Extrasystole is a condition related to heart rhythm disturbances, or arrhythmias, which are expressed by extraordinary contractions of the heart or its parts. Depending on the location of the source of excitation, it can be ventricular, atrial, atrioventricular.
Supraventricular extrasystole, or supraventricular, is characterized by the fact that premature impulses arise in ectopic foci located in the upper parts of the heart (atria) or in the septum between the ventricles and atria, which is called the antiventricular. As a result, incomplete additional contractions of the heart occur.
Causes
Supraventricular extrasystole can be idiopathic, that is, it occurs without any apparent reason. It can be observed in practically healthy people at any age. In addition, there are different reasons for the development of supraventricular extrasystole:
- Heart diseases: heart failure;
- cardiac ischemia;
- myocardial infarction;
- heart defects, both congenital and acquired;
- myocarditis (inflammatory processes in the heart muscle);
- cardiomyopathy.
- diabetes;
- alcohol abuse;
- antiarrhythmic drugs;
Symptom severity
Supraventricular extrasystoles (hereinafter referred to as SVE) according to symptoms are divided into:
- Organic systole. This is a condition in which the patient feels much worse in an upright position than in a horizontal position;
- Systole is functional. A condition when the patient feels much better in an upright position than in a lying position.
The patient cannot always recognize the pathology at the initial stage of the disease. The symptoms of this disease do not appear clearly and often the person simply does not feel them.
When the symptoms become pronounced, then we can talk about a more complex stage of development of the pathology, which is much more difficult to treat. Therapy for this stage of the disease is quite complex and takes a long period of time.
In order to recognize supraventricular extrasystole, you need to listen to the following symptoms in the body:
- The performance of the heart occurs intermittently. A situation in which the heart simply “jumps out of the chest”;
- Discomfort behind the chest;
- Malaise of the whole body;
- Large amounts of sweat;
- Unreasonable irritability;
- Deep state of overexcitation;
- State of paranoia;
- Sense of anxiety;
- Dizziness that occurs over a long period;
- Shortness of breath or lack of oxygen in the body.
Supraventricular extrasystole quite often is not the main diagnosis of cardiac abnormalities, but is a concomitant disease of heart disease, and can also be a consequence of somatic diseases.
Dystonia (vegetative-vascular) is confirmed by identical symptoms of increased heart rate, which does not depend on the amount of physical activity. When examined using an electrocardiogram, supraventricular (supraventricular) extrasystole is detected.
Also, this disease can provoke osteochondrosis of the thoracic spine. Disorders in the spine impinge on blood vessels that do not normally supply vital internal organs in the body. The heart muscle suffers the most from insufficient blood circulation.
The main pathologies due to which she may get sick
Classification
Supraventricular extrasystoles are classified according to several criteria:
According to the location of the outbreak
- atrial - in the upper parts of the heart,
- atrioventricular - in the septum between the ventricles and atria.
Frequency per minute
- single (up to five extraordinary reductions),
- multiple (more than five),
- group (several extrasystoles in a row),
- doubles (two in a row).
By number of outbreaks
- monotopic (1 lesion)
- polytopic (several foci).
By time of appearance
- early (with atrial contraction),
- average (between the time of contraction of the atria and ventricles),
- late (with contraction of the ventricles or with complete relaxation of the heart).
By order
- ordered (alternating normal contractions with extrasystoles),
- disordered (there is no pattern).
Medical reference books
Supraventricular rhythm disturbances
Supraventricular arrhythmias account for 4/5 of the total number of tachycardias and occupy an intermediate position between potentially life-threatening and benign cardiac arrhythmias. Supraventricular rhythm disturbances include sinus tachycardia, supraventricular extrasystoles and supraventricular paroxysmal tachycardia; This also includes atrial flutter and fibrillation. Normally, the sinus node generates impulses at a frequency of 60-90 beats per minute. Normal sinus rhythm is correct; as a variant of the norm, sinus arrhythmia can occur.
