Hypertension (essential or primary hypertension) is a chronic disease associated with a long-term and persistent increase in blood pressure (BP).
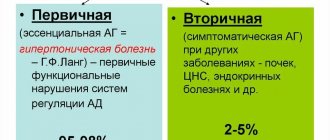
There are two forms of hypertension (hypertension): primary and secondary. Approximately 90-95% of patients with hypertension have the primary form. Unlike secondary hypertension, primary hypertension does not have a clearly defined known cause. Therefore, its diagnosis is made after ruling out known causes, which include what is called secondary hypertension. For example, blood pressure may increase symptomatically with kidney disease, and so on.
Blood pressure: Blood pressure resulting from the work of the heart, which pumps blood into the vascular system, and vascular resistance.
Blood pressure readings are usually given as two numbers: for example, 120 over 80 (written as 120/80 mmHg).
The top number is called systolic blood pressure (the higher pressure and the first number recorded) - this is the pressure that blood puts on the walls of the artery when the heart contracts to pump it to peripheral organs and tissues. The bottom number is diastolic blood pressure (the lower pressure and the second number recorded) - this is the residual pressure exerted on the arteries when the heart relaxes between beats.
Normal blood pressure is a relative value, which depends on age, physical activity, psychological state, and even on the use of various medications.
Hypertension occurs when the body's smaller blood vessels (arterioles) narrow, causing the blood to put undue pressure on the vessel walls and causing the heart to work harder to maintain the pressure. In this case, blood pressure reaches or exceeds 140/90 mm Hg.
Diastolic blood pressure is more common in people under 50 years of age. As we age, systolic hypertension becomes a more serious problem. At least a quarter of the adult population (and more than half of those over 60) have high blood pressure.
What is hypertension?
A syndrome in which there is a regular, long-term and persistent increase in blood pressure is called “arterial hypertension” or “hypertension”. This syndrome may appear:
- in case of hypertension (HTN) - a primary independent disease;
- for secondary (symptomatic) hypertension , which is a consequence of disruption of the functioning of various organs - kidneys, adrenal glands, thyroid gland and others.
Hypertension accounts for the majority of cases of hypertension. The etiology of hypertension is not reliably known, but it is based on primary functional disorders of the systems that regulate blood pressure.
Risk factors for developing hypertension include:
- hereditary predisposition;
- a sedentary lifestyle, which reduces the body’s adaptive capabilities and disrupts the functioning of the circulatory system;
- high body mass index. In obese people, the risk of developing hypertension increases 2-6 times;
- excess salt in the diet, which leads to the accumulation of excess fluid in the body, which increases the load on the cardiovascular system;
- drinking alcohol, smoking;
- elderly age. The older a person gets, the higher their risk of developing the disease.
It turns out that in most cases, bad habits lead to hypertension - physical inactivity, overeating, poor nutrition, nicotine and alcohol addiction. That is why hypertension is considered a pathology directly related to lifestyle, and changing it for the better is the main element of successful treatment.
Causes and risk factors
Despite many years of active research, there is no unifying hypothesis to account for the pathogenesis (mechanism of occurrence) of hypertension. In chronic long-standing hypertension, blood volume and cardiac output are often normal, so hypertension is maintained by increased systemic vascular resistance rather than increased cardiac output. There is also evidence of increased vascular tone. In addition, disturbances in the nervous and endocrine regulation of blood pressure play a role in the development of the disease.
Many factors can affect blood pressure, including:
- Genetic, which play an important role in the occurrence of hypertension.
- How much water and salt is in your body.
- The condition of your kidneys, nervous system and blood vessels.
- Levels of various body hormones.
- Age. Blood pressure gets higher as you get older. This is because blood vessels become stiffer as a person ages.
You are at increased risk of hypertension if you:
- Are you obese?
- Frequently experience stress or anxiety;
- Drinking too much alcohol;
- Consume too much salt;
- Have a family history of the disease:
- Diabetic;
- Smoke;
- You lead a sedentary lifestyle;
- You are experiencing stress.
What blood pressure is considered high?
Blood pressure is a factor that gives the specialist important information about the functioning of the circulatory system. Blood pressure levels are affected by:
- The magnitude of cardiac output, which in turn depends on the contractility of the left ventricle of the myocardium, heart rate and other parameters.
- Total peripheral vascular resistance (TPVR) is an indicator that reflects the ability of blood vessels to resist blood pressure from the inside. OPSS depends on the tone, stiffness of blood vessels, and blood viscosity.
- Circulating blood volume.
Blood pressure has upper and lower limits. The upper pressure is called "systolic", the lower - "diastolic". The first value reflects the force of blood pressure in the arteries during myocardial contraction, the second - at the moment of relaxation of the heart muscle.
The ideal pressure is considered to be 120/80 mm Hg. Art. Depending on the individual characteristics of a person (gender, age, physical activity), a slight deviation of these values down or up is allowed. However, in any person, blood pressure should not exceed 140/90 mmHg. Art. Higher levels are potentially dangerous and can lead to functional and organic damage to target organs.
