Vein thrombosis is a serious and dangerous disease that, in the absence of correct treatment and prevention, can lead to death. Blood clots sometimes form even for no apparent reason, but most often there are provoking factors - recent surgeries, injuries. To reduce risks, drug therapy is indicated. What medications do doctors prescribe for thrombosis? What is the difference between anticoagulants and antiplatelet agents?
Risk factors for thrombosis
Thrombosis occurs not only in older people, but also in young people. The reason for this is a number of factors that do not themselves lead to the formation of blood clots, but create all the conditions for this. The likelihood of forming blood clots increases in the following cases:
- overweight;
- passive lifestyle;
- forced bed rest for more than three days;
- varicose veins;
- recent myocardial infarction or stroke;
- use of oral contraceptives;
- fractures and injuries of the lower extremities;
- unhealthy diet, unhealthy lifestyle.
How medications help with vein thrombosis
All drugs prescribed for the prevention and treatment of venous thrombosis have a blood-thinning effect, since one of the main causes of the disease is increased blood clotting. They cannot miraculously dissolve existing blood clots, but they do prevent them from enlarging and forming new clots. Medicines to reduce clotting may have different principles of action, but give approximately the same effect. They are taken in courses or on an ongoing basis at the discretion of the attending physician.
Blood thinning medications are selected based on tests, diagnosis, and patient characteristics. Self-medication in this case is unacceptable, as it can lead to serious consequences. One of the main side effects is the risk of bleeding. More often it is minor and manifests itself in the form of bruises and nosebleeds. But an incorrectly selected drug and its dosage can lead to more serious consequences requiring hospitalization.
Blood thinners - differences between anticoagulants and antiplatelet agents
There are two groups of blood thinning drugs - anticoagulants and antiplatelet agents. All of them are intended to prevent thrombosis, but differ in their mechanism of action. Anticoagulants inhibit the activity of proteins involved in blood clotting. Antiplatelet agents prevent platelets from clumping together.
For thrombosis of the veins of the lower extremities, anticoagulants are most often prescribed. Drugs of the second group are indicated more likely for cardiovascular diseases - after valve replacement operations, heart attack or stroke. Their task is to minimize the risk of pulmonary embolism as a result of the formation and separation of a blood clot.
Standing and sitting work, long flights
Those at risk include cooks, salespeople, hairdressers, surgeons, traffic police officers, accountants, programmers, secretaries, as well as those who, as part of their duties, have to fly a lot on airplanes, stand in traffic jams, sit in a car, when people are forced to stay in a car for a long time. static, sitting position.
How to warn. When going on a long journey, sitting or standing idle in the office for hours, make it a rule to change your body position every 30 minutes or just walk. To prevent blood clots, you can also wear compression stockings (support stockings, stockings or tights).
Article on the topic
Thick means dangerous. What you need to know about blood clots
Anticoagulants
Anticoagulants are effective drugs that prevent excessive blood clotting and the formation of dangerous clots. They are divided into two large groups:
- Direct action. Mainly injectable drugs used in hospital settings, such as heparin, rivaroxaban. But there are also medications for oral administration. They act quickly, neutralizing clotting factors in the blood plasma.
- Indirect action. They are vitamin K antagonists and affect coagulation factors, gradually reducing their content in the blood. Many drugs from this group are indicated for continuous use; they begin to act slowly, but the effect lasts a long time. These include Warfarin, Aspirin, Trombital.
Anticoagulants are indicated for deep vein thrombosis, bleeding disorders, prevention of heart attack, stroke.
The most common blood thinners
Drugs in tablet form are excellent for outpatient treatment. Some of them are taken in long courses or on an ongoing basis if there is a high risk of blood clots. Below is a list of the main drugs.
Aspirin
Aspirin is an acetylsalicylic acid drug that has a wide range of uses. Its effect varies depending on the dosage. This is a time-tested, effective antiplatelet agent, especially often prescribed for cardiovascular diseases. In tablets of 50 mg and 100 mg, it is used for continuous use. In a high dose it is indicated for fever, to relieve moderate pain. Can be prescribed for varicose veins, thrombophlebitis.
The tablets irritate the gastric mucosa, so they are recommended to be taken strictly after meals. Erosive and ulcerative diseases of the gastrointestinal tract in the acute stage are a direct contraindication. The medicine is common and relatively safe compared to other antiplatelet agents, but it is still not recommended to take it on an ongoing basis without a doctor’s prescription.
