The term “myocardial dystrophy” does not exist as a diagnosis. But cardiologists distinguish this heart pathology separately and associate it with metabolic disorders that lead to a reduction in energy synthesis in myocardial cells.
In the International Classification of Diseases (ICD-10) there is no such nosological form of the disease, since it is considered a complication of other diseases.
Details about the structure of the muscle layer, disruption of the mechanism of myocardial contraction and the causes of myocardial dystrophy can be found in the article “What are diffuse changes in the myocardium and is it dangerous.”
Causes of myocardial dystrophy
The etiology of myocardial dystrophy causes much debate among doctors. Experts believe that the list of causes of metabolic disorders in the heart is extremely wide.
Heart nutritional disorders, as a result of which the cells do not receive enough oxygen and nutrients.
- violation of coronary circulation;
- chronic pulmonary heart disease;
- anemia, hemoglobin level in the blood less than 90-80 g/l;
- altitude sickness;
- arterial hypertension;
- heart defects;
Nervous tension , leading to a significant increase in adrenaline and excessive work of the heart;
- prolonged stress;
- depression;
- neuroses;
Excessive physical activity
- excessive loads in trained athletes;
- intense physical activity in untrained people
- intense physical activity during the period after infectious diseases (sore throat, flu);
Chronic diseases of the digestive system leading to nutritional deficiencies;
- pancreatitis;
- cirrhosis;
- malabsorption syndrome (malabsorption in the intestine);
Eating disorders accompanied by electrolyte imbalance;
- avitaminosis;
- diets with minimal protein and minerals;
Metabolic disorders. Common diseases affect the heart;
- renal and liver failure;
- gout;
- diabetes;
- obesity;
Hormonal disorders. High concentrations of hormones increase heart rate. During intense work, the energy reserves of the myocardium are depleted.
- thyrotoxicosis;
- Cushing's disease;
- menopause;
- puberty;
Poisoning with toxins that damage myocardial cells or disrupt metabolic processes.
- alcohol;
- nicotine;
- drugs;
- taking medications (cardiac glycosides);
- industrial poisons;
The causes of myocardial dystrophy in newborns are:
- oxygen starvation of the fetus;
- intrauterine infections;
- perinatal encephalopathy;
Myocardial dystrophy: symptoms
At the beginning of the disease, signs may not appear, but as it develops, the patient may complain of:
- pain in the heart area of various types (can be either acute or aching, a characteristic feature is that it does not go away after taking medications such as nitroglycerin);
- heart rhythm disturbances (tachycardia, atrial fibrillation, etc.);
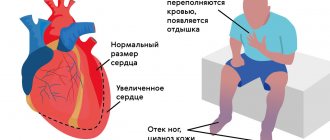
- shortness of breath during movement and at rest;
- swelling of the legs;
- pallor, fatigue, general weakness, decreased performance.
In childhood myocardial dystrophy, the asymptomatic period often lasts a long time, and the disease can be detected only after determining the root cause. In addition, young children do not understand the symptoms to complain about them. This is why regular visits to the pediatrician are so important.
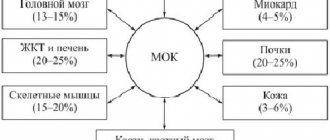
Mechanism of development of myocardial dystrophy
The mechanism of development of myocardial dystrophy does not depend on the cause of the disease. It includes the following steps.
- Violation of the nervous and hormonal regulation of the heart. The heart is under the influence of adrenaline and the sympathetic nervous system. They increase the contraction of the heart and gradually lead to its exhaustion.
- The heart absorbs oxygen worse. At the same time, the myocardial need for oxygen increases.
- A number of changes occur inside the heart cells: calcium levels increase, which disrupts the relaxation of myofibrils. Tissue respiration worsens. Calcium-dependent proteases are activated. These are substances that destroy the structures (mitochondria, myofibrils) of heart cells.
- As a result of impaired fat metabolism, free radicals accumulate in cells, which continue to destroy the myocardium.
- Enzymes are released from damaged lysosomes that destroy the cell structure.
