Heart blocks are pathological conditions in which the conduction of nerve impulses inside the heart muscle is disrupted or completely stopped. In a normal heart, electrical impulses occur at a certain frequency in the natural pacemaker, the so-called. sinus node. The impulse originating in the sinus node spreads through the conduction system of the heart, passing through the atria and ventricles. The function of the conduction system is to ensure coordinated work of different parts of the heart, ensuring maximum contraction efficiency.
Why does the disorder develop?
There are many different conditions that can disrupt the conduction of electrical impulses through the myocardium.
We cannot always accurately determine the cause of this phenomenon. Often we can only guess why the blockade occurred and try to slow down the progression of the process. In clinical cardiology, it is customary to distinguish two groups of cardiac conduction and excitability disorders:
- Cardiac, that is, caused by pathological processes occurring in the heart muscle. This may be coronary heart disease (CHD) or previous myocardial infarction, inflammatory diseases, cardiomyopathies. Often the source of the problem is congenital and acquired heart valve defects. Failure of the conduction system can be caused by tissue trauma during surgery.
- Non-cardiac - the cause of such disorders lies outside the myocardium. Most often we have to deal with endocrine diseases - diabetes and thyroid pathology. Among the possible causes, it is also worth highlighting hypertension, chronic bronchitis, asthma and other conditions leading to the development of hypoxia. In women, failure is often recorded during pregnancy, with the onset of menopause.
It is important to understand: the occurrence of blockade is not always associated with organic changes in the myocardium or serious non-cardiac diseases. Heart failure can be a temporary phenomenon due to stress or physical activity. The nature of the disorders can be determined by examining the patient.
Forecast
Heart block can be congenital) but most often develops after birth. In general, the risk of acquired heart block increases with age, as does the incidence of cardiovascular disease.
First-degree heart block is common in well-trained athletes, adolescents, young adults, and individuals with a highly active vagus nerve. People with various heart conditions, including coronary artery disease, rheumatic heart disease, sarcoidosis, or other structural heart disease, are also at risk of developing first-degree heart block.
Without proper treatment, second-degree Mobitz blocks and third-degree blocks can be accompanied by symptoms that significantly impair the quality of life: constant fatigue, chest pain, severe dizziness and fainting. Without treatment, complete cardiac arrest can result.
Mechanism of occurrence
Normally, electrical impulses pass through the myocardium at a certain speed and in a strictly established sequence. The signal path begins in the right atrial appendage - in the sinus node. From here, the excitation gradually spreads through the tissues of the atria and slows down briefly in the atrioventricular node. Next, the impulse spreads along the branches of the His bundle, which cover the right and left ventricles. The conducting system ends with small Purkinje fibers.
The problem occurs when the conduction of the impulse slows down or is completely blocked at a certain point. The cause may be functional and organic changes. In the first case, the impulse reaches cells that are in the refractory (inactive) phase - and its further passage is disrupted. The next signal can travel through the tissues without obstruction. With organic changes (for example, in the case of scar formation after a heart attack), the impulse will “stumble” over an obstacle, and the failure will become persistent.
If we talk about the pathophysiology of disorders, we should note the work of Na+ channels in cardiomyocytes. As long as these pathways are open, the impulse can penetrate the cells without obstacles. But, if the channels are inactivated, the signal transmission slows down or stops. This happens, for example, in the zone of myocardial ischemia - where the blood supply to the tissues stops.
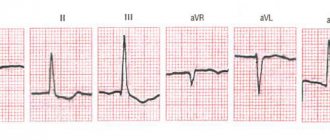
Signs of heart block are nonspecific and are not always noticeable without special examination. The problem can be identified using an ECG. The film shows how the impulse travels through the heart muscle, whether there are obstacles to tissue excitation, and in which zone they are localized. Electrocardiography is the main method for making a diagnosis and prescribing treatment.
Diagnostics
Diagnosis of heart block begins with an interview and physical examination of the patient. Medical history and family history are studied. The patient's symptoms and lifestyle are examined. Medicines that the patient may have taken are checked.
Testing is carried out using a Holter or event monitor - devices that track heart rhythm over a certain period of time.
Figure 2. Signs of heart block.
A Holter monitor is used to study the heart over 24 or 48 hours. Event monitor - for a month or more. They allow changes in heart rate to be recorded even if they do not occur frequently or predictably.
An implantable loop recorder, a small heartbeat recorder that is placed under the skin over the heart, may be used. Capable of analyzing heart function for up to 2 years.
Basic methods of studying the functioning of the heart are used, such as electrocardiography (ECG) and electrophysiological studies. To diagnose heart diseases of a child in the womb, the ultrasound method is used.