Sinus tachycardia
Sinus tachycardia is an increase in cardiac activity at rest over 100 beats per minute with the correct rhythm; during maximum physical activity in healthy young people it can reach 190-220 per minute. Mechanism. The development of arrhythmia is carried out due to increased automatism of the cells of the sinus node due to various influences of the autonomic (sympathetic and parasympathetic) nervous system. Increased automaticity function can cause increased tone of the sympathetic nervous system (excessive production of catecholamines or their toxic effect) or decreased tone of the vagus nerve (inhibition of the acetylcholine-cholinergic effect). Hypoxemia, acidosis, elevated body temperature, intoxication, and infections directly affect the cells of the sinus node. With sinus tachycardia, the conduction of excitation impulses through the atria and atrioventricular node occurs normally. The atria and ventricles are excited and contract in a coordinated manner, but shortened diastole creates unfavorable conditions for the functioning of the heart.
Clinic. Complaints are usually absent or minor - palpitations, a feeling of heaviness or pain in the cardiac region. Auscultation - correct rhythm with a heart rate of 100-150 beats per minute, with a gradual beginning and end. ECG diagnosis - all signs of sinus rhythm, P wave - positive in I, II, avF, negative in avR, biphasic in V1, V2.
Treatment. The main principle is the elimination of factors that provoke the development of tachycardia.
Atrial extrasystoles
Atrial extrasystoles (AEC) are premature, time-leading excitations and contractions of the entire heart or its parts, the impulse for which comes from various parts of the atria. They are caused by impulses arising in a focus with pathologically increased excitability, located outside the sinus node and belong to active ectopic rhythms.
Etiology. Approximately 1/3 of supraventricular ES is functional in nature and is observed in healthy people. It may be a manifestation of general neurosis with neurovegetative dystonia, or an expression of changes in corticovisceral regulation. Abuse of strong tea, coffee or alcohol, smoking, etc. have a great influence on their occurrence. In people with neurosis, the frequency of ES ranges from 7 to 14%. In each specific case, when determining the etiology of neurogenic ES, one should look for mental and physical fatigue, irregular sleep, sexual dysfunction, iatrogenics, domestic and professional psychotrauma. Various intrasecretory conditions and disorders (menopause, pregnancy, menstrual period, ovarian dysfunction) may play a role in the occurrence of ES in individuals without heart disease. Neuroreflex: the result of pathological irritation emanating from other internal organs through viscerocardial reflexes. PES of organic origin can cause processes in the lungs and mediastinum, pleural and pleurocardial adhesions, pneumosclerosis and cervical osteochondrosis. The appearance of atrial ES is facilitated by stagnation and stretching of the atria, for example, in patients with left or right ventricular failure or mitral stenosis. They often turn into atrial fibrillation in such situations.
Causes of atrial ES: - acute respiratory failure, chronic obstructive pulmonary diseases, hypoxia, - heart failure, - ischemic heart disease (angina), valvular heart disease, - use of digitalis, quinidine, procainamide (proarrhythmogenic effect is associated with prolongation of the absolute refractory period of the AV node), - excessive consumption of coffee, alcohol, nicotine , - stress, overwork, overeating.
Clinic: arrhythmic pulse, feeling of heartbeat, there may be no interruptions, after myocardial infarction - a reaction to pain. ECG diagnosis: The PES is characterized by a non-widened QRS complex, the P' wave may be biphasic, negative or absent. It can be recorded both before and after the QRS. Depending on the source of the ES, there may be no P' wave at all. With supraventricular ES, in most cases, an incomplete compensatory pause is observed, however, with stem ES, the compensatory pause is always complete.
Treatment – the underlying disease or known causes (exclude coffee, alcohol, smoking). For frequent atrial ES, if they trigger tachycardia, digitalis, verapamil, and beta-blockers (propranolol) are prescribed. Most often, specialized treatment is not required. The main indications for antiarrhythmic therapy are hemodynamic significance and subjective intolerance. In the second case, you should remember about tranquilizers and antidepressants. The selection of drug therapy is carried out individually. If the patient has concomitant ischemic heart disease, the prescription of antiarrhythmic drugs of all classes except the first is indicated.
