The vessels of the brain form a complex circulatory system, which must ensure constant delivery of nutrients and oxygen to nerve cells.
The circle of Willis is a closed complex of arteries that provides blood supply to the structures of the central nervous system due to the redistribution of blood.
Pathologies in its structure and function lead to various neurological disorders. We will talk further about what the Circle of Willis is and what it means if it is open.
About the Circle of Willis of the brain
The circle of Willis protects the brain from hypoxia when blood flow through the arteries is impaired. Redistribution of blood helps prevent the death of neurons due to thrombosis, compression or rupture of blood vessels.
A closed circle system with anastomoses ensures normal blood flow due to the blood that flows through the vessels of the opposite side. An anastomosis is a small artery that connects two areas of the nervous system with separate blood supplies.
Anatomical structure
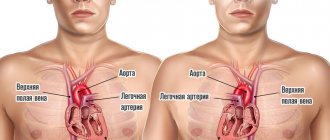
The vessels of the circle are located under the arachnoid membrane in the area of the optic chiasm at the base of the brain. In most people, several vessels are involved in the formation of the arterial circle:
- anterior communicating artery;
- posterior communicating arteries;
- left and right anterior cerebral arteries;
- left and right posterior cerebral arteries;
- supracuneiform part of the internal carotid artery.
All arteries connect with each other, forming a vascular heptagon. Due to this, anastomoses are formed between the carotid and basilar arteries. This makes it possible to prevent ischemic brain damage due to unilateral disturbances of blood flow through the vessels.
Functions
The main function of the arterial circle is to ensure normal blood supply to the brain in case of pathology of individual vessels. This is achieved due to its closed structure and constant blood flow through several arteries.
Causes of the disease
The consequences are varied: from developmental delays to migraines. It is difficult to diagnose the pathology, so the disease can proceed for quite a long time without a clear diagnosis. One of the deviations is the classic structure of a circle, but the vessels are of different diameters. This asymmetry leads to headaches.
The most common pathologies of the circle of Willis are:
- Vascular hypoplasia. This pathology is associated with a reduced diameter of blood vessels. Due to the small size of the arteries, blood flows through them more slowly and in smaller quantities. In the absence of disturbances in other vessels of the brain, this pathology can remain undetected for a long time. However, if there are deviations in the blood supply to the brain, the main function of the Circle of Willis – additional nutrition – will be disrupted. It is very easy to detect hypoplasia using MRI.
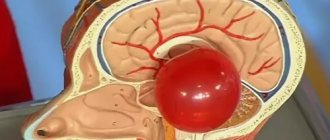
- Aneurysm of a cerebral vessel. This can affect any vessel in the brain. An aneurysm is a bulge and thinning of the wall of a vessel or artery. The patient does not feel any discomfort until the aneurysm ruptures and leads to hemorrhage, which is accompanied by severe headaches and nausea. This condition is life-threatening and requires immediate medical attention.
- Vascular aplasia. This is the absence of any part of the Circle of Willis. This anomaly develops in the womb. It is difficult to determine how dangerous it is. The consequences depend on which part is missing, whether there are other violations, etc.
- Trifurcation of the artery. Splitting of the artery into 3 branches is observed quite often. As a rule, this condition is not life-threatening and does not lead to any negative consequences.
Not all pathologies require treatment; sometimes it is enough to observe and adhere to the rules of prevention in order not to encounter complications.
Symptoms of pathologies can be different: headaches, dizziness, nausea, fear of bright light, decreased memory and attention; children may experience delayed intellectual development.
The most common variant of the development of the circle of Willis is considered to be posterior trifurcation of the ICA, which accounts for almost a fifth of all anomalies of the arterial ring. With this type of structure, three cerebral arteries immediately begin from the ICA - anterior, middle and posterior, and the PCA will be a continuation of the posterior communicating branch.
A similar structure is typical for the circulatory system of the fetal brain at 16 weeks of pregnancy, but later the sizes of the vessels change, the posterior connective branch decreases, and the remaining branches increase significantly. If such a transformation of the vessels does not occur, then the child is subsequently born with posterior trifurcation.
Another common variant of the structure of the circle of Willis is considered to be aplasia of the PCA, which occurs under various unfavorable external conditions and genetic abnormalities during embryogenesis. In the absence of this artery, the circle of Willis does not close on the side where it is not present, that is, there is no relationship between the internal carotid artery system and the basilar area.
