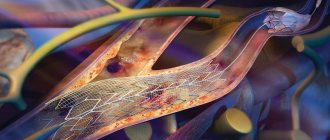
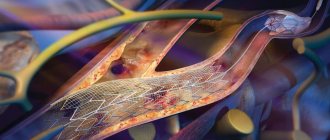
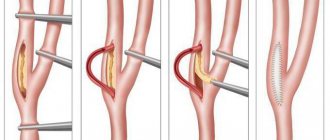
Endovascular surgery comes to the rescue. A special catheter with a balloon at the end is inserted into the narrowed area through a puncture of the vessel using X-ray control. In the area of stenosis, the balloon is inflated, eliminating the narrowing. This is called balloon angioplasty. To maintain the lumen, a fairly rigid mesh structure is installed in the artery - a stent, which plays the role of an internal frame. Since it is a foreign body, there is a possibility that it could cause an unwanted response from the body - thrombosis, especially if the stent is made of metal. Therefore, specialists have developed polymer-coated devices. They secrete medicinal substances designed to reduce this problem. As a rule, with their help, stenting of heart vessels is performed. Such stents have become a new word in the technologies of endovascular interventions and have brought this area of medicine to a new, higher and better level.
Stenting is most often performed on the following vessels:
- coronary arteries - their damage by atherosclerotic plaques is observed in coronary heart disease; Stenting in this case is necessary if a person develops angina or a high risk of developing myocardial infarction;
- carotid arteries - restoration of the lumen of the carotid arteries is indicated in case of cerebrovascular accident; stenting is the least traumatic method of treating carotid artery stenosis in the world;
- the vessels of the lower extremities or peripheral arteries are responsible for delivering blood to the legs; the main sign of impaired blood flow due to the formation of atherosclerotic plaques is pain that appears in the extremities - in the feet, buttocks, thighs, knees, legs while walking;
- restenosis of the artery after balloon angioplasty or in combination with it - during balloon angioplasty, re-narrowing of the artery sometimes develops, in which case stenting is necessary.
Briefly about the treatment method
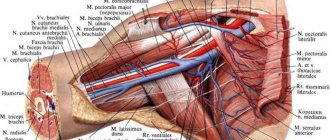
Endovascular surgery for narrowing of the vertebral artery, which allows you to restore the patency of the vessel and prevent the development of stroke in the vertebrobasilar region.
The carotid and vertebral arteries pass through the neck, supplying blood to the brain.
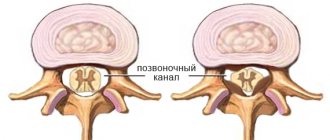
Vertebral (vertebral) arteries are located in the neck and are mainly contained in the bony canals of the cervical spine. The vertebral artery stenting procedure is a minimally invasive method that provides an alternative to surgery. With stenting, a self-expanding mesh tube is placed into the artery at the site of the narrowing. When placed in a vessel, the external force of the stent reduces or completely eliminates the narrowing in the vessel. This method can be applied to vessel narrowing both in the neck and inside the skull. A stent is a tubular metal mesh whose task is to maintain vascular patency. They have been actively used since the 90s. Depending on what the stents are made of, they come in two types: balloon-expandable and self-expanding. The spreadable ones are a mesh, made of stainless steel or other metal alloys (cobalt and chromium) that resist rust. Modern meshes have a complex design and can adapt to the shape of a blood vessel and are distributed evenly and accurately inside it. Self-expanding stents are made from thin wires made of steel or nitinol (an alloy of nickel and titanium) and are characterized by their shape memory. They are less often used for stenting the vertebral artery, since during implantation they are shortened by up to 20% and cannot be held firmly in a certain position. Carotid and vertebral stents remain in place and are not detected by metal detectors. Carotid and vertebral artery stenting is much less invasive than surgery. Patients usually have a shorter recovery time. For the vertebral and subclavian arteries, treatment with angioplasty alone or angioplasty with stenting may be appropriate first-line therapy.
Indications and contraindications for the treatment method
The goal of endovascular stenting surgery is to improve or restore blood flow and oxygen. Some reasons why a doctor may suggest stenting:
- The patient has high risks with open surgery.
- The patient cannot undergo general anesthesia.
- The patient has a new narrowing in the artery from previous surgery (“restenosis”).