Supraventricular paroxysmal tachycardias
Supraventricular paroxysmal tachycardias (SPT) are attacks of increased cardiac activity of a regular rhythm, with a heart rate of 140-220 beats per minute, with a sudden onset and end, as a result of activation of a center located outside the sinus node. The ectopic focus that provokes the development of SPT is located in the atria, AV node or common trunk of the His bundle. A special place is occupied by tachycardia against the background of WPW syndrome (presence of additional conduction pathways) - orthodromic and antidromic. Since re-entry includes the atrium, ventricles, AV node, and additional conduction tracts. In cardiological practice the most common are: · sinoatrial; · atrial; · atrioventricular nodal; · atrioventricular reciprocal tachycardia with the participation of additional pathways (WPW and Clerk-Levy-Critesco syndrome).
Mechanisms of development. The origin of paroxysmal tachycardias can be due to several mechanisms: due to impaired impulse formation and impaired impulse conduction. Impulse formation disorders include disorders of automaticity and triggered activity. Disturbances in the function of automaticity arise due to the presence of an ectopic focus in the heart muscle, and are the result of altered cellular metabolism due to local biochemical and electrolyte disorders. In the occurrence of an ectopic focus, a major role is played by the state of the central and autonomic nervous system, the presence of a focus with myocardial damage and local biochemical and electrolyte disturbances. There are two types of disorders - accelerated normal automatism and pathological automatism. The first causes the development of tachycardia in patients with a practically healthy heart. Damage to the myocardium due to inflammation, dystrophy or the development of scar fields leads to the appearance of lesions with pathological automatism. Among electrolyte disturbances, hypo- or hyperkalemia is of greatest importance. The appearance of early post-depolarizations is due to a slowdown in repolarization processes due to a weakening of the outgoing current of potassium ions in relation to the incoming currents of sodium and calcium. It is realized against the background of slowing repolarization and increasing the duration of the action potential. Predisposing factors are bradycardia, hypokalemia and hypomagnesemia. The appearance of late post-depolarizations is associated with cell overload with calcium ions. This is facilitated by the activation of the effect of catecholamines on the heart. Impaired impulse conduction is associated with the formation of a “closed loop” mechanism (re-entry). The development of re-entry is due to the circular movement of the excitation wave in the myocardium and fibers of the conduction system of the heart. There are anatomically determined development of tachycardia against the background of WPW syndrome (presence of additional pathways) and functionally determined - arrhythmias due to longitudinal dissociation of the AV connection, etc.
Etiology. The development of paroxysmal tachycardia can be observed in practically healthy people; it is caused by extracardiac causes. These include neurosis with lability of the autonomic nervous system, sympathicotonia, psycho-emotional effects, excessive consumption and increased sensitivity to substances that stimulate the nervous system (nicotine, coffee, tea, alcohol). The development of SPT can be a manifestation of viscerocardial reflexes and is associated with pathology of adjacent organs - gastric ulcer, acute and chronic pancreatitis, cholelithiasis, nephrolithiasis, colitis, constipation, diseases of the mediastinal organs, spine, organic diseases of the nervous system, etc. Also predisposing factors can be hormonal disorders - pregnancy, puberty, menstruation, menopause, thyrotoxicosis, ovarian dysfunction, pituitary diseases and allergic-anaphylactic reactions. Genetically determined causes are tachycardia against the background of the existence of additional conduction pathways. The cause of the development of tachycardia may be intoxication with digitalis drugs, congenital or long QT syndrome. Of the organic diseases of the heart muscle, SPT develops against the background of rheumatic valve defects, coronary heart disease, and hypertensive heart.