What pathologies are possible
The circle of Willis has a complex structure and consists of 10-12 arteries. Therefore, some people may have diseases associated with vascular damage. They are divided into two groups: congenital, which arose during intrauterine development of the fetus, and acquired, developing after birth. The most common pathologies are:
- Aneurysm is a local protrusion of the arterial wall outward. A person can go for a long time without any symptoms, which makes timely diagnosis difficult. If blood pressure increases, the aneurysm may rupture. In this case, an intracranial hematoma develops. The patient complains of headache, nausea, vomiting and dizziness. He experiences neurological disorders, including severe paralysis or death. Aneurysms can be located on any vessel;
- hypoplasia is characterized by underdevelopment of the artery with a decrease in its diameter and lumen. This leads to insufficient blood flow. If the circle is closed, then the disease is asymptomatic, since blood flows to the brain through other vessels;
- aplasia is complete underdevelopment of the artery. Can be observed in any vessel. Aplasia of the anterior or posterior communicating artery leads to the fact that the circle of Willis becomes open. This is fraught with the development of cerebral ischemia against the background of concomitant pathologies: atherosclerosis, aneurysms, thrombosis, etc.;
- trifurcation of the carotid artery with its splitting into three vessels. The condition is not manifested by any diseases, however, if the patency of the artery is impaired, cerebral ischemia is possible.
Pathological structure of the arterial basilar circle
The vessels of the anterior half (carotid and anterior cerebral) are distinguished by the greatest stability of development, while the anatomy of the posterior cerebral and connecting parts is characterized by great variability in branching.
However, deviations in the structure of the anterior half are much more important due to the significant severity of clinical symptoms and the greater severity of the prognosis. In addition to the ideal (closed) there are options for the open basilar circle:
- fully;
- not completely.
In the first case (in the absence of connecting branches), the communication between the anterior and posterior sections is completely absent; in the second (with their preservation, but in a state of stenosis or hypoplasia), they speak of incomplete opening of the basilar circle, allowing it to function not at full capacity.
Signs of structural anomalies
Anomalies in the structure of blood vessels may not manifest themselves for years, until reaching an age when the changes become stable and the level of cerebral circulation becomes unstable, but they can appear already in young years.
The most constant ones include the appearance of:
- headaches;
- dizziness;
- decreased attention, memory (in severe cases, intellectual capabilities).
Due to the presence of cerebral ischemia involving fine brain structures, both neurological and mental abnormalities appear - from emotional instability to neuroses and panic attacks.
The most characteristic symptom of circle of Willis pathology is migraine attacks. The most susceptible to it are people with open circles or anomalies in the development of the posterior half of the system:
- posterior trifurcation;
- hypo- or aplasia of the posterior communicating branches.
Due to ischemia of the areas of the brain responsible for vision, the onset of an attack is preceded by the appearance of a visual aura (bright zigzags, flashes and sparks in the eyes).
Other symptoms of insufficient blood supply are signs of DEP (dyscirculatory encephalopathy) with a disorder in both the emotional-volitional and purely physical spheres - from unreasonable weakness to decreased ability to work.
The peak of dysfunction in the abnormal structure of the basal circle is the development of stroke with the development of paralysis and paresis, sensory and motor disorders, and in severe cases - with the onset of coma.
The emergence and development of an aneurysm may also not manifest itself for decades and is often an accidental finding during the study of cerebral vessels.
About the causes of pathologies
Deviations in the development of structures of the circle of Willis occur, as a rule, during intrauterine development, the course of which can be caused by abuse on the part of the pregnant mother:
- her smoking;
- her use of alcohol or drugs;
- overdose of sleeping pills and sedatives;
- unauthorized use of medications not prescribed by a doctor.
The course of pregnancy can be affected by chronic or acute stress of high intensity, viral infection, etc.
The cessation of the functioning of the existing and developed system of messages at the base of the brain can be caused by both the same chronic household intoxications and changes in the properties of blood (due to its high coagulability), as well as diseases that cause degeneration of the vascular wall or narrowing (closing) of the lumen of blood vessels:
- atherosclerosis;
- thrombosis;
- fat or air embolism when large arteries are injured by sharp edges of bones during their fracture, or other acute and chronic causes.
Is an open circle of Willis good or bad?
The structure of the arterial circle has many variations. Normally, it is closed, which helps protect nervous tissue from ischemia and damage.
In some people, the circle of Willis is not closed on the side of the anterior or posterior communicating artery. This condition is not always regarded by doctors as a pathology.
