Sometimes cancer patients require blood transfusions. If the doctor said that he plans to prescribe a blood transfusion, the patient usually has a lot of questions. Why is the procedure needed? Did something terrible happen? How safe is blood transfusion? Can you get HIV and other dangerous infections from a donor? How will the body react to someone else's blood? Will there be any complications? Is it possible to refuse the procedure or replace it with something else?
Below you will find answers to many questions.
- What you need to know about blood?
- In what cases do cancer patients need blood transfusions?
- What are the types of blood transfusion?
- Red blood cell transfusion
- Plasma transfusion
- Platelet transfusion
- Cryoprecipitate transfusion
- Leukocyte transfusion
- How is the blood transfusion procedure performed?
- From whom can a blood transfusion be given?
- How is donor blood tested?
- Are there any alternatives?
- How safe is it?
- Is it possible to refuse a blood transfusion?
- Price
What you need to know about blood?
Doctors and scientists often refer to blood as the body's internal environment. It washes all organs. Blood performs many important functions: it carries oxygen, nutrients and hormones, removes waste products of metabolism, provides immune protection, and helps regulate body temperature.
Blood consists of two main parts:
- The liquid part is plasma. It is a solution of salts, ions, proteins and other substances.
- Blood cells. Erythrocytes (red blood cells) contain hemoglobin and transport oxygen. Leukocytes (white blood cells) provide nonspecific and immune protection. Platelets (blood platelets) form a clot when bleeding needs to be stopped.
Book a consultation 24 hours a day
+7+7+78
Indications for autohemotherapy:
Due to the fact that autohemotherapy causes persistent activation of rehabilitation and protective mechanisms, intensive healing of wounds and injuries, accelerated recovery from inflammatory processes, it is very popular and is included in treatment regimens for various dermatological and cosmetic problems among all ages and categories. Autohemotherapy gives good results in the treatment of indolent and recurrent diseases, has a positive effect on the body as a whole and on the skin in particular:
- getting rid of purulent and inflammatory processes;
- acceleration of reparative processes;
- improvement of metabolism;
- strengthening the immune system;
- improvement of blood and lymph flow;
- normalization of the endocrine system;
- removal of waste and toxins from the body;
- restoration of performance and vitality.
In what cases do cancer patients need blood transfusions?
The cause may be the malignant tumor itself or side effects of antitumor treatment.
Some types of cancer, especially tumors of the gastrointestinal tract and tumors of the female genital area (vagina, cervix, uterus), can cause internal bleeding.
With a long course of cancer, various disorders occur in the body, which cause the so-called anemia of a chronic disease.
Some malignant tumors affect the red bone marrow (the main organ of hematopoiesis), or organs that are necessary to maintain a normal number of blood cells (spleen, kidneys). These types of cancer may also require blood transfusions.
Donor blood is needed by patients after complex operations that are accompanied by large blood loss.
Chemotherapy and radiation therapy affect not only tumor cells, but also other rapidly dividing cells in the body. Sometimes they cause quite a lot of damage to the red bone marrow. It disrupts the production of blood cells, which threatens anemia, bleeding, and severe infections against the background of decreased immunity. Blood transfusion helps normalize the patient's condition and prevent complications.
What does transfusion help with?
Solid tumors lead to significant changes in the hematopoietic system. Under their influence, anemia and abnormalities in the blood clotting system can develop.
The disintegration of tumors leads to depletion of the bloodstream and blood reserve of the body. Surgical treatment also leads to massive bleeding. All of the above factors lead to the fact that the body’s own reserve is depleted and it requires a blood transfusion from a donor. Due to insufficient blood volume, treatment may be delayed because In case of anemia and thrombocytopenia, chemotherapy cannot be administered.
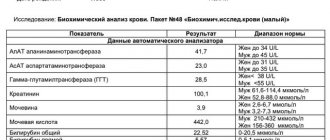
Chemotherapy drugs can have side effects on blood germs and worsen thrombocytopenia. That is why constant monitoring of red and white blood indicators and coagulation properties is necessary. If any deviations from the norm are noted, blood transfusion is prescribed according to all rules.
