Dysplastic cardiopathy (DCP), an abnormal or accessory chord in the left ventricle - when faced with these terms, many parents begin to think that the child has a heart defect. The KinderKlinik pediatrician will tell you whether this condition poses any threat to the child’s life, whether the child needs to be limited in the level of physical activity and how often it is necessary to undergo preventive examinations.
What is an anomaly
First you need to figure out: what is an abnormal chord of the left ventricle?
This name refers to an anatomical feature of the structure of this organ, in which the chords (the so-called fibrous muscle connecting the opposite walls of the left ventricle) have an incorrect location. Of all the types of abnormalities found in the heart, this is the most common.
Irregular chords vary in number: both single (they account for 62%) and multiple (they account for 38%).
Sign up for a consultation
An abnormally located chord in the cavity of the left ventricle is not a disease; as a rule, it does not threaten the body in any way and does not interfere with blood flow. But, in some cases, it can cause disturbances and interruptions in heart rhythms.
Such a phenomenon as an abnormal chord of the left ventricle of the heart is often genetic in nature and is often transmitted to the child from the mother, who is not even aware of such a phenomenon in her body.
The following can lead to an abnormal phenomenon occurring in the womb during the development of a small organism:
- smoking during pregnancy (this is the most dangerous factor);
- bad ecology;
- weak immunity of women;
- improper (unbalanced) nutrition;
- frequent stress, emotional overstrain;
- infection to the fetus.
Interesting! It has been noted that this anomaly is characteristic of people with a thin body structure.
In adults, abnormally located chordae are found much less frequently than in children. This is because over time they may disappear as an anomaly. For example, stretch out or shift, fuse with the surface of the heart muscle. This phenomenon is understandable: in a newborn, the left ventricle of the myocardium has the shape of an ellipse, and with the growth and development of the body it becomes more like a ball.
There are cases when, against the background of advanced heart diseases and defects, drug or alcohol addiction, an abnormal chord appears.
call me back
What is a chord
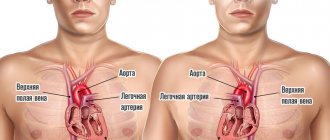
The human heart consists of 4 chambers through which blood regularly passes - 2 ventricles and 2 atria. Blood flow moves through valves, which open in chords. When tensioned, the valve opens the flaps, and when loosened, it closes. Thanks to this, the blood flows only in a given direction and does not move backward.
The valves tension special longitudinal strands - chords. But along with the main ones, additional chords are often identified. They are also attached to certain parts of the heart, but do not take any part in pumping blood. Therefore they are also called false chords.
Symptoms and manifestations
An abnormal chord in the heart does not show any characteristic external signs; its existence may not be known for years. Most often, it is detected only during an ultrasound examination, and the basis for referral for an ultrasound is when the doctor listens to a noise in the area during normal heart function, which should not exist.
For information! Murmurs are acoustic phenomena (whistle, creaking) that appear during contraction of the heart muscle, between beats, and are audible when listening with a stethoscope.
The intensity of the noise depends on the location of the abnormal chord of the left ventricle and on their number (if there is a multiple phenomenon). Also, with multiple anomalies, you can notice some features of the general condition:
- increased fatigue;
- mood swings and instability of psycho-emotional state;
- arrhythmia;
- increased heart rate;
- pain in the chest area.
Get a treatment program
A minor anomaly of cardiac development is manifested by symptoms of autonomic dysfunction:
- pain in the heart area;
- emotional lability;
- fatigue;
- signs of astheno-neurotic syndrome;
- a characteristic heart murmur is heard.
Their manifestations can become more pronounced as the child grows, leading to various complications, for example, heart rhythm disturbances and the formation of additional pathways in the heart. This leads to poor exercise tolerance and a tendency to faint. Such children are at risk for developing infective endocarditis - complications after acute respiratory infections and tonsillitis in the form of an inflammatory process of heart tissue.
Prevention of the development of complications is a timely visit to a doctor in cases of the appearance of the listed complaints and the implementation of prescribed diagnostic measures.
Children are prescribed an ECG (to determine possible arrhythmias) and echocardiography (ultrasound of the heart). This method allows you to visualize the heart and large vessels, clarify the presence of cardiac abnormalities and determine whether there are disturbances in its functioning.
Make an appointment with a pediatric cardiologist and examination by phone +7(495)150-60-03
Services and prices
Primary appointment (examination, consultation) with a pediatric cardiologist
2,200 rub.
Repeated appointment (examination, consultation) with a pediatric cardiologist
2,100 rub.
Electrocardiogram at rest
600 rub.