- As a result of these processes, the number of functioning cardiomyocytes and cells of the cardiac conduction system is sharply reduced.
Popular questions about myocardial dystrophy
Can children develop the disease?
Yes, this disease can appear at any age, and therefore in children.
What will happen if left untreated?
If myocardial dystrophy is not detected in time and treated, the development of the disease will lead to irreversible consequences that will affect both the quality of life and its duration.
What complications can there be?
The main complications are chronic heart failure and heart rhythm disturbances. One and the other lead to dire consequences.
Treatment of myocardial dystrophy
Treatment of myocardial dystrophy is aimed at normalizing metabolic processes in the myocardium, improving heart nutrition and eliminating the underlying disease that caused dystrophy.
In our Medical City Alexandrov, the appointment is conducted by an experienced cardiologist, a high-class specialist who will conduct a comprehensive diagnosis of the disease and prescribe the necessary treatment.
By contacting us, you can be sure of a quality result!
To make an appointment with a specialist and find out all the details, please call: 8 (49244) 9-32-49
Complications and prevention of the disease
If treatment is started on time, and this is the first or second stage of the disease, the prognosis is quite favorable. If the root cause is eliminated, then myocardial function and, accordingly, the work of the heart can be completely restored. If the pathological process is advanced to the third stage, that is, the changes are already irreversible, the main task becomes to slow down the development of chronic heart failure and heart rhythm disturbances. And in this case, treatment is necessary for the rest of life.
Prevention of myocardial dystrophy consists of timely identification of the causes that can cause it, as well as a healthy lifestyle, absence of bad habits, adequate treatment of diseases and elimination of possible foci of chronic infection, harmful environmental factors and regular annual examination by specialists.
Stages of the disease
The course of the disease goes through three stages:
- in the first stage (compensation) - myocardial hypertrophy is possible on the ECG, other objective manifestations cannot be identified, but the patient is bothered by rare shortness of breath and fatigue;
- in the second stage (decompensation) - adaptive mechanisms are exhausted, symptoms appear during physical activity, swelling, arrhythmia, pain are added to shortness of breath, there are changes on the ECG;
- in the third stage (total decompensation), the clinical picture of heart failure develops.
Diseases of the myocardium, endocardium and pericardium in pregnant women
Myocardial diseases during pregnancy
Myocardial diseases of inflammatory and non-inflammatory etiology are represented by myocarditis, myocardial dystrophy, cardiosclerosis and myocardiopathy.
Myocarditis is an inflammatory disease of the heart muscle of an infectious, infectious-allergic or infectious-toxic nature. Myocarditis during pregnancy can be caused by viral, bacterial, purulent-septic infection, and are also observed with parasitic and protozoal infestations. In pregnant women, rheumatic carditis, both primary and developed against the background of various defects, is more common. Pregnancy worsens the course of the disease, so myocarditis in the early stages of pregnancy is an indication for its termination. In the case of uncomplicated myocarditis and the absence of serious concomitant diseases, pregnancy continues and proceeds safely.
Myocardial dystrophies are based on biochemical or metabolic disorders in the heart muscle, caused by endocrine diseases or intoxication, as well as metabolic disorders. Myocardial dystrophy does not have a clear clinical picture; the latter usually manifests itself as symptoms of the underlying disease. In severe thyrotoxic cardiodystrophy with atrial fibrillation, pregnancy is contraindicated. Anemic myocardial dystrophy goes away as the anemia is cured, which is usually done effectively.
Cardiomyopathies during pregnancy can be primary or secondary against the background of various general diseases. The primary forms of this pathology include idiopathic myocardial hypertrophy of the non-obstructive and obstructive type. With mild obstruction, pregnancy proceeds favorably, but one should remember the genetic determination of this pathology and the risk of giving birth to a sick child.
Endocardial diseases during pregnancy
There are acute, subacute and prolonged septic endocarditis during pregnancy. The disease is caused by infection during pregnancy (usually strepto- and staphylococci). It is characterized by growths (consisting of fibrin, platelets, polymorphic leukocytes) of various sizes and shapes on the valve leaflets, chordae tendineae and parietal endocardium. The mitral, aortic, or both valves are most often affected. Pregnancy predisposes to the development of endocarditis against the background of various defects, especially in the presence of infection.