Red blood cell transfusion
The main function of erythrocytes (red blood cells) is the delivery of oxygen to tissues and the return transport of carbon dioxide to the lungs. A condition in which the number of red blood cells in the blood decreases is called anemia. Actually, this is an indication for red blood cell transfusion. The doctor makes a decision depending on how quickly the anemia increases:
- With chronic anemia, which increases gradually, there is no need to rush. The doctor monitors the patient’s condition, controls the level of red blood cells and hemoglobin. If these indicators decrease significantly, or the patient’s condition worsens, red blood cells are transfused. For heart and lung diseases that impede oxygen delivery to tissues, transfusions may be required even if there is a relatively small decrease in hemoglobin levels.
- Acute blood loss requires immediate action. This usually happens during surgery. If the doctor is planning a complex operation during which the patient will lose a lot of blood, blood transfusion may be performed in advance.
Blood. To pour or not to pour? Part 1
Professor Nazarov I.P.
Currently, many issues of blood transfusion are controversial. Scientists and researchers often express ambiguous and sometimes opposing points of view on blood transfusion therapy. At the same time, practitioners at the patient’s bedside or at the operating table are forced to take specific measures in this direction. In this regard, not only moral and ethical, but purely legal problems arise, both for patients and doctors. Often, the very lives of patients depend on how correctly these issues are resolved. We do not consider the answers to some questions published below to be the “ultimate truth,” but we hope that they will find a certain response from readers and will serve as a stimulus for further discussion on current issues of infusion-transfusion therapy.
Question 1. Is it possible to say that only blood transfusion (whole blood, red blood cells, plasma and its fractions) is the only option and absolutely necessary procedure (type of treatment) for patients who require the appropriate type of medical treatment for life-saving reasons?
Answering this question, it is necessary to determine from a modern perspective the indications for blood transfusion and the principles of replenishing acute and chronic blood loss.
Blood loss
– a pathological condition of the body that develops as a result of extravasal bleeding and intravascular sequestration, accompanied by the occurrence of a number of compensatory and pathological reactions. Blood loss of 5-10% of the initial volume is tolerated almost unnoticeably. Acute blood loss of 50% of the blood volume leads to acute circulatory failure and almost immediately to deep shock. However, in the occurrence of shock, not only a decrease in blood volume is important, but also the rate of blood loss and compensation disorder.
Determining the degree (severity) of blood loss is of great practical importance and largely determines the treatment tactics for acute blood loss. There are a significant number of classifications of the degree of blood loss based on various clinical and laboratory data. The most commonly used classifications divide blood loss into four stages: mild, moderate, severe and extremely severe. Thus, the American College of Surgeons in 1982 adopted 4 degrees (classes) of acute blood loss, based on the volume of blood loss and clinical symptoms. In the first degree, the loss of blood volume does not exceed 15%, and clinical symptoms are either absent or there is only tachycardia, which manifests itself primarily in a standing position. In the second degree, the loss of bcc is 20-25%. At the same time, in the supine position, blood pressure may not change or be slightly reduced, however, when performing an orthostatic test, sitting in bed with legs down, orthostatic hypotension occurs (blood pressure decreases by at least 15 mm Hg). Urine flow is preserved at this stage. In the third degree, BCC decreases by 30-40%, which causes arterial hypotension in the supine position and oliguria less than 400 ml/day. A loss of more than 40% of the blood volume causes extremely severe (fourth) degree of blood loss, life-threatening. Clinically, this is manifested by collapse with extremely low blood pressure and impaired consciousness, up to its loss.
The goal of all efforts in the treatment of acute blood loss is to maintain adequate tissue oxygen consumption to maintain tissue metabolism.
The basic principles of treatment of acute blood loss include the following measures:
- Performing final hemostasis.
- Restoration of blood volume and elimination of hypovolemia.
- Maintaining cardiac output.
- Elimination of microcirculation disorders and restoration of tissue perfusion.
- Improving the rheological properties of blood.
- Increasing the oxygen capacity of the blood.
- Correction of breathing disorders and elimination of hypoxia.