An open arterial circle is bad. In the absence of all anastomoses, a person has an increased risk of developing ischemia of nervous tissue against the background of atherosclerosis, thrombosis and arterial embolism.
However, the condition itself does not require treatment, since pathologies arise only against the background of concomitant diseases of the cardiovascular system.
Clinical manifestations
Violations of the structure of the circle and its openness lead to disruption of the blood supply to the brain. Depending on where ischemia develops, a person may develop different symptoms. The first symptoms are often:
- dizziness that occurs during severe physical or emotional stress;
- severe headache that does not disappear when taking painkillers;
- migraine attacks with nausea, vomiting, and fear of loud sounds and lights.
As anemia progresses, neurological disorders occur. The patient may complain of impaired sensitivity on the skin, decreased muscle strength or complete absence of movements in the arm or leg, frequent dizziness, etc. Cognitive functions are also impaired: the ability to remember information decreases, the patient takes a long time to make decisions, forgets the way home, etc. With ischemia frontal cortex, speech is impaired. The patient cannot speak clearly or does not perceive the speech of other people.
Symptoms of disease
The signs of this pathology are similar to other diseases, so the doctor must rule them all out before making a diagnosis. The specialist must study the symptoms in detail and prescribe certain examinations.
Most often, magnetic resonance imaging is used to accurately diagnose such symptoms. in some cases, ultrasound of the vertebral arteries is prescribed. With the help of these studies, the condition of the brain vessels is determined.
Not in all cases, people suffering from this disease need treatment. In most people, the body independently compensates for the disruption of this artery at the expense of other, smaller ones. Thanks to this property of the body, a person can feel great and not suspect that he has health problems.
In mild cases, certain measures need to be taken to alleviate the harm to the body that a disease such as hypoplasia of the left vertebral artery can cause. Treatment consists of prescribing drugs to dilate blood vessels. They can to some extent reduce blood pressure and normalize blood circulation in narrowed vessels.
The use of vasodilators may cause chest pain, nausea, vomiting, nasal congestion, and severe dizziness. The amount of hair on the body may increase.
Diagnostic measures
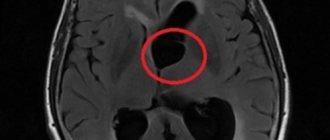
Detection of an open arterial circle requires instrumental studies: angiography, Dopplerography, computed tomography or magnetic resonance imaging.
These methods allow you to visually assess the condition of the arterial vessels and identify their pathological changes. Only the attending physician should interpret the examination results.
Angiography
“Gold standard” for examination of cerebral vessels. Angiography allows you to assess the condition of blood vessels, detect aneurysms, narrowings and complete blockage of the lumen. The principle of the method is similar to radiographic studies. Radiocontrast agents are used only to identify blood vessels on images.
They are inserted through a small catheter into the artery. Contrast agents circulate along with the blood and are clearly visible on the resulting images. They are excreted from the body in the urine, without having a negative effect on internal organs. Modern angiography allows you to obtain a three-dimensional image of the arteries of the circle of Willis.
Dopplerography
The method is carried out simultaneously with ultrasound examination of cerebral vessels. Dopplerography allows you to evaluate the structure of the vessels of the circle of Willis and identify their anomalies. In this case, the doctor can examine the speed of blood flow.
Diagnostics
The examination is carried out under the supervision of a vascular surgery specialist. It is possible to involve a neurologist.
The measures are mostly standard; it is necessary to carefully evaluate the anatomical structure of the circle of Willis.
- Angiography. Essentially an x-ray with contrast. A special drug is introduced, which, accumulating in the blood, enhances the pattern. Then doctors take a series of photographs and, based on the results, evaluate the nature of the structure of the ring-shaped structure. It is considered an accessible and relatively simple diagnostic method with a minimum of contraindications.
- Dopplerography of cerebral vessels. Required to assess the speed and quality of blood flow in cerebral structures, used as part of a functional examination. Prescribed in all cases.
- MRI. To identify complex forms of anomaly. This is perhaps the most informative technique among others. Maximum safe, does not create a load on the body, and is not accompanied by pain. But the research costs on average more than its analogues. That’s why they resort to this method when others have failed.
- It is possible to prescribe invasive, selective angiography.
Activities can be adjusted during the examination and supplemented with other techniques. The issue is resolved at the discretion of the specialist.
