At the first visit and for certain indications, a pediatric cardiologist in Saratov will be able to determine whether the child has bradycardia. The main feature of the disease is a decrease in the working pulse rate, which can be expressed to varying degrees. It is extremely important for parents to show their child to a specialist at the First Children’s Medical Center on time, undergo the necessary examinations in pediatric cardiology in Saratov, take tests and, based on their results, receive a doctor’s conclusion and recommendations.
Types of arrhythmia in children
Taking into account the characteristics of heart rhythm deviations, childhood arrhythmia is divided into four key types:
- Tachycardia. Accompanied by increased rhythm. The heart rate normally increases with physical activity, elevated temperature, and stress. But if such a condition does not depend on external factors, it is considered a pathology. Tachycardia indicates a malfunction of the heart muscle and leads to its rapid wear.
- Bradycardia. Characterized by a rhythm that is too slow. The contraction frequency decreases to 30-50 beats per minute. Pathological bradycardia may not interfere with circulation and cause no symptoms. But if the rhythm drops below 40 beats per minute, the baby experiences fainting, chronic weakness and dizziness.
- Extrasystole. It is distinguished by the presence of contractions outside the rhythm. It occurs when an extraordinary impulse appears between normal heart contractions - an extrasystole. Extrasystoles can be multiple or single, appear according to a certain rhythm or randomly. Rare single extrasystoles are not dangerous and do not require treatment. However, with frequent group extraordinary impulses, diagnosis and treatment of the pathology is necessary.
- Atrial fibrillation . Random rapid contraction of different parts of the atria, which causes an acceleration of the pulse. This type of arrhythmia occurs most often in childhood. The pathology is quite dangerous and, if left untreated, causes heart failure.
Expert advice
If your child suffers from any cardiac disease and is prescribed drugs such as beta-blockers (Bisoprolol, Metoprolol) and calcium channel blockers (Verapamil, Diltiazem) for treatment, you need to remember that the pulse may slow down while taking them. A decrease in heart rate by approximately 5-10 beats from the lower limit of the age norm is not dangerous. But, if the child’s heart rate decreases more, the cardiologist must be informed about this so that he can adjust the dosage.
Symptoms of cardiac arrhythmia in a child
The symptoms of heart rhythm disturbances have different specifics and differ in children of different age groups.
Arrhythmia in a newborn baby can manifest itself through:
- pale, bluish skin;
- baby anxiety for no apparent reason;
- refusal to eat, breastfeed, or bottle;
- shortness of breath;
- slight or no weight gain;
- problems sleeping, crying.
Arrhythmia in a child aged 6 years and older very often has no symptoms. In such cases, pathology is detected during a routine medical examination. Only sometimes do children exhibit characteristic symptoms of the disease:
- excessive fatigue;
- poor body response to physical activity;
- causeless fainting, dizziness;
- pale skin;
- apathy or increased excitability;
- poor appetite;
- pain in the heart area.
Causes of arrhythmia in children
Children's nervous, autonomic and immune systems have not yet entered a stable stage of maturity. It takes years before the sinus node, which is responsible for normal rhythm, begins to generate the correct electrical impulses for the rhythmic contraction of the heart chambers. Only in adolescents the heart begins to beat at the same rhythm as in adults - 60-80 beats per minute.
The most common causes of cardiac arrhythmia in children are:
- heart defects and anomalies (congenital or acquired);
- inflammatory cardiopathologies (myocarditis, endocarditis, etc.);
- severe course of infectious or viral diseases and their complications (angina, hepatitis, diphtheria, intoxication, pneumonia, typhoid fever);
- arterial hypertension;
- failures of nervous regulation of rhythm (vegetative-vascular dystonia);
- mitral valve prolapse;
- pathologies of the central nervous system;
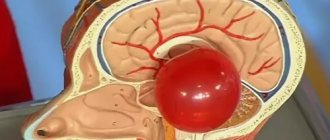
- malignant diseases of the brain;
- hyperfunction of the thyroid gland;
- anemia;
- hereditary diseases;
- difficult course of labor, prematurity;
- rapid development of the child’s body, in which the cardiovascular system does not keep pace with the growth of bone and muscle structures Source: Skudarnov E.V., Baranova N.V., Antropov D.A., Dorokhov N.A. Structure and etiological factors of cardiac arrhythmias in newborns Russian Bulletin of Perinatology and Pediatrics No. 3, 2021, p. 183.
Varieties
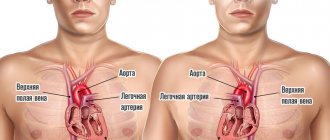
Depending on the location, bradycardia can be sinus and observed with heart block.