Indications for stenting: Arteries can become narrowed (stenotic) or completely blocked due to atherosclerosis. Atherosclerosis is a disease in which fatty deposits called plaques collect inside blood vessels. As atherosclerosis develops, there is a gradual narrowing of the vessel and a decrease in blood flow to the brain. This can lead to stroke or temporary ischemic attacks. By restoring or increasing blood flow through narrowed arteries, the risk of a potentially life-threatening stroke can be reduced or prevented. Pseudoaneurysm: forms a secondary injury to the vessel wall, leading to periarterial hematoma. Arteriovenous fistulas associated with the vertebral arteries are a rare occurrence. Like pseudoaneurysms, these lesions most often occur secondary to blunt or penetrating neck trauma. Iatrogenic lesions are caused by arterial puncture with concomitant damage to the adjacent vein. Symptoms of vertebrobasilar insufficiency. Pathological tortuosity of the artery.
Contraindications Although stenting may be a better option than surgery for many patients, it is not suitable for everyone. The procedure is not performed if the diameter of the artery is less than 3 mm; the patient has severe renal and respiratory failure; the patient has vascular disease that does not allow endovascular intervention; with severe tortuosity of the artery; recent stroke or intracranial hemorrhage.
Introduction
In recent years, carotid artery stenting has partially replaced carotid endarterectomy in many patients [1–5].
However, there are no data from prospective randomized trials comparing two-stage carotid artery stenting and coronary artery bypass grafting (CABG) with a combined surgical approach [6–10]. Long-term results of techniques including brachiocephalic artery (BCA) stenting in addition to myocardial revascularization have also not been published [11, 12]. After carotid artery stenting, there is a need for aggressive antiplatelet therapy, including clopidogrel for at least 1 month and acetylsalicylic acid. Restoration of blood flow through the internal carotid artery (ICA) can provoke hemodynamic changes such as bradycardia and hypotension. These facts make BCA stenting unfavorable for the treatment of patients with severe coronary artery disease (CAD) [1, 5, 9, 13, 14].
The CREST report (2011) showed risk factors for perioperative cardiovascular complications that are common to both endarterectomy and stenting: age over 75 years, operator/surgical experience, mild cognitive impairment or dementia, early post-acute coronary artery disease syndrome [15-18]. Other risk factors are more relevant for increasing the incidence of complications with stenting (large extent of calcified lesion and excessive tortuosity of the ICA). Some risk factors are specific to carotid endarterectomy (CEA) (congestive heart failure, very high or very low stenoses, period after radiation therapy, ipsilateral CEA for contralateral ICA occlusion).
Discussions regarding the choice of method for revascularization of extracranial arteries continue [4, 8, 9, 19, 20]. Thus, K. Ziada et al. in 2005 presented the results of carotid artery stenting and CABG. Among the complications of this tactic were myocardial infarction (3%) and acute cerebrovascular accident (ACVA) (2%) [21].
F. Versaci et al. in 2007 reported the results of a new surgical strategy consisting of a sequential hybrid approach with carotid stenting followed by CABG. The procedure was performed in a group of 37 patients. The total incidence of stroke, myocardial infarction and mortality was 8.1%, 2 (5.4%) patients died, 1 patient suffered a stroke after ICA stenting [22-24].
Lack of data in large numbers of patients and unclear long-term results, as well as the need for aggressive antiplatelet therapy, limit widespread adoption of this approach [3, 20, 25, 26]. In the event of bleeding, postoperative antiplatelet treatment with this strategy may have to be delayed, compromising the patency of the stented ICA.
In addition, when considering the issue of ICA stenting versus CEA, one should keep in mind the data of J. McPhee et al [27]. In a study including all 2005 ICA revascularization procedures in the United States (n=135,701), the authors found that ICA stenting increased the incidence of postoperative stroke and mortality by 4-fold (4.6% vs 1.4%, p<0 .05) in comparison with FEE. In addition, ICA stenting doubles the overall risk of postoperative stroke (1.1% vs. 0.57%, p<0.05) compared with the surgical approach.
M. Van der Vaart et al. in 2008 reviewed 12 randomized trials of carotid artery stenting versus CEA. According to the authors, there is no evidence that carotid artery stenting has an advantage in preventing stroke compared with CEA [28].
