Published: 07/07/2021 11:15:00 Updated: 07/07/2021
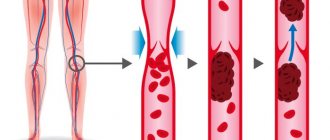
Thrombosis is a complete or partial blockage of the lumen of a vessel by a parietal or mobile thrombus. A thrombus is a dense blood clot that appears as a result of a change in its fluidity. Normally, thrombus formation is a protective mechanism. Damage to the vascular wall leads to a slowdown in blood flow and accumulation of platelets around the damage. The thrombus literally “darns” the wall of the vessel.
The classic causes of thrombosis are described by Vikhrov’s triad: damage to the vascular wall, slowing of blood flow and changes in blood properties [3]. Some blood clots (they are called emboli) are able to move to narrower areas of the vessel, which are completely or partially blocked. Every year, about 25 million people die from thrombosis, and even more face trophic disorders caused by blood clots [3].
Types of vascular thrombosis
The most common thrombosis of the lower extremities, however, the greatest danger is pulmonary embolism - PE - and disseminated intravascular coagulation syndrome - DIC syndrome.
Arterial thrombosis develops when its lumen is blocked by a thrombus or embolus. Clinical signs are determined by the location where the blockage occurs, an organ or tissue that has little or no blood supply. If blockage with impaired vessel patency occurs slowly, “spare” collateral vessels open, which mitigates the clinical symptoms of arterial thrombosis [3]. Arterial thrombosis occurs more often in middle-aged and elderly men [7].
Vein thrombosis varies depending on the location of the lesion into deep or superficial vein thrombosis and pulmonary embolism. Among all cardiovascular pathologies, venous thrombosis ranks third in frequency of occurrence, second only to ischemic heart disease and atherosclerosis. The third place in the structure of causes of mortality is occupied by pulmonary embolism. Starting at age 40, the risk of developing venous thrombosis doubles every 10 years [5].
Two variants of damage to the veins of the lower extremities are described: phlebothrombosis (primary thrombosis, the thrombus is not firmly fixed) and thrombophlebitis (secondary thrombosis due to inflammation of the vessel wall, the thrombus is firmly fixed) [6]. Thrombophlebitis is more often associated with superficial vein thrombosis [2]. The larger the vein affected by thrombosis, the more pronounced its clinical manifestations. The surrounding tissues are compressed by stagnation of blood, since the blood stays at the site of occlusion, but does not move towards the heart. Venous blood clots tend to break off and travel through the bloodstream (thromboemboli). When they enter vital organs, life-threatening conditions develop [3].
Symptoms
Clinical manifestations of a stationary thrombus are much less pronounced. The patient is rarely bothered by:
- tachycardia;
- shortness of breath when sitting.
In case of mobility in the left atrium, the following are observed:
- excruciating attacks of palpitations, when heart tremors shake the entire chest (what clinicians call “frantic”);
- release of cold sticky sweat;
- sharp pallor with cyanosis of lips and fingers;
- fainting states.
During an attack, the pulse in the radial artery is not detected or is sharply weakened. During auscultation, previously heard noises may disappear. A spherical thrombus or one attached to a “leg” is characterized by symptoms of deterioration in a sitting position, when it descends and clogs the venous opening.
Bringing the patient into a supine state significantly improves well-being.
The duration of attacks of loss of consciousness varies individually: from a few seconds to two hours.
Cardiac surgeons pay attention to the role of irritation of the atrial appendage zone in the reflex spasm of cerebral vessels, since subsequent removal of the blood clot shows that due to its size it could not block the blood flow.
Signs of thrombosis in a patient with heart disease may include:
- persistent heart failure that responds poorly to treatment;
- severe shortness of breath, cyanosis of the arms and legs, tachycardia, yellowing of the skin;
- formation of pulmonary hypertension.
Risk factors for thrombosis
Internal:
- arterial hypertension [7];
- pregnancy, childbirth, postpartum period [3];
- biochemical changes in blood [2,3,5,7];
- vasculitis [2];
- age over 40 years [5];
- congenital thrombophilia, thrombosis, varicose veins of the lower extremities [3,5];
- congestive heart failure [5, 6];
- malignant neoplasms, radiotherapy and chemotherapy [3];
- strokes [3, 6];
- myeloproliferation [2, 5, 7];
- nephrotic syndrome and renal failure [5, 6, 7];
- obesity (BMI over 30) [3];
- myocardial infarction [6];
- diabetes mellitus [6, 7];
- systemic lupus erythematosus [2];
- chronic pulmonary diseases [3];
- enterocolitis [5].
External:
- heroin addiction [2];
- hormonal therapy [3,5];
- dehydration due to vomiting, diarrhea, increased sweating, direct lack of fluid [6];
- immobilization [3];
- travel by plane, bus or in a seated car [3];
- infectious diseases, including COVID-19 [1, 3, 5, 9];
- catheterization of central and peripheral veins [2, 5];
- smoking [6, 7];
- sedentary lifestyle [3];
- operations [3];
- fractures of large bones, other injuries [3];
- taking oral contraceptives [5];
- taking Diazepam, Amiodarone, Vancomycin [2];
- sclerotherapy and thermal ablation [2];
- condition after joint replacement [3];
- holding an awkward position [3].
Who is at risk?
Those who are most likely to develop thrombosis are people who are obese and have varicose veins, women who take oral contraceptives, and those who take many long flights. But a high risk of blood clots occurs when all these factors are combined.