Clopidogrel
An antiplatelet agent prescribed primarily for diseases of the heart and blood vessels - atherosclerosis, coronary artery disease, heart attack, unstable angina. Suppression of platelet aggregation is noted from the first day of administration.
Clopidogrel does not have too many contraindications, but it can cause side effects such as nosebleeds, abdominal pain, and dyspepsia. In patients over 75 years of age, treatment is carried out with caution, in moderate dosage.
Warfarin
One of the most common, frequently prescribed anticoagulants. Widely used for the treatment and prevention of thrombosis of various etiologies, thrombophlebitis, varicose veins, and secondary prevention of myocardial infarction. An excellent drug with repeatedly proven clinical effectiveness and safety. One of the few coagulants allowed during breastfeeding.
The drug can be taken only as prescribed by a doctor, since even many doctors note the difficulty of selecting a dose at the beginning of treatment for each individual patient. In addition, it is necessary to constantly monitor hemostasis indicators.
Trombital
The list can be supplemented with a modern combination drug consisting of acetylsalicylic acid and magnesium hydroxide. The antiplatelet agent prevents the formation of blood clots and, compared to Aspirin, does not irritate the gastric mucosa. For this reason, Trombital is prescribed to people with gastrointestinal diseases.
But the drug is used mainly for cardiac diseases, for the prevention of myocardial infarction, and for unstable angina. To reduce the risk of thrombosis of the veins of the lower extremities, doctors usually give preference to other drugs.
Thrombosis of arteries and veins: symptoms, causes, treatment and prevention
Thrombosis is a dangerous condition in which a blood clot forms in a vessel. Such a thrombus can grow, clogging the vessel until it completely occludes, but under certain conditions it can also “break off”, becoming a thromboembolus.
Treatment of this pathology is still difficult, after which relapses are possible1. Therefore, it is important to know the causes of thrombosis so that, if you discover them in yourself, you can begin prevention in time. We will talk about this, as well as about the manifestations of the disease.
Causes of blood clots
Blood clots in blood vessels occur under the influence of a complex of factors that could change:
- blood viscosity;
- the speed of its movement;
- the condition of the wall of blood cells, especially platelets, which also affected their electrical charge.
The main causes of thrombosis include:
A. Conditions in which the blood coagulation system becomes overactive, and its antagonist - proteins and enzymes of the blood anticoagulation system - cannot prevent this
These can be hereditary or acquired diseases, the most common of which are:
- antiphospholipid syndrome;
- hemophilia;
- increased blood levels of the amino acid homocysteine;
- systemic lupus;
- decreased concentration of proteins C or S in the blood;
- antithrombin deficiency;
- DIC syndrome is an acute condition that develops in many serious diseases (including infectious ones), after operations, during complications of pregnancy: preeclampsia and eclampsia, incompatibility of mother and fetus by blood type, and others.
B. Vascular injuries
They occur during the placement of venous catheters (then symptoms of venous thrombosis of the upper extremities are observed), operations - especially during the installation of prostheses and consolidation of fractures, and surgical treatment of the pelvic organs.
B. Providing conditions for blood stagnation
This leads to:
- long-term immobilization: in the treatment of fractures, as well as other serious diseases;
- paralysis;
- paresis;
- long journeys;
- air travel - especially in the presence of concomitant pathologies, for example, rhythm disturbances or previous myocardial infarction;
- anesthesia, when it lasted more than 60 minutes and involved the use of artificial ventilation and, accordingly, the use of drugs that relax the muscles.
D. Certain diseases
Another reason for the development of thrombosis are pathologies that affect blood clotting or the flow of blood vessels. This:
- tumors: any malignant, including leukemia;
- acute myocardial infarction;
- inflammation of the colon;
- obesity;
- stroke;
- heart failure;
- kidney diseases in which nephrotic syndrome develops (edema, loss of proteins in the urine, increased cholesterol levels);
- paroxysmal hemoglobinuria;
- systemic vasculitis, including those accompanying joint diseases;
- previous thromboembolism;
- decreased platelet levels associated with the need for long-term use of heparin;
- vascular atherosclerosis.
In addition, a fairly common cause of thrombosis is pregnancy, especially its second half, as well as the postpartum period. This is due to an increase in progesterone levels, which increases blood viscosity. An enlarged uterus can compress the veins of the pelvis, as a result of which the speed of blood flow in them decreases by 2–3 times1. Thrombosis can also begin when, in the postpartum period, physiological thrombosis of the veins of that part of the uterus that previously communicated with the placenta begins1.
