Coma in diabetes mellitus - types, signs, treatment measures, prevention
Diabetes mellitus is one of the most widespread diseases of the endocrine system, characterized by an absolute or relative lack of insulin in the blood.
Despite many years of experience in studying the causes and methods of treating this pathology, diabetes mellitus remains among the diseases whose complications pose a threat to the patient’s life. Despite the indisputable fact that the body of a person with diabetes adapts to small fluctuations in blood glucose levels over time, a rapid decrease or increase in this indicator often contributes to the development of conditions that require emergency intensive care. These are the so-called acute complications of diabetes mellitus - comatose states, which, depending on the mechanism of development and clinical signs, are divided into several types:
- ketoacidotic coma;
- lactic acidemic coma;
- hyperosmolar coma
- hypoglycemic coma;
Types of diabetic coma
Increased attention to the prevention of the development of diabetic comas is due to the high level of complications of these life-threatening conditions. The mortality rate for diabetic ketoacidosis (DKA) in European countries is 2-7%, in the Russian Federation 7-19% [1].
The incidence of DKA in people living with type 1 diabetes mellitus (DM) is 10-100 cases per 1000 cases. About a third of them end up in hospitals in a state of diabetic coma [2]. At the same time, competent glucose-lowering therapy can significantly reduce the likelihood of developing comatose states and delay the development of other serious complications of diabetes [1].
There are 4 types of comas that develop in diabetes:
- Diabetic ketoacidotic. In the medical literature it is also referred to as hyperglycemic hyperketonemic.
- Diabetic non-ketoacidotic hyperosmolar. It is also hyperosmolar non-acidotic.
- Lactic acidosis (lactic acidosis).
- Hypoglycemic coma [2, 3, 7].
Diabetic ketoacidotic coma - causes and mechanism of development, signs
This type of complication develops with an absolute or relative lack of insulin in the body, as well as with impaired tissue utilization of glucose, which develops in patients with severe insulin-dependent diabetes mellitus. The ketoacidotic state develops unexpectedly, but is usually preceded by a number of provoking stress factors, such as an incorrectly selected dose of insulin, a change in drug, cessation of insulin administration for any reason, gross violation of the diet, alcohol abuse, violation of insulin administration technique, increased need for insulin due to the characteristics of the body’s condition (pregnancy, poisoning, surgery, infections, etc.).
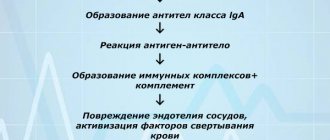
The development of ketoacidosis is due to the fact that with a lack of insulin in the body, the process of penetration of glucose into cells is disrupted, which in turn leads to energy depletion of tissues, contributing to organ dysfunction. Despite compensatory hyperglycemia, which develops due to increased production of adrenocorticotropic, somatotropic and other hormones, as well as increased production of glucose in the liver, due to the lack of a sufficient amount of insulin, glucose cannot penetrate the cellular barrier. In this regard, for compensatory purposes to maintain homeostasis, the body begins to receive the missing energy through the active breakdown of fats - lipolysis, and as a result of this biochemical process, ketone bodies (acetone) are formed, an excess amount of which has a depressing effect on the central nervous system, as a result of which ketoacidosis develops coma.
The concentration of ketone bodies in the blood of healthy people is in the range of up to 100 µmol/l, while only traces of acetone can be found in the urine. If the course of diabetes mellitus enters the stage of decompensation, a large number of ketone bodies are formed in the liver due to metabolic changes (up to 1000 mmol/l per day). This amount of ketone bodies cannot be eliminated from the body by muscles and kidneys, so their accumulation leads to ketoacidosis. The condition is aggravated by the formation of a vicious circle, when as a result of the development of ketoacidosis in the blood there is a decrease in the level of immunoreactive insulin, the relative or absolute deficiency of insulin only increases.
The development of ketoacidotic coma is usually slow - from several days to several weeks. If the process develops against the background of acute infectious diseases or severe intoxication, a diabetic coma can develop within a few hours. As a rule, clinically diabetic ketoacidosis goes through three stages, which, in the absence of timely correction, follow one after another.
1. Stage of moderate ketoacidosis
- the patient may complain of general weakness, increased fatigue, tinnitus, lethargy, decreased appetite, thirst, nausea, acute abdominal pain, increased volume of urine excreted. Exhaled air and urine smell like acetone. An increase in sugar levels is detected in the blood and urine.
2. Precoma stage
or
decompensated ketoacidosis
- the patient’s appetite disappears completely, in addition to nausea, vomiting is observed, which increases general weakness. The patient is indifferent to what is happening around him, his vision deteriorates, shortness of breath, pain in the heart and abdomen appears. Against the background of an indomitable feeling of thirst, there is an increase in the urge to urinate, which is explained by a violation of the water-electrolyte balance and excessive removal of electrolytes from the body - potassium, sodium ions, etc. The patients' consciousness is preserved, as is their orientation in space and time, but inhibition is noted when trying to answer questions. The skin is dry, rough, cold. The cheeks are slightly flushed, and the tongue is covered with a brown coating; teeth marks may be visible on it. This stage can last from several hours to several days. In the absence of timely correction of this condition, a deterioration in the patient’s reaction and the transition of the process to the final stage is observed.
