested by cerebellar, vestibular and spinal disorders. A clinical picture of damage to the caudal group of cranial nerves may also be observed. The most common are:
- assimilation of the atlas (fusion of the first cervical vertebra with the skull) in the area of the foramen magnum;
- platybasia – flattening of the base of the skull;
- basilar impression – displacement of the odontoid process upward into the area of the foramen magnum;
- Klippel-Feil anomaly – fusion of cervical vertebrae;
- atlantoaxial dislocation – displacement of the atlas anteriorly in relation to the axis (second cervical vertebra), often observed in the absence or underdevelopment of a tooth, its non-fusion with the vertebral body;
- Kimerli's anomaly - the presence of an additional bone arch-semi-ring, forming a bone canal instead of the groove of the vertebral artery above the arch of the first cervical vertebra (Fig. 6);
| Figure 6. Kimerli anomaly. 1 – vertebral artery, 2 – bone bridge |
- Arnold-Chiari malformation type I - descent of the cerebellar tonsils into the foramen magnum (Fig. 7).
| Figure 7 . Arnold-Chiari malformation. 1 – cerebellum; 2 – cerebellar amygdala; 3 – atlas; 4 – spinal cord. |
If there are clinical signs of pathology of the cervical roots (shooting pain, loss of tendon reflexes, sensitivity zones), an MSCT or MRI of the cervical spine is necessary. It is these techniques that make it possible to reliably diagnose Arnold-Chiari malformation.
Tomography data is used to determine the presence of protrusions and herniations of intervertebral discs and their effect on the posterior longitudinal ligament and spinal nerve roots. Compression of the spinal cord or anterior spinal artery causes not only segmental sensitivity and movement disorders, but also conduction sensitivity disorders, and in severe cases, pyramidal insufficiency and dysfunction of the pelvic organs, which corresponds to the concept of cervical level myelopathy.
Ultrasound examination of cerebral blood flow.
The primary assessment of the condition of the neck arteries is carried out using a linear sensor of an ultrasound scanner: after excluding developmental anomalies of the brachiocephalic arteries, the parameters of flow velocity and resistance are recorded. Then a Doppler study of blood flow in the cerebral arteries is performed using transtemporal and suboccipital access using standard methods. The middle (MCA), anterior (ACA), posterior (PCA), vertebral (VA) arteries on both sides and the basilar artery (BA) are located. Using compression tests, the functions of the connecting arteries are assessed. Next, blood flow rates in the cerebral venous trunks are assessed: veins of Rosenthal, Galen, middle cerebral veins; straight and cavernous sinuses.
When assessing the LSC in the located arteries, the symmetry (equality) of the LSC in paired vessels is taken into account, as well as the compliance of the LSC with age standards and the observance of the proportions between the LSC in the extra- and intracranial arteries.
The next step is to study the PA in the third segment after repeating the head rotation three times at the maximum angle from side to side (pendulum test - MP). In this case, a Dopplerogram is recorded corresponding to the third cardiac cycle in a standard position after completion of movements. Turning the head in a flexion position makes it possible to evaluate the effect on PA at the upper cervical level, in a neutral position - in the interscalene space, and tilting the head back and forth - at the mid-cervical level. Before Doppler tests, blood pressure is measured with an electronic tonometer.
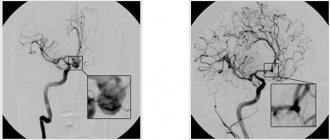
Ultrasound angioscanning plays an important role in studying the trajectory and intraluminal contents of arterial arteries, which makes it possible to detect stenosis of the lumen (atherosclerotic plaque, thrombus, fibromuscular dysplasia), pathological tortuosity, and dissection of the arterial wall. Identification of the local hemodynamic difference in flow velocity in the artery is of fundamental importance.
Predisposing factors for dissection include neck injuries and infections, however, apparently, local disruption of the properties of the vessel wall is also important in the development of this pathology. When clarifying the circumstances of the occurrence of dizziness, information may be important not only about the effects on the cervical-occipital region (pulsation techniques of manual therapy), but also about the patient’s long stay in a position with a fixed neck, as in dental or ophthalmological treatments.