- Restoration of acid-base and water-electrolyte balance disorders.
- Normalization of blood coagulating properties.
- Maintaining the body's energy balance.
- Symptomatic therapy.
Treatment of blood loss should be early and comprehensive. A plastic catheter must be inserted into the vein; if necessary, 2-3 veins are catheterized. Infusion therapy for acute massive blood loss begins immediately after establishing the fact of blood loss and venous catheterization.
Infusion therapy has the following goals:
- Restoring blood volume, eliminating hypovolemia and ensuring adequate cardiac output.
- Preservation and restoration of the oxygen transport function of blood.
- Ensuring adequate microcirculation.
- Preservation and restoration of normal plasma osmolarity.
- Prevention of aggregation of blood cells and elimination of sludge syndrome.
The problem of adequate media for replacing blood loss has remained the focus of attention of researchers and practitioners for many years. This is due to the fact that neither canned nor fresh blood is not only an ideal, but even an optimal medium for replacing blood loss.
When treating blood loss and hemorrhagic shock, blood transfusion cannot provide full effect for the following reasons:
- The risks associated with blood transfusion may outweigh its therapeutic benefits. The incidence of complications from donor blood transfusion reaches 10%, and death is observed in 0.1-1% of cases.
- Canned blood stored for more than 3 days provides only 50% oxygen transport in the body.
- Up to 25-30% of transfused donor red blood cells and plasma are sequestered from the circulation and deposited in various organs and tissues.
- Regardless of the storage period, up to 30% of preserved red blood cells are found in the blood in the form of aggregates with a size of 40-60 microns and, when transfused, settle in the capillary filter of the vascular system of the lungs (capillary diameter from 8 to 12 microns). This process is the main trigger point in the development of “shock lung” and respiratory failure.
- Blood transfusion for the purpose of correcting anemia does not guarantee improvement and maintenance of adequate blood oxygenation, because Tissue oxygen consumption depends not only on hemoglobin concentration, but also on cardiac output and the difference between hemoglobin oxygen saturation in arterial and venous blood.
- Transfusion of preserved blood can provoke coagulopathy, because Long-term storage of whole blood leads to a decrease in the activity of a number of coagulation factors, platelets and granulocytes (viability 24-48 hours).
- The main cause of hemorrhagic shock is hemodynamic impairment, not anemia.
- Blood transfusions can cause immunosuppressive conditions, which increases the incidence of postoperative infectious complications.
Pathogenetic treatment of acute blood loss and hemorrhagic shock is ensured, first of all, by restoring blood volume, increasing cardiac output and improving microcirculation. One of the fundamental issues in the treatment of hemorrhagic shock is the choice of infusion medium - canned blood or plasma substitutes. To enhance cardiac output, “acellular” fluids (colloid solutions and plasma) were most effective, and red blood cell transfusion was the least successful. In some cases, red blood cell transfusion is accompanied by a decrease in cardiac output, which is associated with an increase in blood viscosity. Blood viscosity also increases when blood flow is low. Consequently, the effect of red blood cell transfusion on circulating blood viscosity will be especially pronounced in patients with low cardiac output. To quickly increase cardiac output and intravascular fluid volume, colloidal solutions are considered favorites. To increase cardiac output, only 1/3 of the volume required for the corresponding effect with crystalloid infusion is required. Crystalloid solutions are preferred if blood loss is not life-threatening.
However, the above is not a call for a complete abandonment of blood transfusion. Blood transfusion should be used with certain restrictions, and remains one of the most important components of the treatment of hemorrhagic shock. After cardiac output is restored, lost hemoglobin must be replaced. The traditional approach to blood transfusion requires increasing the hemoglobin content in the patient's blood to 100 g/L or more. However, this position seems controversial, more like a dogma than a scientifically based fact. This becomes clear if we remember that adequate oxygen supply to tissues depends not only on the concentration of hemoglobin. A more appropriate approach to determine the need for blood transfusion in a particular patient is to monitor tissue oxygen consumption as well as serum lactate concentrations. Base deficiency (BE) can be used as an indirect indicator of serum lactate levels and as a guide for fluid resuscitation. If during infusion therapy BE does not decrease, then this indicates increasing tissue ischemia and the need to continue vigorous treatment (blood transfusions, vaso- and rheologically active substances, etc.).