Clinical picture. Subjectively, patients feel a sudden strong palpitation with an initial beat (push) in the heart area with the same sudden ending with a feeling of cardiac arrest. The attack is described as fluttering or “jumping” in the heart area, a feeling of heaviness in the heart area, pulsation and a feeling of tension in the neck and head, general weakness, fear, excitement, tension, dizziness. An attack of paroxysmal tachycardia may be accompanied by increased sweating, increased peristalsis, flatulence, nausea and vomiting. A very important diagnostic sign is frequent and copious urination for several hours; a large amount of light-colored urine with low specific gravity is released. This is the so-called urina spastica, associated with the relaxation of the sphincter of the bladder, which is spasmed during an attack. The end of the attack, often in the form of a jolt and “freezing” in the heart area, is accompanied by a feeling of relief, normalization of cardiac activity and breathing. Clinically, during an attack of paroxysmal tachycardia, patients experience pallor of the skin and visible mucous membranes. The neck veins swell and pulsate synchronously with the arterial pulse. Breathing is rapid. The pulse is rhythmic, sharply increased, difficult to count, and weak in filling. On auscultation, a pendulum-like rhythm is heard, with a heart rate from 150 to 220 per minute. Blood pressure is normal or low. As a rule, attacks occur without a drop in hemodynamics, patients are conscious and adequate, although severe weakness develops. Cardiogenic shock rarely develops with a severe general condition, impaired consciousness, a drop in blood pressure and manifestations of the central and autonomic nervous systems, decompensation and shock.
ECG diagnostics. The rhythm is correct, RR intervals are greatly shortened, but equal to each other, permissible fluctuations are 0.06 s. The constancy of the duration of RR intervals is one of the differential diagnostic features. Depending on the location of the ectopic focus, the P' wave can be positive, biphasic or negative. Each P' wave is followed by a ventricular complex. Often the P' wave merges with the preceding T wave and is not distinguishable on the ECG. The QRS complex is not widened, not deformed, the ST segment and T wave are not changed, and ST segment depression is often observed against the background of high heart rate. Sometimes frequency-dependent bundle branch blocks may occur with all the signs of blocked branches (widening of the QRS complex by more than 0.12 s, discordant changes in the final part of the ventricular complex - the ST segment and the T wave are directed in the direction opposite to the main wave of the QRS complex). Frequent attacks of paroxysmal tachycardia can cause the development of tachycardic cardiomyopathy, with dilation of the heart cavities and subsequent development of heart failure. During an attack of paroxysmal tachycardia with a high heart rate, coronary circulation is significantly disrupted, which can lead to the development of myocardial infarction in patients with coronary heart disease. Sometimes an attack of paroxysmal tachycardia leads to thromboembolic complications. Dynamic cerebrovascular accidents and thromboembolism of peripheral vessels may develop. Often, patients, especially those suffering from severe coronary atherosclerosis, develop post-tachycardia syndrome, which is caused by impaired metabolic processes in the heart muscle and myocardial ischemia. On the electrocardiogram after an attack, ischemic changes in the terminal part of the ventricular complex appear in the sinus complexes in the form of negative T waves, depression of the ST segment, which, the more pronounced the organic changes in the heart muscle, the longer they persist on the ECG.