What is sinus bradycardia? This is a pathology caused by a disruption in the production of bioelectric impulses in the sinus node.
Heart blocks that may cause bradycardia:
- sinoatrial – with it there is a failure in the conduction of bioelectric impulses from the sinus node to the atria;
- atrioventricular - in this case, their conduction between the atria and ventricles is disrupted.
Blockades that cause bradycardia are encountered regularly in cardiologist practice.
Bradycardia is also distinguished:
- physiological - it is observed in trained endurance athletes, during sleep, as well as in ordinary people at rest;
- pathological - this type of bradycardia occurs in various nosologies.
Pathological bradycardia occurs:
- acute;
- chronic.
The acute form of the described pathology develops against the background of serious pathologies. In this case, the question of which tablets are prescribed for symptoms of bradycardia is inappropriate, since these critical pathologies should be eliminated:
- myocardial infarction;
- various types of myocarditis;
- intoxication – poisoning with biological and synthetic poisons.
An illustrative example of chronic bradycardia is involutive, or age-related, sclerotic changes in heart tissue.
Also, depending on the causes of development, the following forms of bradycardia are distinguished:
- extracardiac;
- organic – it occurs with various lesions of the heart structures;
- medicinal (medicines for bradycardia in this case should be selected carefully);
- toxic – caused by various toxic substances (organic or synthetic);
- sinus bradycardia in athletes.
Another division of bradycardia according to etiological factor is also practiced - it happens:
- toxic;
- central;
- degenerative – caused by the “degeneration” of tissues;
- idiopathic - its causes have not been established.
How dangerous is the disease?
In most cases, cardiac arrhythmia in a child has a favorable prognosis and is benign. However, for any form of the disease, it is extremely important to monitor the baby’s health, regularly conduct preventive examinations and, according to the doctor’s decision, undergo treatment.
In the absence of competent and timely treatment, the pathology can cause serious complications in the future. The long course of the disease has a detrimental effect on the functioning of the heart and leads to dangerous consequences.
Arrhythmia can cause heart failure and cardiomyopathy, which carry the risk of early disability and even death. Increases the risk of developing arterial hypotension and myocardial ischemia. A prolonged attack of tachycardia can provoke cardiogenic shock or acute heart failure with pulmonary edema.
In addition, the long-term chronic course of the pathology significantly worsens the child’s well-being. The quality of life is gradually decreasing, and constant fatigue and apathy only increase over the years Source: Dubovaya A.V. Modern approaches to assessing the quality of life of children with arrhythmias Russian Bulletin of Perinatology and Pediatrics, 2016; 61:5, pp. 75-81.
Prevention
Preventive measures will help reduce the symptoms of heart disease. The basis of prevention is adherence to a diet , which includes the following nuances:
- increase the volume of fluid consumed;
- include more fresh vegetables in your baby’s menu, especially carrots, cabbage, and parsley;
- When it comes to meat products, give preference to low-fat varieties;
- include in the menu fruits that are useful for normalizing heart function - apples, persimmons, bananas, all types of citrus fruits;
- consume dairy and fermented milk products daily;
- Prepare seafood dishes 1-2 times a week.
In addition to diet, hardening and moderate physical activity are recommended. It is necessary to determine the type of sport, as well as the method of hardening, only after consultation with a cardiologist.
Diagnostics
Doctors identify several acute time periods when the possibility of developing pathology becomes especially acute. Often, arrhythmia in a child develops in infancy, at 4-5 years, at 7-8 years, at 11-12 years and in adolescence. Growth spurts occur during these age intervals. Therefore, carrying out preventive diagnostics and cardiac examination at this time is of particular importance, even if the symptoms of the disease do not manifest themselves.
Only a pediatric cardiologist or arrhythmologist can identify the deviation and establish a diagnosis. Initially, you should consult with a specialized specialist who:
- will study the medical history of a small patient;
- will conduct a full examination, palpation, percussion and auscultation;
- will prescribe the necessary laboratory and instrumental diagnostics.
To identify the disease and record the diagnosis, the doctor prescribes:
- Electrocardiography (ECG) is a method of studying the heart that allows you to record the electrical activity of the heart. With its help, the doctor identifies rhythm deviations and determines the frequency of muscle contraction.
- Daily ECG monitoring is a study of cardiac activity that takes place throughout the day. Compared to ECG, this method is more accurate. Allows you to record the dynamics of the rhythm during different periods of the child’s life: activity and sleep.
- Stress tests – analysis of heart activity during physical activity of varying intensity. Prescribed for suspected cardiac arrhythmia in a child 3 years of age or older.