Clinical experience shows that the need for blood transfusion arises, first of all, with massive blood loss exceeding half or 2/3 of the initial bcc. Blood loss during surgery, not exceeding 1-1.5 liters (20% of the blood volume or less), does not require blood transfusion and can be compensated for by plasma substitutes.
Infusion-transfusion therapy for acute bleeding depends largely not only on the amount of blood loss, but also on its intensity, the degree and stage of hemodynamic disorders, the duration of bleeding, and the patient’s reactivity. Indications for transfusion, as well as the speed, volume, and quality of infusion are determined by the amount of external or internal blood loss, bcc deficiency, hemoglobin and blood hematocrit, by indicators of arterial and central venous pressure, tissue oxygen consumption, lactate and BE concentrations, the symptom of “pale” spots”, hourly diuresis and other signs.
It is very important to clearly articulate what needs to be replenished and then select the appropriate infusion media. If the main goal is to replenish the deficit of bcc, then the most logical choice would be infusion therapy with colloidal solutions. If it is necessary to replenish the loss of interstitial fluid, then administration of crystalloid solutions should be preferred.
The issue of restoring the gas transport function of blood during acute blood loss requires special consideration. Until recently, this problem was solved only by transfusion of canned blood or red blood cells.
Currently, perfluorocarbon emulsions and solutions of modified and recombinant hemoglobin are undergoing clinical trials and being introduced into practice. The last two are still at the stage of clinical trials and we have not found any data on their effectiveness in the treatment of acute blood loss.
At the end of the 70s, the Japanese company “Green Cross Corporation” released the first commercial drug based on perfluorocompounds for clinical trials called “Fluozol DA 20%”. The drug has been used in the clinic since 1978, but had a number of disadvantages, namely: the polydisperse nature of the emulsions, which affects blood microcirculation; high reactogenicity, manifested in activation of complement systems; low stability of the emulsion during storage. In connection with which its clinical trials were terminated.
The most famous among perfluorocarbon emulsions is the drug Perftoran - Russia. Its widespread use in clinical practice as a plasma substitute with a gas transport function has been permitted since 1994. As a carrier of oxygen and carbon dioxide, it is used in surgical hemodilution, plastic surgery on coronary vessels and storage of organs before transplantation.
There is positive experience with the use of Perftoran for blood loss and shock, but all authors are inclined to recommend the use of Perftoran for blood loss of up to 40% of the blood volume, or in combination with blood transfusion, and the volume of blood transfusions when using Perftoran decreased by 1.5 - 2 times.
Conclusion:
Thus, acute blood loss of up to 20% of the volume of blood volume usually does not require blood transfusion and can be compensated for by colloid and crystalloid solutions. If blood loss is 30-40% of the bcc, it is possible to use perftoran in the complex of infusion-transfusion therapy, and in its absence, the introduction of donor red blood cells. In case of extremely severe blood loss (more than 40% of the total blood volume) accompanied by a violation of blood clotting, permeability of the vascular wall, as well as in patients with diseases of the blood system, it is not possible to refuse the use of donor blood and its components.
Question 2.
What dangers to the life and health of the patient are associated with blood transfusion (during transfusion, immediately after it, and in the post-transfusion period), taking into account the standards of its collection, production, transportation, storage and use?
With massive blood transfusions, some adverse reactions can be observed in 10% of recipients. Blood transfusion reactions develop acutely, their frequency is presented in Table 1.
Table 1.