Dopplerographic dissection of the wall of the cervical artery is manifested by a pattern of stenotic blood flow in the area of interest, which is caused by a narrowing of the lumen of the artery at the level of pathology: an increase in BFV, an expansion of the spectrum due to high frequencies, a difference in peripheral resistance parameters between the pre- and poststenotic segments. Sometimes a “double” spectrum can be insonated due to the superposition of the sound of the flow in the main channel and in the hematoma channel. With angioscanning in the dissection area, it is possible to visualize thickening of the arterial wall with a wide anechoic layer and narrowing of the arterial lumen in the absence of intraluminal formations. If the course of the process is unfavorable, thrombosis may develop in the narrowing zone.
Angioscanning also allows you to evaluate the diameter and shape of the lumen of the internal jugular veins, the speed of blood flow in the jugular and vertebral veins. Exceeding standard values may indicate difficulty in venous outflow from the cranial cavity, which often correlates with the presence of labyrinthine hydrops.
Neuroimaging techniques
MRI or MSCT of the head is indicated for the patient when a central type of lesion of the vestibular analyzer is detected. MRI in standard magnetic sequences (T1, T2, FLAER) allows you to identify infarct and post-hemorrhagic lesions in the brain, signs of leukoaraiosis and hydrocephalus, space-occupying formations, incl. neoplasms of the cerebellopontine angle.
Magnetic resonance angiography (MRA) in the first (arterial) phase allows to identify abnormalities in the structure of the arteries (aneurysms, arteriovenous malformations), as well as significant stenoses of the intracranial arteries. In the second (venous) phase, anomalies in the structure of the veins and sinuses of the dura mater can be assessed.
MSCT of brain vessels is a study that is more sensitive than MRA and is carried out with a bolus injection of intravenous contrast. This technique also allows you to evaluate separately the arteries and veins of the brain.
In some cases, three-dimensional reconstruction of the arterial and venous beds, which is possible with modern tomographic devices, brings great diagnostic benefit.
To identify the neurovascular conflict of the VIII cranial nerve and the arteries of the SMV, special MRI programs (usually on high-tensile installations - 3T) 3D-SPGR and 3D-FIESTA are used.
List of abbreviations
- PCA – posterior cerebral artery
- MP – pendulum test
- MRA – magnetic resonance angiography;
- MRI – magnetic resonance imaging
- MSCT – multislice computed tomography
- OA – main artery
- VA – vertebral artery
- SMS – vertebral motion segment
- ACA – anterior cerebral artery
- MCA – middle cerebral artery
Forecast
With atherosclerosis of the vertebral artery, it is quite difficult to give a prognosis for the life and health of the patient. With large narrowings, blood flow is compensated by the second vertebral artery; in addition, there is collateral blood flow. There have not yet been large studies assessing the risk of stroke with damage to the vertebral arteries. However, the fact remains that strokes in the vertebrobasilar system account for at least 25% of all strokes and are much more severe than strokes associated with the carotid artery. Therefore, the identification of significant narrowing of the vertebral artery should be a reason to eliminate this risky condition.
Without identifying and eliminating the causes of the development of vertebral artery syndrome, the prognosis for recovery is unfavorable. Most often, the patient's condition gradually worsens, which negatively affects the quality of life.
The most difficult thing is to identify the exact cause. Knowing the cause will allow it to be eliminated surgically or endovascularly and relieve the patient from painful symptoms.
Symptoms
When a person has a non-linear course of the vertebral arteries, symptoms can only indicate that blood circulation in the brain is impaired. Only a complete examination will help make the correct diagnosis.
Stage of functional impairment (dystonic)
The main symptoms that show that the patient has a non-straightforward course of the vertebral arteries:
- the back of the head hurts, the pain is bursting and aching;
- there is a feeling of pressure in the back of the head;
- neck pain regularly;
- dizzy when getting out of bed;
- blood pressure rises, it is not possible to lower it with medications;
- there is no strength to do everyday work, you constantly want to sleep, it’s hard to wake up in the morning;
- nausea bothers me, nosebleeds appear, although there are no problems with the gastrointestinal tract;
- weakness in the arms and legs, even if the person has not played sports;
- Vision and hearing deteriorate, tinnitus appears, and “spots” flash before the eyes.
Ischemic stage
It is advisable to consult a doctor as soon as the above symptoms occur. He will refer you for examination and prescribe a course of treatment. If symptoms are ignored, irreversible changes may occur. With severe deformities, a spinal stroke develops. Its main symptoms:
- gait becomes unsteady;
- facial expressions change;
- the tongue deviates to one side;
- there may be paralysis of the legs or arms on the left or right side;
- the patient cannot speak.
In this case, we are talking about life and death, the patient must be urgently taken to a neurological or special vascular hospital.