Pregnancy with bacterial endocarditis should be interrupted, although this is unsafe and may be accompanied by thrombo-embolic complications and heart failure. Subsequently, if the outcome of the disease is favorable, pregnancy is permissible after a year.
Pericardial diseases during pregnancy
The cause of illness during pregnancy is infection (viral, bacterial, fungal, parasitic). Pericarditis can develop with collagenosis, allergic conditions and metabolic disorders, as well as with radiation injury, after heart surgery. Constrictive pericarditis is a contraindication for pregnancy.
Pregnancy and systemic lupus erythematosus
Systemic lupus erythematosus is an autoimmune disease of connective tissue. It occurs more often in women of reproductive age. It is detected during pregnancy, after childbirth and abortion, sometimes after taking medications (with individual intolerance to sulfonamides, antibiotics), as well as after stressful situations (surgeries, colds, mental trauma). The diagnostic criterion is the presence of lupus cells and specific antibodies in the blood.
Systemic lupus erythematosus during pregnancy - forms and symptoms
The clinical course of the disease can be slow or rapid progression. There are the following forms of lupus erythematosus: visceral, endocardial, polyarthritic, renal, anemic and neuropsychic. It is characterized by a polymorphism of symptoms: skin manifestations, cardiac changes, damage to the lungs, spleen and lymph nodes, vasculitis and thromboembolic complications. Kidney damage with pronounced changes indicates the progression of the disease, is a difficult-to-reversible process and can quickly lead to death. Pregnancy worsens the patient's condition and is contraindicated in most cases.
Pregnancy in women with heart surgery
This contingent of pregnant women (even after successful surgical interventions) should be considered as suffering from heart disease. The decision on the admissibility of pregnancy and childbirth in women undergoing heart surgery should be made taking into account the effectiveness of the operation, the activity of the rheumatic process, possible relapse of the disease, pulmonary hypertension, arrhythmias, heart failure, etc.
Heart surgeries are also performed during pregnancy (at 16-26 weeks).
Management and treatment of pregnant women with heart disease
The question of the possibility of pregnancy in women with heart disease should be decided jointly by a cardiologist (general practitioner) and an obstetrician-gynecologist. If pregnancy occurs, then they must develop an action plan for its management in order to prevent or promptly identify possible complications. If the pregnancy needs to be terminated, this is done in the early stages (up to 12 weeks).
Pregnancy is contraindicated or termination is indicated before 12 weeks in the following conditions:
- any form of anatomical lesion with symptoms of circulatory failure or activity of the rheumatic process;
- bacterial endocarditis;
- pronounced mitral stenosis and combined mitral disease with a predominance of stenosis;
- severe aortic stenosis;
- combined aortic disease;
- coarctation of the aorta and stenosis of the pulmonary artery;
- tricuspid valve defects;
- pulmonary hypertension with any heart defect;
- heart defects in combination with arterial hypertension or chronic glomerulonephritis;
- all “blue” heart defects;
- congenital defects of the “pale” type with signs of severe pulmonary hypertension;
- defects of the interatrial and interventricular septa, as well as patent ductus arteriosus with severe symptoms of reverse blood flow, enlargement of the right heart, signs of decompensation and pulmonary hypertension;
- acute and subacute forms of myocarditis;
- myocardial dystrophy and myocardiosclerosis with dysfunction of the conduction system and arrhythmia;
- myocardial diseases with circulatory failure;
- incomplete surgical correction or recurrence of acquired or congenital heart diseases.
Clinical observation of pregnant women is carried out by an obstetrician-gynecologist together with a therapist and a cardiologist with the participation of a midwife. A thorough examination of the state of the cardiovascular system and all major organs and systems is carried out every 2 weeks, and if necessary, more often.