3. Stage of coma - the patient is absolutely indifferent and may fall into deep sleep. Upon examination, deep, noisy breathing with a pungent odor of acetone in the exhaled air, decreased blood pressure, and a rapid rhythmic pulse are revealed. Tendon reflexes gradually fade away. There is a decrease in body temperature.
If the development of ketoacidotic coma is suspected, the patient should be immediately hospitalized in order to carry out the necessary set of resuscitation measures.
Lactacidemic
Lactic acid coma is also called lactic acid coma and develops more often than other types of emergency conditions in diabetes. Lactic acid coma is the most dangerous acute condition, with mortality reaching 75%. This condition can develop against the background of provoking conditions:
- Massive bleeding;
- Myocardial infarction;
- Generalized infectious process;
- Heavy physical activity;
- Kidney or liver failure.
As a result of lactic acidemia, ketone bodies and pyruvic acid are broken down in the blood with the formation of an increase in the concentration of lactate and a decrease in pyruvate - chemicals that shift the acid-base balance of the blood to the acidic side. In 30% of victims, hyperosmolar coma is initially noted.
Clinical picture
The condition of patients is rapidly deteriorating, and negative dynamics are observed. The onset is usually sudden, with severe development of symptoms. Diabetics note:
- Severe muscle pain and weakness;
- Drowsiness or, conversely, insomnia;
- Severe shortness of breath;
- Abdominal pain with vomiting.
With further deterioration of the condition, convulsions or areflexia associated with muscle paresis may occur. These symptoms arise as a result of brain damage due to energy deficiency and disturbances in the ionic composition of the plasma. Even with proper and timely treatment, the prognosis for a victim of lactic acidemia coma is unfavorable.
Lactic acidotic coma - development mechanism and symptoms
This type of diabetic coma is less common than other types, but is one of the most severe complications of diabetes. This type of coma develops as a result of a complex biochemical reaction - anaerobic glycolysis, which is one of the alternative methods of producing energy, the residual product of which is lactic acid. If in a healthy body the level of lactic acid is in the range of 0.5 - 1.4 mmol/l, then in lactic acidotic coma this figure reaches 2 mmol/l when the blood pH level drops below 7.3. In addition, there is a change in the lactate-pyruvate balance towards an increase in lactate concentration.
Lactic acidotic coma often develops against the background of shock, intoxication, sepsis, extensive blood loss, cardiovascular and renal failure. Despite the fact that the liver is normally capable of processing more than 3 thousand mmol of lactic acid, due to the state of tissue hypoxia that accompanies the above pathological processes, the ability to process lactic acid becomes significantly less than the lactate formed. If patients are given intravenous solutions containing xylitol, sorbitol, fructose and other sugars, this is also a provoking moment for the development of lactic acidotic coma.
The onset of this type of coma is usually sudden, characterized by signs of depression of consciousness (apathy, drowsiness, delirium), as well as rapid loss of appetite, nausea, vomiting, and muscle pain. Upon examination, the patient's skin is pale and cold. The effect of lactic acid on the cardiovascular system is manifested by increased heart rate, decreased blood pressure, impaired excitability and contractility of the myocardium, paresis of peripheral vessels, and collapse.
Patients with the first signs of coma need prompt hospitalization. Confirmation of the diagnosis of lactic acidotic coma is carried out based on laboratory data, namely a high concentration of lactic acid and pyruvate in the blood, as well as a violation of the acid-base balance towards acidification.
Forecast
The prognosis for a comatose state depends on the cause, as well as the degree of depression of consciousness and the duration of its depression. In case of precoma or the presence of stage I coma, a favorable prognosis is noted. In the case of coma II and III degrees, the prognosis is questionable, but there is hope for recovery. If we consider a IV degree coma, it most often ends in death. A deep coma lasting more than 24 hours has a poor outcome. If reflexes are absent for less than 6 hours, the prognosis is relatively favorable.
Favorable prognostic factors are:
- Early return of speech.
- Spontaneous eye movements.
- Preserved muscle tone at rest.
- Ability to execute commands.
The prognosis is unfavorable if patients, after circulatory arrest, experience:
- Myoclonic status epilepticus .
- Lack of pupil reaction for 24-72 hours.
- Absence of corneal reflexes.
- No response to pain within 72 hours.
In uremic coma, all reflexes and motor reactions may be lost, but recovery after treatment is complete. If hypothyroid coma , death occurs in 60-90%.
If a patient develops a hepatic coma against the background of chronic liver pathology, then every fifth person does not come out of it and death occurs after 1-3 days. How long do people live in a hepatic coma after they come out of it? This period depends on many factors, but most often the life span does not exceed several months, provided that the patient is constantly supported by liver function. Life extension is possible through organ transplantation - patients live from 5 to 10 years. Coma with fulminant hepatitis ends in death in 85% of patients. Patients with liver failure live for 3 months.