D. Taking medications
Contraceptives, hormonal drugs - including those for the treatment of malignant neoplasms, chemotherapy drugs, including tamoxifen - increase the risk of intravascular blood clots.
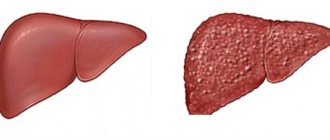
Difference between the causes of arterial and venous thrombosis
In general, the reasons for the development of thrombosis in the venous bed are listed above. Venous vessels are distinguished by the fact that their muscular wall is poorly developed, and the movement of blood in them occurs slowly. This promotes stagnation and the formation of blood clots.
In this regard, the vessels of the inferior vena cava system are the most vulnerable: the blood in them is forced to rise against gravity - only with the help of the muscles of the lower leg, the suction pressure of the lungs and the pericardium. Therefore, symptoms of thrombosis of the lower extremities and pelvic veins - namely, they are part of the inferior vena cava system - occur in 95% of cases of venous thrombosis (phlebothrombosis)2.
Most often, blood clots form in the deep veins of the leg. This is facilitated by conditions in which the “second heart” of the body, the calf muscles, is switched off. The main one is anesthesia with the use of muscle relaxants, drugs to relax all muscles, making many abdominal operations possible. Muscle relaxants cause much deeper muscle relaxation than is possible during sleep or even with muscle paralysis. This is why it is important to wear compression garments before surgery: it supports the “second heart” in artificial tone.
Now about the causes of arterial thrombosis. In arterial vessels of large and medium caliber, the blood flow speed is high3. Therefore, blood clots can occur:
- On atherosclerotic plaques: these lipid deposits occur mainly in areas of uneven blood flow, so it is easier for a blood clot to stay here.
- In arteries of small diameter, where the speed of blood flow is low.
- On the walls of an aneurysm - a pathological expansion of the vessel. Consequently, with Marfan syndrome, Ehlers-Danlos syndrome, neurofibromatosis, Erdheim tumor and other pathologies in which aneurysms are formed very often - due to a violation of the structure of the vascular walls.
- In the area of the artery wall that is inflamed or damaged by its own immunity.
- In a place where the artery is compressed: by bone, tumor, cyst.
- In a place where the wall of an artery (mostly of small diameter) consists of “wrong” proteins that attract platelets to themselves, although they should repel them due to the difference in electrical charges. This occurs with collagenosis.
- With generalized DIC, when the blood coagulation system practically no longer stops the speed of blood flow.
Factors predisposing to angiothrombosis
Not everyone who has the above causes of thrombosis necessarily develops the disease. Often external influences are also needed, which will trigger the pathological formation of blood clots in the vessels.
These factors become:
- Smoking. In this case, thrombosis mainly develops in the arteries - and the vessels of the lower extremities suffer from smoking 2-3 times more often4 than this bad habit causes cardiac ischemia. The reason is a prolonged spasm of blood vessels (vasa vasorum), small vessels that supply arteries and veins.
- Diabetes. This pathology leads to disruption of the properties of the vascular wall, mainly arterial. As a result, although diabetes is not the direct cause of thrombosis, it increases the risk of its development by 2–4 times1. In addition, pathology is also a factor that will worsen the prognosis after surgical treatment of arterial thrombosis, therefore, if it is present, it is necessary to maintain blood glucose within normal limits.
- Violation of fat metabolism. Each increase in total cholesterol concentration by 10 mg/dL increases the risk of obliterating atherosclerosis, and with it thrombosis of the lower extremities, by 5–10%1.
- Impact of local factors. If there is a cause for the development of thrombosis, its risk is higher in those people whose limbs are more often injured (minor scratches and cuts count), hypothermia or overheating.
- Stress. Psychogenic stress leads to the production of increased levels of cortisol, and it leads to prolonged spasm of the arteries with disruption of normal blood flow through the vessels.
Risk factors for angiothrombosis - venous and arterial - also include those circumstances that cannot be changed, but can be taken into account by starting prevention in time. This:
- Age: the older a person is, the more attention he should pay to his health, including the condition of his lower extremities. The symptoms of thrombosis described below are not normal at any age.
- Male gender: this increases the risk of clots in both veins and arteries.