Electrocardiogram with functional tests
1,000 rub.
Echocardiography with Doppler analysis (in PW, CW mode) and color two-dimensional Doppler mapping for children under one year old
RUB 3,800
Echocardiography with Doppler analysis (in PW, CW mode) and color two-dimensional Doppler mapping for children from 1 year to 7 years
3,700 rub.
Echocardiography with Doppler analysis (in PW, CW mode) and color two-dimensional Doppler mapping for children over 7 years old
3,600 rub.
Diagnosis and treatment
If a pediatrician detects murmurs when listening to the work of the myocardium, then you should definitely visit a cardiologist and undergo a diagnostic examination, including:
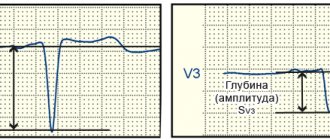
- taking an electrocardiogram (with its help it will be possible to identify whether there are disturbances in the functioning of the myocardium);
- ultrasonography.
It is very important that if the examination shows the presence of an abnormally attached chord of the left ventricle, you need to periodically visit a cardiologist, because this phenomenon creates noise, due to which it is possible to untimely pay attention to the appearance of serious diseases associated with the work of the myocardium.
Regarding the chord itself, it should immediately be noted that its abnormal location in the left ventricle does not require specific treatment, much less such as surgery. But there are a number of rules that must be strictly followed by those who have this phenomenon.
Diagnostics
First of all, you need to contact a therapist or children's doctor (pediatrician), who will listen to your heart rhythm using a stethoscope. It is very easy to hear a heart murmur, so the therapist can easily make a preliminary diagnosis after the first examination.
Next, the patient may be referred for additional diagnostics:
- ECG at rest and after exercise;
- blood pressure measurement;
- Holter monitoring.
Thanks to the examinations carried out, it is possible to accurately determine the presence of a chord, the degree of its danger to health, as well as other diseases (if any).
Diagnostics: how to determine LVHL
When the doctor tells you that your baby has a heart murmur, there is no reason to panic. The condition does not require emergency resuscitation measures or intensive treatment. The main diagnostic method is ultrasound examination. It will help clarify the location and number of additional strands. There are the following types of LVDC:
- according to location in the ventricle - apical, middle, basal;
- in relation to the axis of the heart - diagonal, longitudinal, transverse;
- by number - singular and plural.
If echocardiography has revealed an additional chord in the cavity of the left ventricle in a child of any age, I advise parents to undergo the following examinations:
- A general blood test is not important in terms of diagnosing LVHL, but it will reveal anemia or an existing inflammatory process in the body, which can aggravate the condition of a child with a minor cardiac anomaly.
- Electrocardiography. It is advisable to conduct Holter monitoring, which will exclude arrhythmia with greater diagnostic accuracy.
- ECG tests with physical activity will show how well the child’s heart “copes” with its function.
- Consultations with specialized specialists (orthopedist, endocrinologist, otolaryngologist).
I always explain to parents of infants that sometimes the abnormal chord can lengthen and “grow” into the valve, so during subsequent ultrasounds the doctor does not detect LVDC. In such cases, they say that the baby has “outgrown” this pathology.
Forecast
In most cases - favorable. Even when symptoms develop, many years pass before the process reaches a critical, decompensated phase.
This can only be achieved consciously. Typically, symptoms in the earlier stages are unbearable and significantly reduce the quality of life. There is no choice but to see a doctor.
The survival rate is good, the likelihood of maintaining working capacity is also good. But this does not mean that you need to sit idly by. You cannot do without the consultation and help of a cardiologist.
Reasons for the development of the anomaly
The main etiological factor in the occurrence of such an anomaly as an additional chord in the heart of a child is genetic predisposition. The risk increases if the mother has cardiac pathology. But experts do not exclude other reasons for the development of small cardiac anomalies:
- consumption of alcoholic beverages;
- smoking;
- viral and bacterial infections;
- stress;
- excessive physical activity;
- malnutrition;
- environmental pollution;
- radiation.
An abnormality of connective tissue is closely related to its dysplasia. The formation of the fetal cardiovascular system ends by the eighth week of intrauterine development. Obstetricians and gynecologists know that the blood of the unborn child circulates independently already on the 26th day of pregnancy, heart valves are formed at the 6th week, therefore it is in the first trimester that a woman needs to be especially careful about adverse effects.
Treatment of the disease
If the false chord is not life-threatening and does not affect health, preventive monitoring by a cardiologist is indicated. Moreover, treatment as such is usually not prescribed - the patient regularly visits a specialist every 3-6 months.
