Supraventricular extrasystole - symptoms and treatment
NVE may be benign. In this case, the risk of sudden death is very low, sometimes the patient does not even feel the rhythm disturbance. Such extrasystole does not always require treatment.
If possible, the etiological factor must be eliminated:
- normalize sleep;
- limit or completely stop taking provoking medications and drinks;
- quit smoking:
- normalize thyroid function in hyperthyroidism;
- adjust the level of potassium in the blood;
- remove the gallbladder in case of cholelithiasis;
- Avoid a horizontal position after eating if you have a hiatal hernia;
- normalize blood pressure;
- increase physical activity according to the body’s capabilities;
- Avoid excessive physical activity (weightlifting, heavy lifting).
The patient is advised to establish a daily routine. The diet should be supplemented with foods rich in potassium and magnesium; they have a beneficial effect on the cardiovascular system.
| Products containing potassium | Products containing magnesium |
| ⠀•⠀dried apricots; ⠀•⠀cocoa powder; ⠀•⠀wheat bran; ⠀•⠀raisins; ⠀•⠀sunflower seeds; ⠀•⠀nuts (pine nuts, almonds, peanuts, walnuts); ⠀•⠀legumes (peas, lentils, beans); ⠀•⠀jacket potatoes; ⠀•⠀avocado; ⠀•⠀ceps; ⠀•⠀bananas; ⠀•⠀citrus fruits; ⠀•⠀Brussels sprouts and kohlrabi; ⠀•⠀milk and fermented milk products; ⠀•⠀cereals (oatmeal, buckwheat, pearl barley, rice); ⠀•⠀fruits (peaches, pears, watermelon, apples, prunes, apricots, melon); ⠀•⠀chicory; ⠀•⠀vegetables (carrots, spinach, green onions, eggplant, cucumbers); ⠀•⠀chicken eggs; ⠀•⠀fish and meat; ⠀•⠀apple juice. | ⠀•⠀oil (sesame, flaxseed, peanut); ⠀•⠀cheese (Dutch, Poshekhonsky, goat, with mold); ⠀•⠀cottage cheese (low-fat and low-fat, curd cheese); ⠀•⠀bitter chocolate; ⠀•⠀almost all types of meat; ⠀•⠀fish (halibut, sturgeon, perch, haddock, cod, saury); ⠀•⠀duck eggs; ⠀•⠀cereals (rolled oats, chickpeas, peas, buckwheat, brown rice, lentils); ⠀•⠀fruits and berries (cherries, kiwi, pineapple, feijoa, raspberries, pears, peach, persimmon); ⠀•⠀many varieties of tea (for example, “Ivan-tea”) and juices; ⠀•⠀ginger; ⠀•⠀mustard; ⠀•⠀vanilla. |
Indications for antiarrhythmic therapy are:
1. Poor tolerance of supraventricular extrasystole. In this case, it is necessary to determine in what situations and at what time of day heart rhythm disturbances most often occur, and then time the drug intake to this time.
2. The occurrence of VVC (not necessarily frequent) in patients with heart defects (primarily mitral stenosis) and other organic heart diseases. In such patients, atrial overload and dilatation progress. Supraventricular extrasystole in this case serves as a harbinger of the occurrence of atrial fibrillation.
3. Supraventricular extrasystole, which arose as a result of a long-term etiological factor in patients without previous organic heart disease and atrial enlargement (with thyrotoxicosis, inflammatory process in the heart muscle, etc.). If antiarrhythmic treatment (along with etiotropic treatment) is not carried out, the risk of persistent EVE increases. Frequent supraventricular extrasystole in such situations is potentially malignant in relation to the development of atrial fibrillation.
4. Frequent (700-1000 extrasystoles per day or more) EVA also requires antiarrhythmic therapy, even if it is regarded as idiopathic, since there is a risk of complications. The approach in these cases should be differentiated. It is also possible to refuse antiarrhythmic therapy if there are reasons for this:
- absence of subjective symptoms and complaints;
- borderline number of extrasystoles;
- intolerance to antiarrhythmic drugs;
- signs of sick sinus syndrome or impaired AB conduction.
Antiarrhythmic drugs used for EVA:
- Beta blockers (Metoprolol, Bisoprolol), calcium antagonists (Verapamil). It is pathogenetically justified to prescribe drugs from this group to patients with hyperthyroidism, a tendency to tachycardia, when EVE occurs against the background of stress and is provoked by sinus tachycardia. Beta blockers are indicated for ischemic heart disease, arterial hypertension, and sympathoadrenal crises. "Verapamil" is prescribed for concomitant bronchial asthma, variant angina, nitrate intolerance, and patients with coronary artery disease.
- “Belloid”, “Teopek” are indicated for patients with vagal-mediated VHE, which develops at night against the background of a decrease in heart rate. These drugs increase the rhythm and are prescribed at night.
- Sotalol (“Sotalex”, “Sotagexal”). It is necessary to select a dose depending on blood pressure and heart rate, the duration of the PQ and QT intervals. Indicated for a combination of ventricular extrasystole and ventricular extrasystole.