Holter monitor. Photo: yupachingping / freepik.com
Possible symptoms
Clinically, heart blocks are not always evident. With mild disorders, the patient may not have any complaints. A malfunction in the functioning of the heart is detected only on an electrocardiogram.
With progressive conduction disturbances, the following symptoms occur:
- causeless weakness;
- labored breathing;
- dyspnea;
- interruptions in heart function;
- heart rate slowdown;
- dizziness.
If several impulses in a row do not pass through the tissues of the heart, loss of consciousness is possible. Over time, the disease progresses, the patient's condition worsens, and such attacks occur more often.
Types of blockades and their signs on the ECG
In cardiology, various classifications of cardiac conduction disorders are proposed. In practice, it seems convenient to us to separate all pathological processes by location. The following types of blockade are distinguished:
- Sinoatrial. The failure is localized in the region of the sinus node - at the very beginning of the impulse path.
- Interatrial. The passage of the signal slows down between the atria.
- Atrioventricular (AV block). The transmission of impulses between the atria and ventricles slows down or stops.
- Intraventricular. There is a failure in signal transmission along the branches of the His bundle in the ventricles of the heart.
These conditions can be distinguished using an ECG. Characteristic signs of pathology are presented in the table.
| Type of blockade | Signs on ECG |
| Sinoatrial | Sinus rhythm is abnormal. There are long pauses and loss of individual heart contractions. The appearance of bradycardia is characteristic |
| Interatrial | Change in the P wave – expansion for more than 0.12 seconds, deformation. Can be combined with PQ interval prolongation |
| Atrioventricular | Prolongation of the PQ interval, loss of the QRS complex |
| Intraventricular | Widening and deformation of the QRS complex |
Let us dwell in more detail on atrioventricular blocks. According to the clinical course, it is customary to distinguish 3 stages of development of the process.
First degree heart block is characterized by slow passage of electrical impulses from the atria to the ventricles. The ECG shows an expansion of the PQ interval to 0.2 seconds. – it reflects the speed of signal transmission through the atria. This is the most common AV conduction disorder. It occurs mainly in old age against the background of organic pathology - a previous heart attack, myocarditis, heart defects.
Second degree heart block occurs as the process progresses. Not all impulses travel to the ventricles. Changes in the ECG are determined by the type of blockade:
- Mobitz type 1 AV block leads to loss of ventricular contractions. On the cardiogram this can be seen by the lengthening of the PQ interval, and the changes progress with each complex. Next, only the P wave is recorded, and the QRS, a marker of ventricular function, drops out. Such symptoms are observed with a heart attack, overdose of cardiac glycosides, etc.
- Mobitz type 2 AV block on the ECG is indicated by a loss of QRS. The PQ interval lengthens, but its increase does not progress. This symptom indicates serious damage to the heart muscle and threatens the development of complete heart block.
If the process continues to progress, several ventricular contractions in a row are blocked, and QRS complexes occur two or more times. The patient experiences Morgagni-Adams-Stokes (MAS) attacks with loss of consciousness.
III degree violations are complete transverse heart block. The signal does not travel from the atria to the ventricles. Separate excitation of the upper and lower parts of the heart is recorded. Changes in the ECG are chaotic, dissociation is visible between the markers of atrial and ventricular contractions - PQ and QRS. Often this condition is combined with intraventricular block.
Consequences
Bundle branch block requires timely diagnosis, since if left untreated, the disease causes serious consequences, sometimes incompatible with the patient’s life. Among them are:
- tachycardia;
- ventricular fibrillation;
- thromboembolism;
- heart failure;
- heart attack;
- stroke;
- sudden death.
To prevent these complications, it is recommended to undergo regular preventive medical examinations. If heart pain, shortness of breath and other signs of the disease appear, you should contact a specialist immediately.
Doctor's advice: how to properly see a doctor if there is a blockage
After the diagnosis is established, the patient remains in outpatient treatment or is hospitalized in a hospital. Tactics are determined by the severity of the blockade. After achieving remission, the patient should not be left without specialist supervision. We recommend:
- If your condition is stable and there are no complaints, visit a cardiologist and do an ECG every 6 months.
- If the condition worsens, new complaints appear or existing disorders progress, make an appointment with a doctor as soon as possible.
If the doctor prescribes drug therapy, you should adhere to it and not violate the drug dosage schedule. Stopping the medication on your own is unacceptable - this leads to the development of complications.
If the patient has had a pacemaker installed, the monitoring tactics change. You should visit your doctor 3, 6 and 12 months after surgery to make sure that the device is working smoothly. The further observation schedule will depend on the patient’s condition.