Hyperosmolar coma - prerequisites for development, clinical manifestations
Hyperosmolar coma usually develops in patients suffering from mild to moderate non-insulin-dependent diabetes mellitus, who are treated with diet therapy and medications that lower blood sugar levels. This complication often develops in elderly patients with limited mobility, as well as with concomitant pathological processes such as burns, hypothermia, infectious diseases of the kidneys and urinary tract, lungs, pancreas, myocardial infarction, etc., which aggravate the process of impaired blood supply. With a high concentration of sugar in the blood, there is an increase in the excretion of urine from the body by the kidneys, resulting in dehydration, which in turn leads to thickening of the blood and difficulty in its movement through small vessels. The consequence of such microcirculatory disorders is a deficiency of cerebral blood supply.
The development of hyperosmolar coma is extended over time. The first signs are a constant feeling of thirst, increased volume of urine, and general weakness. Increasing dehydration leads to lethargy and clouding of consciousness, hallucinations, convulsions, paresis of the arms and legs. At the first signs of an impending complication, patients should be hospitalized in order to immediately restore water-salt metabolism through the administration of infusion solutions.
List of sources
- Efimov A. S., Komissarenko I. V., Skrobonskaya N.A. Emergency endocrinology. – M.: Medicine, 1982, – 208 p.
- Balabolkin M.I., Lukyanchikov V.S. Clinic and therapy of critical conditions in endocrinology. – Kyiv: Health, 1982, – 152 p.
- Kurek, V.V. Guide to emergency conditions in children / V.V. Kurek, A.E. Kulagin. 2nd ed. Moscow: Med. lit., 2012, - 464 p.
- Sumin, S. A. Anesthesiology, resuscitation, intensive care: textbook. for students of institutions of higher professional education / S. A. Sumin, I. I. Dolgina. Moscow: Medical Information Agency, 2015, 496 p.
- Krylov, V.V. Neuroreanimatology. Practical guide / V. V. Krylov, S. S. Petrikov. Moscow: GEOTAR-Media, 2010, - 176 p.
Hypoglycemic coma - causes, symptoms
This complication of diabetes mellitus develops due to a rapid decrease in blood glucose levels, which can be caused by an overdose of insulin or other drugs that lower sugar levels, or excessive physical activity, leading to a sharp consumption of glucose. If the patient does not eat after an insulin injection, this can also cause hypoglycemia.
The development of hypoglycemic coma is always sudden. Harbingers of an impending coma are increased anxiety, trembling, sweating, flashing “spots” before the eyes, a feeling of numbness of the tongue and lips, and a sharp feeling of hunger. In the absence of correction of the condition at this stage, the patient experiences the appearance of convulsions, agitation, and increased blood pressure. In the future, depression of consciousness, increased sweating, slowing of breathing and gradual disappearance of reflexes can be observed.
First aid
Correction of the patient's condition is carried out in a medical institution. People with moderate ketoacidosis are hospitalized in the therapeutic/endocrinology department, and in a state of precoma and coma - in the intensive care unit [4].
At home you can:
- conduct a rapid glycemic analysis if you have a glucometer;
- call an ambulance.
A person with ketoacidosis can be given 20 units intramuscularly. short-acting insulin (RAI) [4]. With moderate hypoglycemia, the patient needs to take easily digestible carbohydrates (sugar dissolved in tea, water, a piece of bread) [3].
In the emergency department, a urine test for ketone bodies is additionally performed and infusion therapy begins with the introduction of a 0.9% NaCl solution at a rate of 1 l/h [4].
Laboratory diagnostics
When diagnosing, in addition to the obvious symptoms, it is necessary to differentiate the type of diabetic complication. To do this, a number of rapid blood tests are performed:
- for sugar;
- for the presence of acetone bodies (ketones);
- arterial pH;
- on lactate concentration;
- for sodium and potassium content.
Water homeostasis (blood plasma osmolarity), the level of fatty acids, and the presence of acetone in the urine are determined. Glucose levels in the patient's precomatous and comatose state always exceed 30 mmol/liter. The presence of sugar in the urine is detected. With ketoacidosis, acetone bodies are detected in the blood. Hyperosmolar coma is characterized by a significant increase in plasma osmolarity. In lactic acidosis, excessively high levels of lactate are detected.
Features of the course in childhood
Hyperglycemic coma in children occurs for the same reasons as in adults, but there are several additional factors. These include mental and hormonal instability. These features often become the causes of the development of a serious condition in diabetes mellitus. Hyperglycemic coma requires immediate medical attention, as its course in children often ends in death. More often, ketoacidotic coma is diagnosed in young patients, in which it is necessary to provide the patient with emergency care in a hospital setting. If left untreated, the consequences can be very serious.
It is important to promptly pay attention to signs of hyperglycemia in a child, this will help prevent the onset of coma.
Signs of the disease in children are similar to those in adults, but we must not forget that the child cannot independently assess his condition, so parents must carefully monitor the baby’s well-being.