How does angiothrombosis manifest?
In general, the symptoms of thrombosis depend on three factors:
- where the blood clot formed - in an artery or vein;
- in which vessel and at what level did the thrombus appear;
- whether the clot blocked the vessel, how quickly it happened.
Manifestations of phlebothrombosis are swelling and pain in the limb, which intensifies when walking. In this case, the swollen skin becomes bluish, this color becomes brighter when standing. The affected limb is warmer than the healthy one. Under the swollen skin you can feel a painful cord - this is the affected vein. Active palpation or squeezing of a limb is dangerous for the development of pulmonary embolism.
The level of swelling depends on the location of the blood clot: the lower it is, the less surface area of the leg or arm will swell. In some cases, the disease occurs hidden. Then thrombosis of the lower extremities is detected after symptoms of pulmonary embolism: a sharp feeling of lack of air, shortness of breath, fainting, strong heartbeat and cough.
With arterial thrombosis, the symptoms are different. While the clot grows and blocks the artery by 25% or less, the limb will develop:
- numbness;
- tingling;
- chilliness that comes in “hot flashes” and is localized closer to the fingers;
- heaviness in the legs - when exercising.
As the blood clot increases, more noticeable symptoms of thrombosis are observed: the limbs begin to tire faster, become more sensitive to cold, and “pins and needles” and numbness occur more often and last longer. One limb becomes paler, drier and colder than the other. It often develops pustules and inflammations that do not heal for a long time.
As the disease progresses, pain occurs in the affected leg or arm, and with thrombosis of the arteries of the lower limb, lameness appears. And in an advanced stage, if acute thrombosis does not develop, trophic ulcers appear - first as superficial wounds that do not heal, and then as deep “potholes” with uneven edges. The final symptoms of thrombosis, which develops gradually, are the development of wet gangrene, the appearance of signs of general intoxication: nausea, weakness, loss of appetite, headaches. Along with this, body temperature often also rises. If the affected part of the limb is not amputated, the functioning of the kidneys, cardiac and respiratory systems is disrupted.
If the blood clot in the artery grows quickly, acute symptoms of limb thrombosis appear:
- skin swelling;
- severe pain in the leg or arm;
- pain when touching a limb;
- rapid development of gangrene.
Changes are observed below the artery blocked by the thrombus. This is where the pulse disappears, which is noted at the very beginning of the disease.
Complications
Regardless of the cause of thrombosis, its main complications are thromboembolic. This term refers to the detachment of a blood clot from the wall of a vessel and its blockage of an artery of suitable diameter, as a result of which the part of the organ that fed from this artery does not receive nutrition and dies.
Most often, thromboembolus enters the arteries extending from the aortic arch (this includes the arteries supplying the brain), in second place are the large arteries of the pelvis and lower extremities, then the arteries going to the internal organs. Thromboembolism of the upper limb arteries very rarely develops1.
One of the common complications of the most common thrombosis - deep vein thrombosis of the lower extremities - is PE (pulmonary embolism), when a larger or smaller area of the lungs ceases to be supplied with blood. PE does not develop in every case of phlebothrombosis, but, unfortunately, risk factors for this dangerous disease have not been identified. It is believed that the greatest danger of pulmonary embolism exists in the early stages after the onset of symptoms of thrombosis of the extremities - while the thrombus is still loosely fixed to the vein wall and can come off. However, thromboembolism can occur after a long period of time after phlebothrombosis, especially if no preventive measures are taken.
In addition to thromboembolism, phlebothrombosis can be complicated by the growth of a blood clot and its spread to nearby veins. For example, from the deep veins of the leg, a clot can “grow” to the popliteal vein, and from the superficial femoral vein to the common femoral vein. In this case, the outflow of blood from the limb worsens, and the risk of blood clot rupture increases.
Treatment
Therapy should be started as early as possible. In acute thrombosis - both venous and arterial - it consists of administering those drugs that can dissolve the blood clot. If drug thrombolysis is ineffective, surgery is performed to remove the blood clot from the vessel. After this, anticoagulant therapy continues under the control of coagulation parameters.
Treatment is often performed in the intensive care unit, under the supervision of a vascular surgeon.
For chronic symptoms of thrombosis of the upper limbs or legs, treatment is also prescribed by a vascular surgeon. In the initial stages, it is conservative and consists of prescribing vasodilators, angioprotectors, B vitamins, and cholesterol-lowering agents; for phlebothrombosis - venotonics.