All pregnant women with diseases of the cardiovascular system are hospitalized at least three times during pregnancy:
within a period of up to 12 weeks for a complete examination, making a full diagnosis and deciding whether it is permissible to continue the pregnancy, developing management tactics and the necessary therapy;
in 28 - 32 weeks of pregnancy - during the period of the most unfavorable hemodynamic conditions and maximum load on the heart for appropriate therapy;
2 - 3 weeks before birth to prepare for childbirth, appropriate therapy and develop management tactics, method of delivery.
If the disease progresses, treatment is ineffective, or complications occur in the heart (arrhythmias, heart failure, thromboembolism, activity of the rheumatic process) and pregnancy (preeclampsia, fetal hypoxia, threat of miscarriage), immediate hospitalization is indicated.
It is advisable to terminate pregnancy at a later stage by cesarean section.
The issue of lactation is decided individually; it is inappropriate in all cases of decompensation, circulatory disorders, and activity of the rheumatic process. To suppress lactation, parlodel is used, 1 tablet (2.5 mg) 2 times a day for two weeks. Dispensary observation continues by an obstetrician-gynecologist and therapist in the postpartum period, then women are under the supervision of a cardiologist.
Complex therapy for pregnant women with heart disease includes
. protective regime, therapeutic nutrition, prevention and treatment of circulatory failure, increased reactivity of the mother and fetus, pathogenetic and symptomatic treatment of the main and concomitant diseases, prevention and treatment of hypoxia and acidosis of the mother and fetus.
Pregnant women with full compensation and the absence of various complications and concomitant diseases do not need special restrictions on physical activity compared to healthy pregnant women.
For all decompensated conditions, heart failure, strict bed rest is indicated, often in a hospital setting.
Drug therapy for pregnant women with heart surgery
Drug therapy is carried out according to traditional principles of cardiology, but taking into account its possible effect on the fetus. It is known that women with heart disease are more likely to give birth to children with congenital defects, including heart defects, which are mainly due to multifactorial causes. Defects are often discovered several months or years after birth. When drug therapy, it is important to take into account the timing of pregnancy: the phase of organogenesis is critical in relation to teratogenicity (8 weeks, for the heart - up to 40 days), after this period the embryotoxic effect of pharmacological agents appears. Of the antihypertensive drugs, nitroglycerin is preferred as an ambulance - 1 tablet under the tongue. Of the anticoagulant agents, heparin is prescribed in the first 10-12 weeks and the last 2-4 weeks of pregnancy, and indirect anticoagulants are prescribed in the remaining periods. Prescribe medications aimed at treating maternal and fetal hypoxia (riboxin, multivitamins, methionine, ascorbic acid, 20-40% glucose solution, unithiol, trental). Oxygen therapy is always indicated.
Careful treatment of myocardial, endocardial and pericardial diseases in pregnant women is very important.
Diagnostic methods
Myocardial dystrophy is indicated by disturbed biochemical tests indicating changes in metabolic processes:
- total protein and protein fractions;
- blood glucose level;
- violation of mineral content (potassium, sodium, magnesium, calcium);
- cholesterol, lipoproteins and triglycerides;
- hormonal background.
The most informative conclusion may be:
- ECG - assessment of ventricular repolarization, conductivity, rhythm, focal and metabolic changes in the myocardium, degree of hypertrophy;
- Doppler echocardiography and ultrasound of the heart - allow you to see and compare with the norm the contractility of the atria and ventricles, the functioning of the valve apparatus, the direction of blood flow, the force of cardiac output;
- X-ray of the chest organs is a technique for detecting congestion in the lungs and expansion of the cardiac boundaries.
Treatment
Treatment of myocardial dystrophy is carried out depending on the severity of the patient’s condition in a hospital or on an outpatient basis.
First of all, therapy uses drugs to eliminate the underlying disease.
Treatment using a hyperbaric chamber allows you to saturate tissues with oxygen
Recommendations for the regimen
The regimen should be taken as seriously as medications:
- the patient should adhere to a constant regimen of getting up in the morning, going to bed in the evening, eating, and walking;
- it is necessary to do daily feasible physical exercises, breathing exercises, swimming, but avoid strenuous sports activities;
- categorically give up all types of alcohol and smoking;
- learn to cope with negative emotions;
- beware of hypothermia.