In a 2010 study of 2502 patients, T. Brott et al. [17] showed that the incidence of stroke or death over 4 years of follow-up in patients with ICA stenting was 6.4%, and in the CEA group it was 4.7% (p = 0.03). When the MI rate was included in the analysis, the overall rate was 1.1% for stenting versus 2.3% for endarterectomy (p=0.03).
Of interest are also the data from the EVA-3S study, which was stopped early due to a high percentage of stroke and significant mortality in the ICA stenting group compared to the CEA group [29, 30].
When talking about the choice of surgical tactics (CEE or carotid angioplasty with stenting (CAS)), one must take into account the possible risks of complications of each treatment method. Thus, with CEE, damage to the hypoglossal and vagus nerves and laryngeal paresis occur much more often. In the early postoperative period, acute paravasal hematomas may occur, causing compression of surrounding tissues, neck organs and displacement of the trachea, which leads to impaired respiratory function [8-10, 14, 19, 20, 31]. With CAS, during catheterization of the carotid arteries and with severe atherosclerotic lesions of the aorta, damage to its intima and embolism of the BCA by atherothrombotic complexes are possible, which is highly likely to lead to the development of stroke [1, 2, 6]. According to the ICAROS study, echo-negative atherosclerotic stenoses contribute to the formation of the largest percentage of emboli during CAS [29, 30].
The purpose of this study is a retrospective analysis of in-hospital results of ICA stenting in patients with multifocal atherosclerosis (MFA).
How the treatment method works
The patient is connected to equipment with which his vital parameters will be monitored. A drug that reduces blood clotting is injected intravenously. If installed, a balloon-expandable stent is inserted through an introducer (an accessory device, a plastic tube with a sleeve). The introduction takes place under angiographic control. When the stent reaches the desired location, it is inflated with a balloon. When installing a self-expanding stent, a catheter is inserted through the introducer and the stent is delivered to the desired location. The catheter is then removed and the stent is deployed. After some time, the stent takes the required shape. The operation lasts on average 1-2 hours.
What happens after surgery?
The surgeon sutures the insertion site of the instruments. This prevents bleeding. A pressure bandage is applied for several hours. After this, the patient is transferred to the intensive care unit. Here, control is exercised over the brain, vascular function, pulse, and blood pressure.
Forecast
Of course, stenting is not 100% effective. However, it allows you to restore the normal functioning of the brain and the vessels that deliver blood and nutrients to it in a large number of cases.
About 20% of patients experience relapses. But today stenting is a technique that is constantly being improved.
Are complications possible?
In some cases, yes!
- Pseudoaneurysm formation. This complication often occurs due to the fault of the doctor. That is why it is very important to wisely select a clinic and a specialist you can trust.
- Spasm, embolism. These complications also arise due to the fault of the doctor. To prevent them, it is necessary to strictly control the guiding catheter, the brain's protection system. Avoid moving them.
- Embolism of the vessels of the head. This complication can cause a stroke. To prevent it, your doctor prescribes special medications.
Possible complications during treatment
Immediate complications occur in 9% of patients. Embolic complications with a closed stent placement are caused by dissection or rupture and embolization of the atherosclerotic plaque; embolic strokes and postoperative transient ischemic attacks rarely occur. The stent may be thrombosed. Complications also include: Acute asymptomatic thrombosis after stent deployment. Recurrent bleeding after initial hemostasis. Subacute thrombosis and intimal hyperplasia leading to stent stenosis or vascular occlusion. The graft material may delay endothelialization, leading to thrombotic closure of the stented vessel. In addition, injured vessels are hypercoagulable.
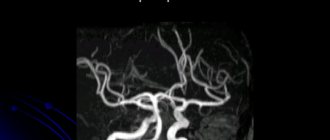
Diagnosis of obstruction of the brachiocephalic arteries
To make an accurate diagnosis before surgery, the following is carried out:
- Duplex scanning of blood vessels.
- Ultrasound.
- Triplex scanning.
- Angiography.
If necessary, an MRI is also prescribed.
During a comprehensive examination, large arteries, surrounding tissues and small vessels are visualized. Thanks to this, the specialist receives important information regarding:
- The presence of blood clots, enlargements, stenoses, detachments, etc.
- Closure or patency of the lumen.
- The presence of various deformations.
- Elasticity and mobility of artery walls.
- Threats of ruptures.