Blood transfusion reactions
| Reaction | Frequency of occurrence | Cause | ||
| Fever | 1:50-1:100 | Antibodies to donor leukocytes | ||
| Hives | 1:100 | Sensitization to donor plasma proteins | ||
| Acute lung injury | 1:5000 | Leicoagglutinins in donor blood | ||
| Acute hemolysis | 1:6000 | ABO antibodies to donor red blood cells | ||
| Fatal hemolysis | 1:100000 | ABO antibodies to donor red blood cells | ||
ACUTE HEMOLYTIC REACTIONS
Serious transfusion reactions are quite rare, but they can be life-threatening. Acute hemolytic reactions are caused by the interaction of the recipient's antibodies with the surface ABO antigens of the donor's erythrocytes. These antibodies bind complement, which can lead to massive hemolysis. A standard package of red blood cells can be completely lysed in less than 1 hour.
Even 10-50 ml of blood transfusion can lead to pronounced hemolytic reactions, and their clinical signs are usually quite characteristic and appear within a few minutes after the start of the blood transfusion.
NON-HEMOLYTIC FEVER REACTIONS
Pyrogenic reactions during blood transfusions occur in 1-4% of cases and are associated with anti-leukocyte antibodies formed in the recipient’s body either during a previous blood transfusion or during pregnancy. This is the most common cause of transfusion fever.
ALLERGIC REACTIONS
Allergic reactions occur in 1-3% of recipients, and their development is associated with sensitization of the body to donor plasma proteins during previous blood transfusions. Patients with immunoglobulin A deficiency are predisposed to allergic reactions of varying severity, even without a history of administration of plasma preparations or plasma proteins.
ACUTE LUNG INJURY
Acute respiratory failure (ARF) is a fairly rare complication of blood transfusion - 1:5000 blood transfusions performed. ARF can be observed even after a single transfusion of both whole blood and red blood cells. Today, the pathogenesis of ARF is associated with the ability of anti-leukocyte antibodies from donor blood to interact with circulating granulocytes of the recipient. The formed leukocyte complexes enter the lungs, where a number of toxic products released by the cells damage the capillary wall, as a result of which its permeability changes and pulmonary edema develops; in this case, the current picture resembles adult respiratory distress syndrome (ARDS). However, ARF is not ARDS (although ARF does occur with it), since the former is almost always resolved safely, and ARDS is accompanied by a very high mortality rate. Currently, the nature of ODN is not fully understood.
Among post-transfusion complications, it should be noted that the recipient is infected with viral infections. Despite the fact that all collected blood in Russia undergoes mandatory testing for the presence of hepatitis B and C viruses, as well as human immunodeficiency virus, any of the test systems used and other methods for determining virus carriage in donors do not provide a 100% guarantee of their detection, which is due to cases of areactive carriage, as well as mutation of viruses that are not recorded by available tests.
The consequences of blood transfusion include immunosuppression.
Conclusion:
Thus, the frequency and severity of complications that arise during and after blood transfusion force a very strict approach to determining the indications for transfusion of canned donor blood and red blood cells.
Continued, questions 3 to 6, read here
Plasma transfusion
Plasma, the liquid part of blood, appears as a clear, yellowish liquid. It contains blood clotting factors - substances that are necessary for the formation of a blood clot and stop bleeding. Plasma also contains substances that protect the body from infection.
Plasma can be stored frozen for up to 12 months. When necessary, it is thawed and the resulting fresh frozen plasma is transfused into the patient.
The main indication for plasma transfusion in cancer patients is increased bleeding. The procedure is also necessary for DIC syndrome (disseminated intravascular coagulation syndrome) - a serious condition in which blood clots form in small vessels, ultimately depleting the entire supply of platelets and coagulation factors, and there is a risk of severe bleeding.
Yours is better than someone else's
Instead of donor blood, the patient can be transfused with his own blood - doctors call this technique autotransfusion. Blood is taken from the patient in advance, two to three days before surgery, and stored under appropriate conditions. In this case, there is no risk of contracting blood infections, an immune reaction to transfusion is eliminated, and there is no risk of complications.
In addition, a little bloodletting before surgery has a good effect on the condition of the body. And a psychologically sick person also has a better attitude towards transfusion of his own blood than someone else’s.
Autotransfusion is especially indicated for those who have a rare blood type, who do not tolerate transfusion well, as well as for those with impaired liver or kidney function. This procedure itself has such a beneficial effect on the body that it is even used as stimulation for athletes before competitions.