Treatment. When an attack of paroxysmal tachycardia develops, emergency management of patients includes performing so-called vagal tests, influencing nervous regulation by stimulating the branches of the vagus nerve. These techniques include: the Chermak-Goering test, the Aschner-Danyini test, the Valsalva test. The Chermak-Hering test is performed by applying mechanical pressure to the area of the carotid sinus (carotid sinus), located at the bifurcation of the common carotid artery. The test is carried out with the patient lying on his back. Press on only one side on the inner surface of the upper third of the sternocleidomastoid muscle at the level of the upper edge of the thyroid cartilage. The area of the carotid sinus is gradually pressed with the thumb of the right hand, towards the spinal column. The duration of pressure is no more than 30 seconds, under constant monitoring of the pulse. Typically, pressing on the right carotid node is more effective. As soon as the attack has stopped, pressure on the carotid artery must be stopped immediately due to the risk of prolonged ventricular asystole. This test is contraindicated in elderly people with severe cerebral atherosclerosis, as well as in the late stages of hypertension. To relieve an attack of paroxysmal tachycardia, the Aschner-Danyini test is used. Apply moderate and even pressure on both eyeballs. This test is also performed only in a horizontal position of the patient. The tips of the thumbs apply pressure for no more than 30 seconds on the patient’s closed eyes, directly above the upper supraorbital arches. For eye diseases and severe myopia, this test is contraindicated. The next test used to relieve an attack of paroxysmal tachycardia is the Valsalva maneuver. This is a mechanical technique - straining while taking a deep breath and pinching the nose, artificially inducing vomiting, coughing, strong pressure on the upper abdomen, bending and pressing the legs to the stomach, cold rubbing of the skin, etc. In terms of effectiveness, the Valsalva maneuver is the most effective. The effectiveness of stopping tachycardia is 70-80%. The most effective drug for relieving SPT is adenosine. Adenosine is administered intravenously in a stream over 1-3 s. at an initial dose of 6 mg; if there is no effect, it is advisable to administer a second dose - 12 mg, if necessary, after 1-2 minutes - another 12 mg. Transient side effects include facial flushing, chest discomfort, difficulty breathing, and AV block. If there is no effect, verapamil is administered at an initial dose of 2.5-5 mg IV, then this drug can be used orally at a daily dose of 240 mg/day. The use of adenosine should be avoided in patients with bronchial asthma, vasospastic form of angina, in combination with beta-blockers. Verapamil or diltiazem should be used instead. Digoxin and propranolol, esmolol, and sedatives can also be used in the treatment of SPT, but it should be remembered that verapamil and digoxin cannot be used in the treatment of tachycardia of unknown etiology with wide QRS complexes.
In WPW syndrome, the following are distinguished: · paroxysmal reciprocal AV-orthodromic tachycardia (anterograde impulse is conducted through the AV node, retrograde – through the AP node), · paroxysmal reciprocal AV-antidromic tachycardia (anterograde – through the AP node, retrograde – through the AV node).
ECG criteria for orthodromic paroxysmal tachycardia in WPW syndrome: heart rate - 170-220 beats per minute, rhythm - correct, RR intervals - the same. Negative P waves are often not visualized because they overlap the QRS complex. The QRS complexes are not widened or deformed, their duration does not exceed 0.12 s. (impulses enter the ventricles through the AV connection).
ECG criteria for antidromic paroxysmal tachycardia in WPW syndrome: heart rate - 170-220 beats per minute, rhythm - correct, RR intervals - the same. P waves are not visualized because they overlap the QRS complex; sometimes a negative P wave is located behind the QRS complex. The QRS complexes are widened, lasting more than 0.1 s, and not deformed (a reflection of the maximum pre-excitation of the ventricles, when they are excited non-simultaneously).
Treatment of orthodromic SPT with narrow QRS complexes: vagal tests, if ineffective - ATP 10-30 mg or adenosine 6-12 mg IV bolus over 1-3 s. Verapamil or diltiazem can be used in optimal doses. If possible, insert a probe electrode into the esophagus to the level of the right atrium and perform ultra-frequent stimulation with a current of 10-30 mA, with the maximum possible duration of the stimulus. If ineffective - electrical cardioversion sequentially 150-200-270 kJ.
Treatment of antidromic SPT with wide QRS complexes: ATP, adenosine and verapamil is dangerous to administer, as it can provoke the development of ventricular fibrillation. First-line drugs are procainamide 0.5-1.0 g IV in a bolus, disopyramide 150 mg IV in a bolus, or sotalol 40 mg IV in a bolus or amiodarone 300-450 mg IV in a bolus. If ineffective, use electrical cardioversion. Planned treatment of reciprocal tachycardias is radiofrequency catheter ablation (modification) of the corresponding conductive structures of the heart. It is a first-line treatment and is offered to all patients with supraventricular reentrant tachycardia, which is associated with its safety, favorable cost-effectiveness ratio and the ability to eliminate the background mechanism of arrhythmia with minimal risk of complications. In case of AV nodal tachycardia, exposure in the area of the AV junction is preferable (less risk of AV block) - ablation of slow pathways. With WPW – ablation of additional pathways. Preventive antiarrhythmic therapy for reciprocal tachycardia is carried out only if there are contraindications or the patient refuses radiofrequency ablation.