Dietary recommendations
It must be taken into account that the patient needs an increased dose of vitamins and plastic material for muscle tissue, therefore the diet should provide:
- a sufficient amount of fruits, vegetables, fresh juices;
- liquid up to 1.5 l;
- limit salt to 3 g;
- if you are overweight, reduce your caloric intake;
- Dairy products, kefir, cottage cheese are required;
- lean meat and fish;
- from cereals - buckwheat, millet, rice.
It is necessary to avoid spicy seasonings, fatty meat dishes, rich soups, and coffee.
Use of medications
To stimulate metabolism in the heart muscle, the following are prescribed: Mildronate, potassium and magnesium minerals in Panangin, Asparkam.
Depending on the severity of heart failure and arrhythmia, beta-blockers, Dipyridamole, and agents that reduce blood viscosity are used. For patients without severe circulatory failure, massage, balneological procedures (pine and oxygen baths), and spa treatment are indicated.
It is impossible to cope with a pathology such as myocardial dystrophy with one remedy. It should be “expected” in terms of preventing and treating common diseases. Consult a doctor and undergo medical examination, timely further examination in case of suspicious symptoms.
Causes
The following pathologies can cause disturbances in the contractile function of the heart:
- Excessive physical overload for a long time.
- Deviations associated with abnormal metabolism.
- Hormonal imbalances.
- The effect of drugs (for example, cardiac glycosides, cytostatics, antibacterial agents).
- Chronic breeding grounds for infection in the body.
- Gastrointestinal dysfunction.
- Poisoning by nicotine, ethanol, narcotic drugs, toxic elements at work.
- Poor nutrition (not enough protein, vitamins, microelements).
- Nervous disorders.
- Cardiac and vascular pathologies (defects, myocarditis, hypertension).
Classification
Cardiac dystrophy can have local and diffuse distribution. In the first case, the lesion covers a limited area of tissue, and in the second, the entire muscle layer is affected.
Primary pathology is recorded when it is not possible to find an obvious cause of its origin. This also includes dystrophy of a complex nature, which does not fit any description of all known types of pathology.
Before leading to dangerous complications, myocardial dystrophy goes through three stages of development:
- At the first stage, several lesions of cardiomyocytes appear. But all abnormal phenomena are compensated by the organ itself: the proliferation of neighboring cells occurs. During this period, a person may experience shortness of breath, arrhythmia, and severe fatigue when performing physical activity. The pain in the chest is of a pressing nature and is not related to physical activity. By the end of the day, your legs swell. Stopping the development of pathology at this stage is not particularly difficult.
- In the second stage, you may notice a more intense manifestation of symptoms. It is called subcompensatory. Tissue damage becomes diffuse (diffuse). Areas that have not undergone change try to replenish the missing cells and increase in size due to the growth of new cells. The heart becomes larger than its usual size. Blood is released in a smaller volume. Contractions weaken. The possibility of complete recovery of damage still remains with adequate and timely treatment.
- The third stage leads to degenerative changes in the myocardium. Signs of cardiac dysfunction occur without physical stress. The heart does not cope well with its functions, blood circulation is disrupted, and other organs suffer. Blood stagnates in the vessels of the lungs, the liver hypertrophies. The compensatory mechanism does not work. Dead heart cells cannot be restored.
Changes leading to myocardial dystrophy occur for various reasons. They form the basis for the classification of the main types of myocardial dystrophy.
- dishormonal;
- dismetabolic;
- anemic;
- alcoholic;
- tonsilogenic;
- sports;
- complex;
- mixed.
Types of heart dystrophy
The clinical classification of myocardial dystrophy subdivides it according to pathogenetic causes, the degree of myocardial damage, and anatomical changes in the heart.
Depending on the results of pathological changes in the heart, there are 3 types of dystrophy:
- hypertrophic - leads to an increase in the thickness of the muscle layer;
- restrictive - characterized by a predominance of narrowing of the cardiac chambers;
- dilatational - the cavities expand and increase in size (without hypertrophy).