In some cases, a whole blood transfusion is not necessary because the body is missing one of its components, such as red blood cells, platelets, or plasma. In these cases, those blood components that are necessary are prepared.
Article on the topic
Promotion of blood donation: plans include new benefits and free parking
Platelet transfusion
Platelets, or blood platelets, take part in the formation of a blood clot and stop bleeding. Their levels may drop due to chemotherapy, radiation therapy, or if the tumor has replaced normal red bone marrow tissue. Platelet transfusions are usually required for cancer patients in one of three cases:
- if the level of platelets in the blood has fallen below a critical value;
- if there is increased bleeding, risk of bleeding;
- if you are undergoing surgery during which significant blood loss is expected.
How is the blood transfusion procedure performed?
Although blood transfusion is formally equated to surgical interventions, this procedure is not at all scary and is practically painless. Blood transfusion is carried out through a needle that is inserted into a vein. It is no more painful than a regular intravenous injection. If the patient already has a central venous catheter, donor blood can be administered through it.
The procedure can take different times, depending on which blood components are transfused: from 30-60 minutes (platelet transfusion) to 2-4 hours (red blood cell transfusion).
How is donor blood tested?
A person who donates blood for the first time must fill out a questionnaire, undergo an examination by a therapist, a dermatovenerologist, and take tests for blood type, Rh factor, and infections: HIV, viral hepatitis B and C, syphilis, cytomegalovirus. Sometimes the examination program can be expanded.
If signs of a particular infection are found in the donor’s blood, it is discarded and not used in the future.
The compatibility of the blood of the donor and the recipient is checked using a special test - a cross-blood compatibility test.
Where do they get the material?
Preparation, separation into components, preservation and preparation of drugs are carried out in special departments and at blood transfusion stations. There are several sources of blood, including:
- Donor. This is the most important source of biomaterial. Any healthy person can become one on a voluntary basis. Donors undergo mandatory testing, during which they are examined for hepatitis, syphilis, and HIV.
- Waste blood. Most often it is obtained from the placenta, namely, it is collected from women in labor immediately after childbirth and ligation of the umbilical cord. It is collected in separate vessels containing a preservative. Drugs are prepared from it: thrombin, protein, fibrinogen, etc. One placenta can produce about 200 ml.
- Corpse blood. Taken from healthy people who died suddenly as a result of an accident. The cause of death can be electric shock, closed injuries, cerebral hemorrhages, heart attacks, and more. Blood is drawn no later than six hours after death. The blood that flows out on its own is collected in containers, adhering to all the rules of asepsis, and used for the preparation of drugs. This way you can get up to 4 liters. At the stations where the preparation is carried out, it is checked for group, rhesus, and the presence of infections.
- Recipient. This is a very important source. On the eve of the operation, blood is taken from the patient, preserved and transfused. It is allowed to use blood that has spilled into the abdominal or pleural cavity during illness or injury. In this case, you don’t have to check it for compatibility, various reactions and complications occur less often, and transfusion is less dangerous.
Are there any alternatives?
Sometimes blood disorders can be corrected with medications. For example, colony-stimulating factors are used to increase the number of white blood cells.
However, in cases where blood transfusion is necessary, there are no alternatives. There are no blood substitutes that can provide similar effects. That is why donation is constantly promoted in all countries of the world, including Russia, and donor days are held periodically. It is important. This helps save the lives of many people.
Compatibility
It is believed that different groups can be compatible if there is no agglutination reaction during transfusion, in which antibodies attack foreign red blood cells and they stick together.
- The first is considered universal, that is, suitable for everyone, since it does not contain antigens. At the same time, people with this group cannot be given any other transfusion, only the first one.
- The second contains antigen A, so it can be transfused to people with II and IV, and to a person with such groups - I and II.
- The third blood contains antigen B. It can be transfused to people with III and IV, and people with this group - I and III.
- The fourth contains both antigens, so it can only be transfused into an IV, but any one is suitable for a person with this group.
As for Rh, it is believed that a Rh-positive person can be transfused with negative blood, but this cannot be done in the reverse order.