Treatment approaches
If the arterial circle is not closed, special treatment is not required. Without accompanying changes in the blood vessels, people do not experience any symptoms of disease. Therapy should be aimed at preventing arterial pathologies and eliminating them.
For this, patients are prescribed a number of medications, and are also advised to adhere to a diet and change their lifestyle.
Non-drug approaches
All patients should adhere to medical recommendations regarding lifestyle:
- exercise regularly. To prevent vascular diseases, aerobic exercise is recommended: walking, jogging, cycling and swimming. Classes should be ongoing and suitable for the person’s level of physical fitness;
- eliminate bad habits: smoking and drinking alcohol;
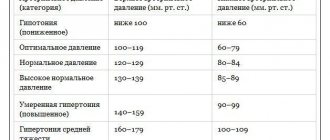
- Avoid fatty, salty, fried and spicy foods in your diet. They contribute to the development of atherosclerosis and hypertension. Both conditions are often complicated by thrombosis, aneurysms and their rupture;
- It is recommended to eat more vegetables, fruits, berries, nuts and lean meats. They are rich in beneficial amino acids, vitamins, microelements and biologically active substances that have a positive effect on the condition of the cardiovascular system;
- Limiting salt intake to 5 g per day. If the patient has severe arterial hypertension, then the volume of consumption is reduced to 1 g;
- avoid stressful situations at work and in your personal life.
These recommendations reduce the risk of developing heart and vascular diseases by preventing pathological changes in the arterial circle of the brain.
Medicines
Medications are recommended for people with vascular pathology of the circle of Willis and accompanying changes in the arteries. Medicines of the following pharmacological groups can be used:
- drugs that improve cerebral circulation (Cerebrolysin, Cavinton, etc.). They normalize vascular tone and increase the intensity of blood flow in the arteries of the brain. This avoids ischemia and neurological disorders;
- nootropics – Phenotropil, Glycine, Nootropil, etc. They enhance metabolic processes in neurons and reduce their sensitivity to damaging factors. Requires long-term use over several months to obtain a therapeutic effect;
- antioxidants (Dihydroquercetin, Mexidol) protect nerve cells from damage, including toxic substances. The effect is achieved by blocking free forms of oxygen, which negatively affect the structures of neurons;
- antispasmodics (Drotaverine, Papaverine and their analogues) are prescribed for spastic changes in blood vessels. Allows you to dilate arteries and restore normal blood supply to the brain. They have only a symptomatic effect and do not affect the underlying disease;
- B vitamins, which stimulate the restoration of nerve tissue and neuron membranes. Used in courses in the form of intramuscular injections;
- To eliminate pain, non-steroidal anti-inflammatory drugs (Diclofenac, Nise, etc.) are prescribed. They are highly effective for any form of headache, except migraine.
All medications are prescribed only by a doctor. Medicines have contraindications, failure to comply with which may cause progression of the underlying disease or lead to the development of side effects.
Surgical treatment
In case of multiple blood flow disorders, the patient is prescribed surgical interventions. They may be associated with the creation of a shunt or mechanical expansion of the lumen of the arteries. A shunt is a bypass for blood flow, which is placed around a narrowed area, an area of hypo- or aplasia. Mechanical expansion of the vessel is carried out using a stent or ballooning.
What are the dangers of improper development?
Congenital abnormalities can gradually create obstruction of the blood supply or signs of decompensation when excessive stress is placed on the arteries.
The consequences can be completely catastrophic - the development of an aneurysm, hemorrhagic or ischemic strokes.
Even young people can experience periodic migraine attacks.
In the older age category, aneurysms caused by acquired pathologies (atherosclerosis, vasculitis infections, syphilis) more often occur.
An aneurysm is a protrusion on the wall of an artery; the development of pathology occurs without visible symptoms. Most often localized inside the circle of Willis (in the ACA or PCA, at the bifurcation of the ICA and BA) against the background of the asymmetric structure of the arterial ring.
When an aneurysm forms, there is a danger of rupture of the vessel and, as a result, hemorrhage in the brain.
Clinical syndromes caused by arterial ring aneurysms:
- pseudotumor - nerve tissue and brain matter are compressed;
- hemorrhagic extracerebral basal - after rupture of a vessel with subarachnoid hemorrhage;
- discirculatory - with slow growth or with the development of a dissecting form of aneurysm.
Anomalies in branching options and deformation of the shape (broken circle) weaken or lead to loss of compensation in complex cases (hypertensive crisis, thrombophlebitis, spasm, etc.).