Depending on the pathogenetic factors, it is customary to distinguish:
- the primary form, if the cause that led to the disease is not clear or the detected myocardial dystrophy of complex genesis does not fit into any nosological form;
- secondary - has a clear connection with the underlying chronic disease.
The patient has to be asked about the connection with a sore throat because he goes to the doctor with heart complaints
Myocardial dystrophy
Signs
Symptoms of myocardial dystrophy depend on the disease that caused the myocardial dystrophy. In most cases, patients complain of discomfort in the heart area, stabbing or aching pain in the heart, shortness of breath during exercise, and weakness. Arrhythmias, swelling of the legs, and decreased performance are also possible.
Description
If there is a malnutrition of the heart muscle, the structure of its cells is damaged and the contractility of the heart decreases. When the damaging factor ceases, it is possible to restore the structure and functions of the myocardium, but prolonged exposure is fraught with heart failure.
There are several reasons for myocardial exhaustion. This
- exhaustion or, conversely, obesity;
- thyrotoxicosis;
- anemia;
- myasthenia gravis;
- dehydration;
- hypo- and vitamin deficiencies;
- hormonal imbalance (menopause);
- intoxication (alcohol);
- physical stress.
Alcoholic myocardial dystrophy is one of the most common types of this disease. It occurs due to prolonged use of alcohol. In this case, metabolic processes in the myocardium are disrupted, which is manifested by tachycardia and lack of air. In later stages, heart failure develops, which is characterized by shortness of breath and swelling.
Myocardial dystrophy often occurs with thyrotoxicosis. In this case, patients complain of shortness of breath, pain in the heart, palpitations and increased fatigue when performing their usual work.
Women often experience myocardial dystrophy, the cause of which is menopause. At the same time, they experience aching pain in the heart, radiating to the left arm. They intensify during high tides. Heart failure rarely develops, only with concomitant arterial hypertension.
Dystrophy develops gradually, in three stages. At the first stage, small foci of degeneration appear in the heart, and the heart gradually begins to enlarge.
At the second stage, the foci of dystrophy increase and merge with each other. At the same time, the cavities of the heart expand, and the contractility of the myocardium decreases. At this stage, heart failure develops and atrial fibrillation may occur.
In the first two stages, dystrophic changes are reversible. At the third stage , necrosis of the heart muscle develops, and a scar forms in place of the necrotic tissue. At this stage, the changes occurring in the heart muscle are irreversible.
Diagnostics
To make a correct diagnosis, you need to be examined by a cardiologist. A detailed survey of the patient, results of electrocardiography, and x-ray examination are required.
It is important not only to diagnose myocardial dystrophy, but also to find out why it developed. To do this, you need to do general and biochemical blood tests, a blood test for thyroid hormones.
This disease must be differentiated from heart defects, myocarditis, coronary heart disease, atherosclerotic cardiosclerosis, and cor pulmonale.
Treatment
Treatment of myocardial dystrophy should be aimed at eliminating the factor that caused it. This could be detoxification therapy, treatment of hormonal diseases, correction of hormonal balance during menopause, diet, vitamin therapy.
It is also necessary to minimize the consequences of the disease. For this purpose, drugs are prescribed that improve metabolism in the heart.
Depending on the patient’s condition, physical activity is either partially limited or bed rest is prescribed. It is also necessary to limit stress.
If you have concomitant diseases, you should consult your doctor about replacing medications that have a negative effect on the myocardium. Thus, with myocardial dystrophy, sensitivity to glycosides increases, so they should be used with caution.
After recovery, patients are followed up with a cardiologist.
Prevention
Prevention of myocardial dystrophy is aimed at preventing or timely and correct treatment of the diseases that cause it.
In addition, it is necessary to lead a healthy lifestyle, eat right, exercise moderately, and monitor your weight.
It is necessary to get rid of bad habits, as alcohol and nicotine have a detrimental effect on the heart.
At work, the influence on humans of harmful substances that can disrupt the functioning of the heart should be limited.
© Dr. Peter