Signs
With supraventricular extrasystole there are often no complaints. In some cases, the disease causes the following symptoms:
- lack of air, shortness of breath;
- interruptions in the work of the heart: a feeling of “reversals” of the heart or beats out of rhythm;
- dizziness;
- general weakness.
In children, supraventricular extrasystole most often occurs without any symptoms. Complaints usually come from older children. The child may experience weakness, irritability, fatigue, dizziness, and a feeling of heart failure.
What is supraventricular extrasystole?
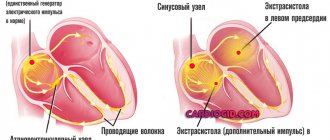
Extrasystole is the general concept of extraordinary (arrhythmic) heart contractions. According to localization they are divided into the following types:
- supraventricular extrasystole (supraventricular);
- ventricular extrasystole (ventricular);
- antiventricular extrasystole (atrioventricular).
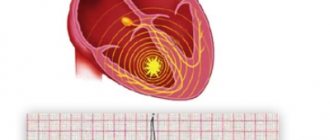
The foci of supraventricular extrasystoles are located in the atria, that is, above the ventricles. Hence the name arrhythmia. The atrioventricular form is characterized by the appearance of ectopic (arising in the wrong place) contractions in the septum between the atrium and the ventricle or between the ventricles. Ventricular extrasystole is localized in the ventricles. The consequence of supraventricular and ventricular extrasystoles is often changes in the muscle tissue of the heart (myocardium).
Classification of atrial extrasystole is made according to many parameters. By number of pulses per minute:
- single (number of unscheduled layoffs 1 – 5);
- paired (two pulses in a minimum period);
- group (several reductions per period);
- multiple (over 5 extraordinary impulses).
Based on the number of sources of impulse generation, they are distinguished between monotypic (one source) and polytopic (more than one source of excitation). If there is a certain pattern in the passage of normal contractions and extraordinary ones, then they speak of organized extrasystole. If this alternation is chaotic, then it is called disorganized. Division by etiology (origin) of arrhythmia:
- organic extrasystole is caused by pathological changes in the heart, which in particular includes sinus extrasystole;
- functional, resulting from other disorders in the body.
Extrasystole on ECG
Extrasystole leads to the fact that the heart cannot fully contract. And this in turn can cause supraventricular tachycardia and fibrillation.
Diagnostics
Diagnosis is based on the patient’s complaints, a general examination with listening and measuring the pulse, as well as on the patient’s story about the lifestyle, bad habits, heredity, past illnesses and operations.
In addition, laboratory tests are required: general and biochemical analysis of blood and urine, determination of hormonal status.
Pulse measurement
Instrumental diagnostic methods include the following: ECG, Holter monitoring, electrophysiological study, echocardiography (ultrasound of the heart), stress tests with recording of an electrocardiogram during and after exercise.
Diagnostics and its methods
Most often, the primary diagnosis is an electrocardiogram. Most often, extrasystole is detected during a medical examination and requires a more thorough study of the heart.
Sometimes, if the patient already has symptoms of some kind of heart problems after physical activity, then diagnostic procedures are used that measure the heart rate after physical activity.
In addition to these methods, there is also a classic examination by a doctor, where he measures the patient’s pulse and listens to the work of the heart.
- Why ventricular extrasystole occurs, symptoms and treatment of pathology
Treatment
If there are no organic heart diseases, the patient has no complaints, then specific treatment for supraventricular extrasystole, as a rule, is not carried out . Therapy is usually indicated when symptoms are present and poorly tolerated.