Treatment approaches
When choosing a treatment regimen, we focus on the protocols adopted by the Ministry of Health and clinical recommendations of domestic and foreign communities. Treatment must be comprehensive and rational. It is necessary not only to remove the symptom, but also to eliminate the possible cause of the problem - and prevent the development of complications.
Moderate disturbances of intraatrial and intraventricular conduction do not require treatment. We suggest that the patient be regularly monitored by a cardiologist, monitor his well-being, and lead a healthy lifestyle. Drug therapy is prescribed for obvious clinical symptoms - the appearance of interruptions in heart function, shortness of breath, dizziness and other conditions that interfere with leading a normal lifestyle. If dangerous complications develop, surgical treatment is indicated.
Let us dwell in more detail on the treatment of AV block. The treatment regimen will depend on the severity of the patient's condition. If, after the diagnosis, the ECG reveals first-degree AV block, therapy is not indicated. It is recommended only to be monitored by a specialist - visits to the doctor at least once a year.
If second-degree AV block of the Mobitz type 1 is detected, treatment should be comprehensive. To stabilize the conduction system of the heart, antiarrhythmic drugs are prescribed. At the same time, treatment is carried out for the underlying disease that caused the heart failure. No specific therapy is provided here. We select medications based on the leading symptoms and concomitant diseases.
Mobitz 2nd degree AV block and complete heart block are reasons for surgical treatment. A pacemaker is being implanted. The device regulates the heart rhythm, ensures proper transmission of signals and uninterrupted functioning of the myocardium. A pacemaker may also be offered to a patient with Mobitz type 1 AV block if severe symptoms are present.
Emergency care is indicated for the development of MAS syndrome and complete heart block. The patient must be hospitalized in a hospital. Indirect cardiac massage is performed and medications are prescribed to maintain a stable rhythm. The installation of a pacemaker is shown.
Lifestyle and precautions
Treatment and prevention of heart problems is not only about taking medications or undergoing surgery. We recommend that the patient completely change his attitude towards life. To prevent the progression of the disease and avoid undesirable consequences, you should:
- Change your diet. The daily menu should contain less fried, spicy and salty foods. It is recommended to add products of plant origin, focusing on fresh vegetables and fruits. Fast food and quickly digestible carbohydrates are prohibited - they negatively affect metabolism and provoke the development of cardiovascular pathology.
- Exercise. Aerobic exercise, yoga, and swimming are recommended. If it is not possible to visit a fitness club or gym, you can walk in the fresh air every day - at least 30 minutes a day.
- Don't overexert yourself. Working too hard will not be good for your heart. It's worth reconsidering your daily routine. Night sleep should be at least 8 hours.
- Avoid stress. Excessive worries negatively affect the functioning of all internal organs, and the heart is no exception.
- Watch your weight. If you are overweight or obese, you should consult an endocrinologist and create a diet.
- To refuse from bad habits. Smoking is prohibited. You should not abuse alcohol.
The prognosis of the disease depends on the severity of the patient's condition. Compliance with all doctor’s recommendations and timely installation of a pacemaker will prolong life and maintain health.
Case from practice
Patient R., 75 years old, turned to his local doctor with complaints of interruptions in his heart function.
Upon examination and history taking, it turned out that the patient was also bothered by headaches, attacks of dizziness, and shortness of breath during exercise and at rest. Considers himself sick for 10 years. Suffered a myocardial infarction at the age of 67 years. She is seen by a cardiologist with a diagnosis of coronary artery disease. Post-infarction cardiosclerosis. After further examination, ECG revealed signs of second degree AV block, and echoCG revealed left ventricular hypertrophy. After consultation with a cardiologist, the patient was referred to the cardiac surgery center. A pacemaker was installed. The patient was discharged with improved condition. Observation by a cardiologist is recommended.
Advantages
Excellent technical base
Powerful equipment - expert class ultrasound machines with 3D scanning capabilities, monitors/defibrillators, Holter monitors, as well as our own laboratory make it possible to accurately determine the causes of pathology and monitor the progress of treatment.
Highly qualified personnel
A complete examination of patients and treatment is carried out by experienced cardiologists, arrhythmologists, therapists, and functional diagnostics doctors. Candidates of Medical Sciences, doctors of the highest category are regular participants in European and domestic congresses of cardiologists, as well as participants in international clinical studies, and have numerous publications in scientific journals.
Modern diagnostic methods
To diagnose the disease, extensive laboratory testing, ECG at rest, with stress and 24-hour Holter ECG monitoring, ultrasound, Doppler and Duplex examination of the carotid arteries are performed. If necessary, it is possible to conduct an ECG at home using a portable device.