All this is true only theoretically, since today it is forbidden to use other blood for transfusion. In emergency cases, the first one can be used as a universal one, but only if it is Rh-negative.
How safe is it?
Can you get an infection from donated blood? Donated blood goes through rigorous testing, but there are still risks, even though they are negligible. Thus, the likelihood of becoming infected with HIV through donated blood is lower than the likelihood of being struck by lightning during a person’s lifetime. The risk of contracting hepatitis C is 1 in 2,000,000. Doctors and scientists are constantly working to reduce the risks to zero.
Can incompatible blood be transfused? Before blood transfusion, the recipient's blood type and Rh factor must be determined; the doctor must make sure that the blood of the donor and recipient are compatible.
But the blood of different people can differ not only in group A0 and Rh factor. It is very difficult to take into account all the nuances. Therefore there is a slight risk of an allergic reaction. Most often it manifests itself in the form of fever, chills, and rash. Such complications are rarely life-threatening. In order to provide assistance to the patient, if necessary, a medical professional is constantly monitoring his condition during the procedure.
An allergic reaction can occur not only immediately during the transfusion, but also within 48 hours after it. You should immediately tell your doctor if your body temperature rises above 38°C, chills, rash, itching, redness of the skin, shortness of breath, difficulty breathing, nausea, lower back pain, blood in the urine, weakness. The most dangerous symptom is chest pain, which requires immediate attention. If you are at home, you should immediately call an ambulance.
Is it possible to refuse a blood transfusion?
The patient always has the right to refuse prescribed treatment, be it chemotherapy, surgery or blood transfusion. But you need to remember some points:
- A doctor will not prescribe a procedure, especially one as serious as a blood transfusion, just like that. If the doctor decides to perform a blood transfusion, then there are good reasons for this, and first of all it is in the interests of the patient.
- Large blood loss during surgery and significant blood disorders can lead to death or serious complications and impair the effectiveness of antitumor treatment.
- There are some risks during blood transfusion, but they are negligible, and the procedure often helps save the patient's life.
Euroonko clinics officially cooperate with the largest blood banks in the country. We operate on the basis of a license for “transfusiology in outpatient and inpatient settings” issued by the health departments of Moscow and St. Petersburg.
Contraindications
Practice has shown that blood transfusion is a very responsible tissue transplant operation with possible tissue rejection and subsequent complications. There is always a risk of disruption of important processes in the body due to blood transfusion, so it is not indicated for everyone. If a patient requires such a procedure, doctors are required to consider contraindications to blood transfusion, which include the following diseases:
- stage III hypertension;
- heart failure caused by cardiosclerosis, heart defects, myocarditis;
- purulent inflammatory processes in the inner lining of the heart;
- circulatory disorders in the brain;
- allergies;
- protein metabolism disorder.
Disposable systems are used for transfusion
In cases of absolute indications for blood transfusion and the presence of contraindications, transfusion is carried out with preventive measures. For example, they use the blood of the patient himself for allergies.
There is a risk of complications after blood transfusion in the following categories of patients:
- women who have suffered miscarriages, difficult births, or given birth to children with jaundice;
- people with malignant tumors;
- patients who have had complications with previous transfusions;
- patients with long-term septic processes.
Price
- Consultation with a transfusiologist - 5100 rub.
- Complete blood count (CITO) - 2400 rub.
- Compatibility test before blood transfusion - 3,200 .
- Erythrocyte suspension, depleted of leukocytes (filtered) - 24,000 rub.
- Transfusion of blood components - 5300 rub.
- The cost of fresh frozen plasma (1 dose 250 ml) is 25,300 rubles.
- Platelet concentrate (1 dose) - 86,100 rub.
In accordance with the legislation of the Russian Federation (Law of the Russian Federation of June 9, 1993 N 5142-I “On the donation of blood and its components”), the procurement of blood, the receipt of blood components and their storage are carried out exclusively by state budgetary institutions. Blood transfusions to our patients are carried out on the basis of licenses for “transfusiology in outpatient and inpatient settings”.
Book a consultation 24 hours a day
+7+7+78