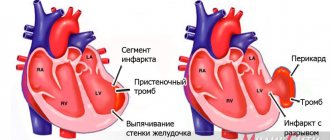
If the situation is dangerous and the chord threatens the functioning of the heart (can lead to cardiac arrest), surgical intervention is indicated to remove it. Such a decision is made if the functioning of the heart is severely impaired, causing regular disruptions in the distribution of blood flow.
It is also allowed to use folk remedies (in consultation with the doctor):
- Take a handful of raisins every day in the morning (on an empty stomach);
- take valerian decoctions;
- drink tea based on peppermint or calendula flowers.
Treatment
As a rule, single LVDC without clinical manifestations do not require treatment. Medicines are prescribed for the development of complications and concomitant heart pathologies. Symptomatic therapy - antiarrhythmic drugs and substances that correct hemodynamics: diuretics, antihypertensives, antioxidants, potassium and magnesium preparations.
Surgical treatment methods (local cryodestruction and excision of left ventricular ventricle) are rarely used: if an abnormal cord causes arrhythmia that threatens the patient’s life.
Lifestyle recommendations:
- give up fast food and sugary carbonated drinks;
- spend at least an hour a day in the fresh air;
- do not sit too long at the computer;
- find time in your personal schedule for physical exercise;
- learn to cope with stress;
- get vaccinated against influenza and other infectious diseases in a timely manner;
It is imperative to discuss the issue of “bad habits” with your teenager. It is important that the young person consciously considers it unacceptable for himself to take a sip of a low-alcohol drink or inhale cigarette smoke.
Pregnancy is not contraindicated for women with LVDC. It does not pose a threat to health, passes without negative consequences for mother and child, you just need to notify the doctor about the existing additional chord.
Arrhythmogenic right ventricular dysplasia
Terminology
Arrhythmogenic right ventricular dysplasia (ARVD) is a relatively rare cardiac disease, regarding which many questions and conflicting ideas remain to this day.
The first clinical description belongs to the outstanding Italian thinker, doctor, anatomist Giovanni Maria Lancisi (all other transcriptions of the Italian surname Lancisi, namely “Lancisi”, “Lancisi”, etc., are incorrect). He also wrote avant-garde works for that time (XVII-XVIII centuries) on the neuro-brain organization, on malaria, on the connection between syphilis and vascular aneurysms, and on epizootics in cattle. The date of writing the cardiological study “De Motu Cordis et Aneurysmatibus”, where J.-M. Lancisi described in detail ARVD as a hereditary disease in four generations of one family, domestic sources call it either 1736 or 1745, without any reservations regarding the fact that Lancisi himself died in 1720. In fact, the publication was posthumous and was published in 1728.
All this may seem unimportant, but there are other ambiguities regarding arrhythmogenic pancreatic dysplasia. The modern formulation of the diagnosis of ARVD was proposed only in 1977, but already five years later (1982) the synonymous diagnosis “arrhythmogenic right ventricular cardiomyopathy” came into use, which is used, in particular, in ICD-10 (heading “Other heart diseases / Cardiomyopathies” ). The disease is usually called hereditary, but often in the same text it is reported that the genetic factor is traced in less than half of the cases. Epidemiological data are incomplete and inaccurate; arrhythmogenic pancreatic cardiomyopathy is classified as a rare disease, but it is the second most common cause of sudden cardiac death at a young age.
The essence of this pathology is that the parenchymal (functional, specialized) tissue of the right cardiac ventricle is gradually replaced by fatty and connective tissue; this steato-fibrous process is usually localized in the “triangle of dysplasia”, the vertices of which are the apex of the heart, the inlet and outlet valves of the ventricle. Statistical estimates of occurrence in the general population vary very widely, with a range of two orders of magnitude: from 0.01% to almost 1% (the latter applies to the Mediterranean region, where ARVD is recorded much more often). Men predominate among those affected - again, some authors limit themselves to this statement, others talk about a threefold predominance. Only one case out of five is diagnosed over the age of 40, the remaining 4/5 occur in children and young people. Sudden cardiac death in 25-26% of people under 20 years of age is caused by arrhythmogenic cardiomyopathy of the pancreas. Similar statistics (25%) are observed in athletes who suddenly died. In total, in the age group under 40 years, ARVD as a direct cause of cardiovascular mortality is detected in 20% of cases. However, it should be emphasized that all these data were obtained from small samples; Of course, they need clarification, and the disease itself needs intensive further research (which is currently being carried out), since until recent decades the clinical and medical-social relevance of this problem, apparently, was seriously underestimated.