- Antiarrhythmics of IA and IC classes (“Dizopyramide”, “Allapinin”, “Propanorm”, “Etatsizin”). Use is not indicated in patients with coronary artery disease who have recently suffered a myocardial infarction due to its arrhythmogenic effect on the ventricles.
- Amiodarone (“Cordarone”). Amiodarone is the most effective antiarrhythmic drug available. Can be prescribed to patients with organic heart damage.
- If monotherapy is insufficiently effective (i.e., using one antiarrhythmic), combinations of drugs can be used.
If the prescribed therapy has a good effect, antiarrhythmics should not be discontinued quickly. Treatment lasts several weeks (months). If there is a threat of developing atrial fibrillation or if there are episodes of it in the anamnesis, NVE therapy is carried out for life. In the case of continuous antiarrhythmic therapy, the minimum effective doses are selected. Patients with an undulating course of EVE should strive to discontinue the antiarrhythmic during periods of improvement (excluding cases of severe organic myocardial damage). The withdrawal of antiarrhythmics is carried out gradually with a decrease in dosage and number of doses per day. After discontinuation, the patient is recommended to have the drug with him (the “pill in his pocket” strategy) for the purpose of rapid administration when the arrhythmia resumes [11].
If there is no effect from antiarrhythmic therapy, with frequent NVE (up to 10,000 per day), the issue of surgical treatment is considered - radiofrequency ablation of arrhythmogenic foci (destruction of foci using electric current) [5].
Classification
Supraventricular arrhythmia is a general name for a number of pathologies that manifest as disturbances in heart rhythm. They differ in symptoms and require different treatment regimens. For a more accurate diagnosis, a classification is used that identifies several types of supraventricular arrhythmias:
- extrasystole;
- tachycardia of various types;
- accelerated supraventricular rhythms;
- atrial flutter and fibrillation.
REFERENCE! The most common types of supraventricular heart rhythm disturbances are extrasystole and sinus tachycardia. They can be diagnosed even in a healthy person of any gender and age.
Other violations
Supraventricular heart rhythm disorders are a huge group of pathologies that includes various diseases. The most commonly diagnosed of them are extrasystole and tachycardia, but less common disorders are also identified.
- Ventricular preexcitation syndrome is caused by the formation of additional (pathological) pathways that block the conduction of impulses along the normal atrioventricular pathway. There are several types of such pathways, but they all lead to disruption of the processes of normal polarization and depolarization of the ventricles.
- Sinus bradycardia is a decrease in heart rate. It can reach 50-60 beats per minute or less, while it remains correct.
- Sick sinoatrial node syndrome is a typical disorder in which organic damage to this area is observed. As a result, the patient develops persistent bradycardia, and the pulse does not increase even after physical exertion or the use of atropine.
Most pathologies have a benign course. In some cases, they are chronic and require constant monitoring.
Prevention of supraventricular arrhythmia
There are certain principles for the prevention of rhythm disturbances that apply to all forms of arrhythmia, including supraventricular;
- Proper nutrition should consist of lean meats, fish, and a sufficient amount of plant foods should be included in the diet.
- Physical activity must be at an acceptable level for the patient so that the heart is supplied with sufficient oxygen and nutrients.
- Maintaining blood glucose and total cholesterol levels within normal limits. Also, body weight must correspond to age and physiological norms.
Video Therapy of extrasystoles and supraventricular tachyarrhythmias
4.75 avg. rating ( 93 % score) - 4 votes - ratings
Description of supraventricular arrhythmia
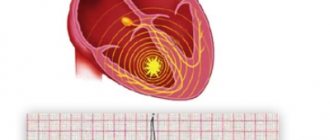
Supraventricular arrhythmia (SVA) is also defined as atrial or supraventricular. The source of the spread of extraordinary contractions is in the atria, that is, above the ventricles, hence the name of the pathology.
The formation of NFA is based on the formation of a pathological focus of trigger activity, which sends periodic extraordinary impulses. In some cases, the electrical signal is transmitted through the atria or in the atrioventricular node via the reentry mechanism, then a cyclic propagation of the impulse is observed, leading to an acceleration of cardiac activity.
The development of supraventricular arrhythmia can occur against the background of cardiovascular diseases, which is typical for old age, or without visible clinical signs during the formation of the body, that is, in children and adolescents.
If the pathology is associated with other cardiovascular disorders, then it is important to undergo regular examinations with a cardiologist. Otherwise, you will have to find out the dangers of supraventricular arrhythmia from your own experience.
Symptoms of supraventricular arrhythmia
All types of NDA are characterized by the following general manifestations:
- disruptions in cardiac activity in the form of increased rhythm (tachycardia), interrupted rhythm (extrasystole) or decreased rhythm (bradycardia);
- discomfort in the sternum;
- a feeling of palpitations or the heart turning over in the chest, jumping out of the chest.
Further, to the given symptoms, manifestations specific to the underlying disease are added. With neuroses, panic attacks or vegetative-vascular dystonia, this may include increased sweating, a feeling of heat in the body, irritability, fear of death and anxiety. With heart failure, you feel weak, dizzy, and cardialgia (heart pain) may appear. Hypertension is characterized by increased blood pressure, tinnitus, and “pounding in the temples.”