Stages of pathology
Depending on the degree of increase in blood pressure, three stages of hypertension are distinguished ⇓⇓⇓
First stage of headache
In the first stage of hypertension, high blood pressure can independently return to normal values. As a rule, at this stage of the disease, target organs are not affected and there are no complications.
Second stage of headache
At the second stage of hypertension, a person may experience various pathological changes:
- thickening of the walls of the left ventricle of the myocardium, which often leads to heart failure and coronary heart disease;
- atherosclerosis - the formation of atherosclerotic plaques on the walls of blood vessels that impair blood circulation;
- retinal angiopathy is a violation of the tone of the vessels that supply the iris of the eye.
At the second stage of hypertension, normalization of blood pressure is possible only with the help of medications.
Third stage of headache
The third stage of hypertension can lead to severe complications:
- stroke - acute disruption of blood supply to the brain;
- aortic dissection - rupture of the largest artery. If the aortic wall is completely ruptured, massive blood loss occurs;
- myocardial infarction - necrosis of a section of the heart muscle;
- renal failure - decreased excretory capacity of the kidneys.
In the third degree of hypertension, blood pressure is difficult to normalize even with the help of medications. A person may experience hypertensive crises, during which blood pressure rises sharply and urgent medical attention is required.
What symptoms may indicate hypertension?
As a rule, the disease is asymptomatic for a long time. In some cases, increased pressure is accompanied by:
- frequent heart rate;
- headaches, dizziness;
- weakness, fatigue;
- redness of the facial skin;
- increased sweating;
- blurred vision, ringing in the ears.
However, such symptoms are not specific to hypertension and may be signs of other diseases or fatigue. Therefore, pathology can be detected at an early stage only by regularly measuring blood pressure.
Cost of treatment for stage 3 hypertension
The cost of treatment for third-degree hypertension for each patient is calculated individually, taking into account factors such as:
- age and general condition of the patient;
- the presence of associated complications;
- etiology of the disease, etc.
It's cheaper with us
- Beneficial programs for annual placement, pregnancy management, medical examination and “check-up” with discounts from the price list to 25%
- Discounts for disabled people, veterans, pensioners 10%
- Discount on deposit program up to 25%
- Discounts on promotions and seasonal offers up to 50%
How is the disease diagnosed?
To diagnose arterial hypertension, a doctor needs to take several blood pressure measurements at different times of the day. If necessary, a specialist can prescribe ABPM - an instrumental study in which blood pressure is monitored throughout the day using a special device.
Differential diagnosis of hypertension occurs as follows:
- An examination of organs whose pathologies could cause increased blood pressure is performed. For example, the examination may include an ECG, ultrasound of the kidneys, and fundus examination.
- If secondary hypertension is excluded and a specific cause for the increase in blood pressure is not found, then a diagnosis of hypertension is made.
Diagnostic measures
A treatment regimen is drawn up by a cardiologist after a comprehensive examination, identifying pathologies in target organs, determining the form of the disease and the causes that led to the disorder. But the main sign remains the indicators of systolic and diastolic pressure. To determine these data, studies are carried out on:
- pressure stability throughout the day;
- degree of risk of developing complications of the disease;
- exclusion or confirmation of increased blood pressure as a complication of other ailments;
- identification of factors contributing to hypertension;
- identification of pathological changes in other organs and systems.
The first thing the doctor does is measure your blood pressure and give recommendations for self-diagnosis at home. For hypertension, blood pressure is measured 2-3 times a day for a week, recording all data in a special diary. This allows the doctor to make an accurate diagnosis and take into account the peculiarities of the course of the disease. The physical examination is complemented by the collection of data obtained from a patient interview.
Additionally, daily blood pressure monitoring is prescribed using a special device in a hospital setting. An obligatory part of the diagnosis is an electrocardiogram and ultrasound of the heart. The techniques help to see any type of tacharrhythmia and assess the thickness of the ventricular walls. If abnormalities in the functioning of the internal organs are suspected, a magnetic resonance therapy study is carried out, and ultrasonography is prescribed to determine the size of the kidneys.
Prevention measures
Measures to prevent hypertension include:
- regular physical activity;
- giving up alcohol and smoking;
- balanced diet.
- dosed consumption of table salt (no more than 5 g per day).
Also, do not forget to regularly measure your blood pressure with a tonometer, which will allow you to notice its increase in time and seek medical help.
At President-Med clinics you can
- undergo examination and treatment in more than 30 medical specialties, rehabilitation after strokes, surgeries, injuries,
- pass various types of tests (more than 5,000 types of tests and laboratory tests),
- undergo functional diagnostics (ultrasound, endoscopy: gastroscopy), ECG, installation and interpretation of ABPM and Holter ECG and others,
- pass a medical examination in one day, undergo a medical examination (for both organizations and individuals), undergo a medical examination (for both organizations and individuals),
- obtain all kinds of certificates - certificates from the traffic police and for admission to sports, to purchase weapons, to a sanatorium,
- if there is evidence, issue a certificate of temporary incapacity for work,
- draw up and receive other types of medical documentation,
- make any injections,
- use the services of one-day surgery or day hospital.