The diagnostic results allow the cardiologist to diagnose the disease. Additionally, the doctor can prescribe procedures that will help identify the causes of the pathology:
- Echocardiography (EchoCG) is the study of the heart using ultrasound. With its help, you can detect the organic prerequisites for the development of arrhythmia: defects, neoplasms, etc.
- Electroencephalography (EEG) is the study of the electrical activity of the brain. It is prescribed if there is a suspicion of a connection between the pathology and abnormalities in the functioning of the brain.
- Radiography is a study using x-rays. Allows you to detect the preconditions for arrhythmia that are not directly related to the work of the heart: diseases of large vessels, pathologies of the spine, etc.
Which sport is suitable
Moderate physical activity is what has a beneficial effect on children diagnosed with bradycardia. They will benefit from long leisurely walks in the fresh air, morning exercises and water treatments. Sports should be low-energy and calm.
If your child wants to play big sports, encourage him to look at the following types:
- Swimming will strengthen the heart muscle and increase endurance. Due to the horizontal position of the swimmer, it will improve the pushing of blood through the arteries.
- Golf has a beneficial effect not only on the body, but also on the intellect. It does not require explosive, static or vigorous exercises. Competitions and training take place outdoors, and golfers travel a lot on foot. Almost ideal sport for bradycardia.
- Race walking. Like golf, most of your training takes place outdoors. In this case, there is no heavy load on the heart as with fast running.
- Volleyball. It will not only strengthen the body, but also improve blood circulation.
- Rowing. During rowing, the concentration of oxygen in the blood increases. In addition, it has been noticed that the rowing technique is somewhat reminiscent of a pacemaker. Therefore, this sport has a beneficial effect on the heart.
- Classic cross-country skiing. The principle of aerobic exercise, which enriches the blood with oxygen, also applies here. Considering that training takes place in the fresh air. The efficiency of classic cross-country skiing increases significantly.
Thus, it is best for children with bradycardia to engage in sports that do not put too much strain on the heart, enrich the blood with oxygen, and take place in the fresh air.
Treatment of cardiac arrhythmia in children
After completing the examination, the doctor examines the results of diagnostic procedures and makes a diagnosis. Only after this, the specialist develops an individual treatment plan, taking into account the type and degree of development of the disease, its duration, the presence or absence of concomitant pathologies, the cause of the development of arrhythmia, the age and general health of the patient, as well as many other factors.
Complex treatment of arrhythmia in children involves taking drugs with a different spectrum of action: vascular, neurometabolic, antiarrhythmic. Antioxidants and cell membrane stabilizers are also used. The doctor determines the type of medication, dosage and duration of use individually.
In addition to drug therapy, preventive measures are also prescribed. Parents receive recommendations that will help speed up recovery and stabilize the child’s cardiovascular system:
- reduction of stress, emotional changes;
- healthy sleep and daytime rest;
- proper diet, which excludes fatty foods;
- normalization and maintenance of healthy body weight;
- monitoring cholesterol and blood glucose levels;
- regular preventive examination Source: Balykova L.A., Nazarova I.S., Tishina A.N. Treatment of cardiac arrhythmias in children Practical Medicine No. 5 (53), September 2011, pp. 30-37. .
Treatment of children's ari
Our medical centers provide comprehensive diagnostics and treatment of cardiovascular pathologies in young patients. By contacting SM-Clinic, you can be sure that:
- the child will be treated by qualified cardiologists;
- if necessary, related specialists will be involved in the therapeutic process, who will provide an integrated approach;
- the baby will be examined in a modern diagnostic center with advanced equipment that provides highly accurate results and eliminates the possibility of receiving erroneous data;
- consultations and other procedures will take place at a clearly appointed time, without queues or tedious waiting.
Sign up for a consultation by phone or fill out the feedback form, and we will contact you to confirm your appointment.
Sources:
- Balykova L.A., Nazarova I.S., Tishina A.N. Treatment of cardiac arrhythmias in children. Practical Medicine No. 5 (53), September 2011, pp. 30-37.
- Pavlova N.P., Maksimtseva E.A., Artemova N.M. Arrhythmias in children. Cardiovascular therapy and prevention No. 18, 2021, pp. 118-119
- Dubovaya A.V. Modern approaches to assessing the quality of life of children with arrhythmias. Russian Bulletin of Perinatology and Pediatrics, 2016; 61:5, pp. 75-81
- Skudarnov E.V., Baranova N.V., Antropov D.A., Dorokhov N.A. Structure and etiological factors of cardiac arrhythmias in newborns. Russian Bulletin of Perinatology and Pediatrics No. 3, 2021, p. 183