Only a doctor can make a competent substantiation of the involvement of supraventricular arrhythmia in a particular disease.
Asymptomatic NVA is mainly associated with functional disorders. These may be the same VSD or neuroses.
Particular attention should be paid to arrhythmias that occur in the following cases:
- In case of hormonal disorders (pregnancy, menopause, adolescents), arrhythmia is observed both at rest and during physical or emotional stress. Also, pathology of the thyroid gland and bronchopulmonary system can contribute to disruption of the heart.
- After a heavy meal, the parasympathetic nervous system begins to predominate and, against the background of its activity, a malfunction of the heart occurs. The condition worsens when taking a horizontal position immediately after eating.
You should consult a doctor not only with pronounced supraventricular arrhythmia. When determining the asymptomatic course of the disease, you should also undergo periodic examinations with a cardiologist or arrhythmologist.
Diagnosis of supraventricular arrhythmia
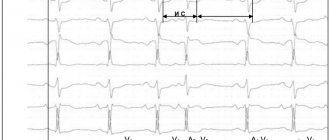
Electrocardiography is one of the main methods for examining patients for arrhythmia. Provides detailed data on the nature of the rhythm disturbance, the location of the outbreak, and heart rate. The research takes a little time - up to 10 minutes. The safety of the study is very high, so it is allowed to conduct it from one month.
Interpretation of the ECG makes it possible to identify almost all forms of supraventricular arrhythmia, the number of foci, their location, and the time of occurrence of extrasystole. The wide availability of this diagnostic method makes it indispensable during medical examinations and medical examinations, during which most of the NFA are determined.
The main ECG signs of supraventricular arrhythmia:
- an altered P wave, in the figure it is shown negative, it may also be double-humped or otherwise deformed;
- the distance between RRs is different and may decrease or, on the contrary, increase;
- Heart rate according to the cardiogram most often increases, more than 100 times per minute.
Daily ECG monitoring involves placing sensors on the patient in the chest area, which are connected to a recording device. The purpose of the procedure is to record the heart rhythm in a day or several days and then decipher it using special programs. This makes it possible to identify rare attacks that may not be detected on a standard ECG.
Echocardiography is a modern diagnostic method that works on the basis of ultrasound. When using echocardiography, the organic and functional state of the heart and blood vessels is assessed. For example, using ultrasound, the thickness of the atria is determined, which in normal condition on the left side should be no more than 4 cm.
Classification of supraventricular arrhythmia
The pathology is quite variable, so it is divided according to the nature of its manifestation into three types: tachycardia, bradycardia, extrasystole.
All extrasystoles differ in frequency, location and number of ectopic foci, as well as the time of occurrence of the attack.
By frequency
The frequency of premature contractions, which are counted per minute, divides all extrasystoles into:
- single - there are no more than five extrasystoles;
- paired - the ECG shows two extrasystoles located one after the other;
- group - premature contractions occur several in a row;
- multiple - more than five extrasystoles are determined.
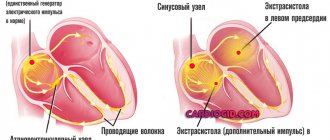
According to the location of the outbreak
It can be determined directly in the atria or in the atrioventricular node. In any case, they talk about supraventricular arrhythmia.
Atrial arrhythmias are localized in the corresponding part of the heart
Atrioventricular arrhythmias are characterized by the location of an ectopic focus in the septum located between the atria and ventricles.
By number of outbreaks
When determining one ectopic focus using special research methods, they speak of monotopic extrasystole.
The presence of two or more pathological foci indicates polytopic extraordinary cardiac contractions.
By time of occurrence
Using an ECG, the time period during which the extraordinary contraction occurs is determined. There are three types of extrasystoles, distinguished by the time of formation:
- early - occur at a time when the atria contract;
- interpolated - the localization site is at the junction of the contractions of the atria and ventricles;
- late - characteristic of the period of ventricular contraction; they can also form during relaxation of the heart (in diastole).
Causes of supraventricular arrhythmia
It was noted above that in the development of arrhythmia the primary role is played by a provoking factor, which can have a functional or organic origin.
Functional reasons:
- autonomic dysfunctions;
- excessive consumption of alcoholic and caffeinated drinks;
- irregular work schedule with insufficient rest;
- hormonal disorders (most often in women and adolescents);
- infectious processes accompanied by high fever.
Organic reasons:
- heart defects;
- myocarditis and endocarditis
- postoperative disorders;
- traumatic heart lesions;
- tumor processes located in the heart area;
- pulmonary heart disease, which developed against the background of pulmonary hypertension.
Some metabolic disorders, such as a lack of potassium, magnesium, and renal failure in the blood, can also contribute to the development of NFA.
The use of cardiac glycosides, sympathomimetics, theophylline and antiarrhythmic drugs in incorrect doses can cause supraventricular arrhythmia.
If the patient has a state of hypoxia, which often occurs with anemia, heart failure and bronchopulmonary pathology, the activity of the heart can be disrupted by the type of arrhythmia localized in the atria.