First of all, the doctor assesses the number of extraordinary heart contractions per day. A single extrasystole does not pose a health hazard. Then you need to make sure that there are no organic heart diseases. If the patient has subjective complaints and does not tolerate them well, sedatives may be used. The doctor should evaluate the advisability of taking antiarrhythmic drugs. The fact is that they have many side effects, and therefore the treatment can become more dangerous than the disease itself. Rare supraventricular extrasystole (several tens or hundreds of contractions per day) does not require taking such serious medications. Thus, in the absence of complaints and diseases, the patient is recommended:
- Eat right, that is, exclude preservatives, fatty, fried, spicy, hot foods. Eat more plant foods rich in fiber.
- Eliminate bad habits (alcohol, smoking, energy drinks).
- Avoid stress and exercise in moderation.
- Ensure restful and sufficient sleep.
- Spend more time outside.
In the presence of heart disease and severe symptoms, conservative treatment with glycosides and antiarrhythmic drugs is indicated, which are selected strictly individually.
If medications do not help and the patient does not tolerate extrasystole, surgical treatment is performed.
This may be an open operation in which ectopic lesions are removed. As a rule, it is performed when intervention for heart valve replacement is required.
Another type of surgical treatment is radiofrequency ablation of lesions using a catheter, which is inserted into a large blood vessel, an electrode is passed through it and the area where the pathological impulse occurs is cauterized.
What does it represent?
According to the International Classification of Diseases (ICD-10), supraventricular extrasystole has code 149.4. It is included in the registry of cardiac arrhythmias in the heart diseases section.
Extrasystole can be of different types, but the main ones are atrial and ventricular. When an additional contraction out of turn is caused by an impulse that comes from the ventricular system, they speak of ventricular extrasystole. These attacks are accompanied by an interruption in the heart rhythm, which is accompanied by weakness and dizziness.
- Extrasystole of the heart causes and symptoms treatment
According to ongoing studies, single extrasystoles can also occur in healthy people; 50% of the patients studied had positive results.
Therefore, we can say that this condition can be physiological and occur in healthy people. Stress may be the main cause of functional impairment. In addition, drinking alcohol and energy drinks, smoking, etc. can also provoke extrasystole. In these cases, the pathology is considered harmless and quickly goes away on its own.
As for pathological ventricular arrhythmia, it develops against the background of serious diseases and requires mandatory treatment and monitoring by a specialist.
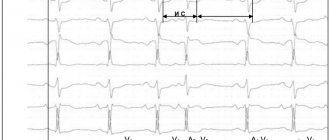
ECG No. 4
This is another ECG demonstrating a variant of supraventricular (also nodal) extrasystole. Only here it’s difficult to find the ‘P’ wave without knowing where to look. It may seem incredible, but it is here and seeing it once, you will be wary in the future.
The ectopic focus is located in the lower parts of the AV node, and possibly in the trunk of the His bundle (before the branching of the legs), since ventricular excitation (QRS) begins much earlier than retrograde excitation of the atria (negative P).
To close the topic, let’s look at the topic “Ventricular extrasytolia” and only then complete the task for self-control.
Prognosis, complications and consequences
According to some experts, frequent supraventricular extrasystole after a few years can lead to the development of heart failure, atrial fibrillation and cause a change in the configuration of the atria.
The prognosis for SE is favorable. This disease does not lead to sudden death, unlike ventricular extrasystole in combination with organic heart damage.
- Extrasystole - what is it, causes and methods of treatment
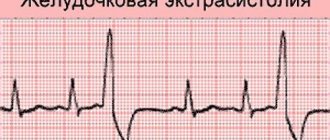
ECG No. 3
The fourth complex is extrasystolic, and there is a negative P wave in front of the QRS. This means that the atria were depolarized retrogradely (from bottom to top), this is only possible when the ectopic pacemaker (extrasytoles) is localized in the AV node itself or in the immediate vicinity of it.
! Channel V1 was not recorded due to technical reasons, but still I included this indicative ECG in this course