Prescription of blood thinning medications is mandatory. Thrombo ACC is a drug of acetylsalicylic acid that blocks the deposition of platelets on the walls of blood vessels, including the affected one, thereby preventing the blood clot from growing. Thrombo ACC tablets are coated with an enteric film coating, which reduces the likelihood of developing local irritant effects on the stomach.
In case of advanced chronic thrombosis, it is necessary to restore the patency of the vessel. The decision on surgical treatment to restore the patency of the vessel is made by the doctor. Regardless of the cause of thrombosis, after surgery, anticoagulants and/or antiplatelet drugs are prescribed for a long period.
Prevention
It consists of improving blood flow in the extremities. To do this you need:
- maintain blood pressure, cholesterol and blood glucose within normal limits;
- undergo preventive examinations, respond in a timely manner to pathological changes in the heart and blood vessels;
- walk more;
- avoid standing for long periods of time;
- reduce salt intake;
- enrich the diet with foods rich in fiber, as well as polyunsaturated fatty acids, vitamins E and P;
- protect limbs from injury, hypothermia and overheating.
If you have one or more risk factors, you need to get your doctor’s recommendations for preventive use of Thrombo ACC.
The drug is adapted for long-term use. Acetylsalicylic acid in cardiac dosages has been actively used by specialists for many years to prevent thrombosis and their thromboembolic complications. * There are contraindications, before use you must consult a specialist 1 Zatevakhin I.I. Treatment tactics for acute thrombosis of the arteries of the lower extremities // Materials of the fourth international surgical congress “Scientific research in the implementation of the Russian Population Health program” - M., 2012. 2 Arterial thrombosis and embolism of the extremities / Under. ed. IN AND. Lupaltsova, S.S. Miroshnichenko, I.A. Dekhtyaruk / Kharkov, KhNMU, 2010 3 Ministry of Health of the Russian Federation. Clinical recommendations. Diseases of the arteries of the lower extremities. 2021 (reviewed every 3 years). 4 A. K. Lebedev, O. Yu. Kuznetsova. Deep vein thrombosis of the lower extremities. Clinical recommendations. / M, 2015. RUS-GPS-THR-NON-01-2019-1486
Blood thinners for injection
Direct anticoagulants are most often available in the form of an injection solution. Some are used only in hospitals, others are intended for self-administration by patients. At the moment, two drugs are most widely used.
Fraxiparine
Direct anticoagulant, low molecular weight heparin. Can be used by patients independently as prescribed by a doctor. It comes in a syringe with a small needle. It has a fast but short-lasting effect.
It is often prescribed by doctors for vein thrombosis; according to their observations, in most cases there is a pronounced positive dynamics and regression of the thrombotic process. The drug is potent and is prescribed with caution to elderly people, patients with low body weight, and severe arterial hypertension.
Heparin
One of the most common, frequently used direct-acting anticoagulants, widely used in hospitals for the treatment of patients with cardiovascular diseases, venous thrombosis, pulmonary embolism, and acute myocardial infarction.
Compared to other anticoagulants, it has a low cost, so it still remains the main drug in this group, despite the emergence of more modern analogues. It is practically not used at home due to the complexity of dosing, the injection form and the increased risk of bleeding.
To reduce the risk of thrombosis, in addition to blood-thinning drugs, agents may be prescribed to strengthen the walls of blood vessels and lower cholesterol levels. Considerable importance is attached to lifestyle - giving up bad habits, healthy eating, physical activity. The daily routine depends entirely on the person, and this is already a big step towards the prevention of thrombosis. But to prescribe the correct drug treatment, you need to consult a doctor.
Signs of pulmonary thromboembolism
- A sharp decrease in blood pressure.
- Severe shortness of breath.
- Interruptions in the functioning of the heart.
- Pain in the chest area.
- Malfunctions
- gastro-
- intestinal tract.
- Blue in the face
- skin.
- Cold,
- sticky sweat.
The first thing to do if you suspect thromboembolism is to urgently call an ambulance, and before the medical team arrives, you need to lay the patient on a hard, flat surface and ensure complete rest. Calling an ambulance is very important - diagnosis
"thromboembolism" can be confirmed using an ECG. Doctors have 2–3 hours to administer drugs that dissolve blood clots (thrombolysis) or perform surgery. In mild cases, you can get by with prescribing anticoagulants.