“Patients with obesity and varicose veins are at risk. As for medications, in particular oral contraceptives, now most of them are well balanced and we rarely see the development of thrombosis and thromboembolism in women taking these drugs. People with a sedentary lifestyle, impaired hemostasis, namely blood clotting disorders, also fall into this group. If the patient has all these provoking factors, then the risk of developing thrombosis increases. Age also makes it worse. Over the years, the vessels lose elasticity and become brittle, plus a number of concomitant diseases cause swelling of the lower extremities,” says Shpachenko.
Thrombosis Clinic
Symptoms of thrombosis can be general, regardless of location, or specific.
Common symptoms include pain with movement and at rest, limited mobility, and decreased function of the affected organ or tissue. Symptoms of arterial obstruction (acute thrombosis, or gradual obstruction of vessel patency):
- asymmetry of blood pressure when measured on both arms [7];
- pallor of the skin, turning into cyanosis [7];
- pain at rest at night [7];
- pain when moving in the thigh, buttock, lower leg, foot, shooting or aching [7];
- sleep disorders [7];
- numbness, coldness of the limb [7];
- absence of peripheral pulsation [7];
- necrosis (necrosis) of affected tissues, trophic ulcers, gangrene [7];
- intermittent claudication [7].
Symptoms of venous thrombosis:
- pain [6];
- swelling, soft and asymmetrical [6];
- blue discoloration of the skin (skin cyanosis) [6];
- increased skin temperature of the extremities [6];
- increased sensitivity and compaction in the projection of the superficial veins [2];
- post-inflammatory hyperpigmentation [2];
- dilated saphenous veins [6];
- erythema [2].
Sometimes the only symptom of venous thrombosis is PE [6].
Briefly about the treatment method
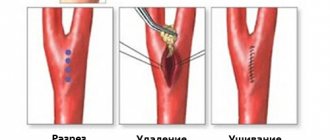
Removing blood clots (thrombectomy) can be a separate type of treatment, but more often it is a component of it. Vessel thrombosis can form as a result of its narrowing or expansion; a thrombus fragment can be brought from other arteries or the heart. Thrombotic masses in the lumen of blood vessels block blood flow and cause circulatory failure, which can lead to gangrene of an organ or limb. Modern vascular surgery has a number of technologies that make it possible to remove thrombotic masses from vessels.
Diagnosis of thrombosis
Primary diagnosis is based on a detailed history and anthropometry (calf or thigh circumference).
The Wells scale is used to diagnose acute thrombosis and diagnose pulmonary embolism [8,9]. Instrumental diagnostics include compression or duplex scanning of veins, Doppler ultrasound with compression of veins, impedance plethysmography, pulmonary angiography, radiocontrast or MRI venography [6,9], CT and MRI angiography [7,9].
To diagnose arterial thrombosis, physical tests are used (6-minute walk test, treadmill test), determination of pulsation of superficial arteries (arteries of the dorsum of the foot), duplex scanning of the arteries of the extremities, angiography (X-ray of a vessel filled with a radiopaque substance) and measurement of transcutaneous oxygen tension [ 7].
Possible complications during treatment
The following complications are possible when using a Fogarty probe:
- Rupture of the inner wall of the artery with its dissection and secondary thrombosis
- Tearing off the probe head and leaving it in the lumen of the artery
- Perforation of an altered artery wall with a probe with internal bleeding
- Complications associated with access (hematoma, lymph accumulation, wound suppuration)
Such complications are quite rare. Their frequency decreases as clinical experience with thrombectomies accumulates. In our clinic, we have not observed such complications over the past five years.
Complications of Rotarex thrombectomy:
- Dissection of the arterial wall due to rough passage of the probe
- Transfer of pieces of blood clots to small arteries below the site of thrombosis
- Formation of hematoma along the artery
Such complications are usually identified during the operation and are usually corrected immediately.
Tests for thrombosis
Laboratory indicators play a significant role in the timely diagnosis of thrombosis.
Thus, guidelines for the management of patients with a new coronavirus infection provide for stratification of the risk of coagulopathy in patients with COVID-19 based on simple laboratory tests: D-dimer, prothrombin time, platelet count, fibrinogen level [1,9]. A clinical blood test can detect inflammation. It also determines the level of platelets, that is, the very substrate of thrombosis.
Additionally, the level of inflammation in the blood and the risk of thrombosis is indicated by an increased level of C-reactive protein.
Biochemical analysis primarily demonstrates blood glucose levels. It can be used to judge the presence of diabetes, one of the most serious risk factors for thrombosis.
Also, a biochemical analysis can determine the level of protein C, which also characterizes the severity of the risk of thrombosis.
Elevated levels of homocysteine in the blood are also a currently proven risk of thrombosis, leading to miscarriage and cardiovascular events (heart attacks and strokes).
D-dimer is a laboratory marker of fibrin formation [8]. It also indicates the presence of inflammation, just like C-reactive protein. The level of D-dimer is a control indicator of COVID-19 and its complications, including those associated with thrombosis.
You can take tests under the comprehensive Thrombosis program, which includes determining the levels of Antithrombin-III, D-dimer and genetic factors of cardiac diseases and platelet levels. This program allows you to determine the fact of thrombosis occurring somewhere in the body, as well as determine the genetic predisposition to it. This program, like other tests, is offered by the CITILAB network of clinics.
Additional determination of homocysteine and C-reactive protein levels will help determine the biochemical risk of thrombosis.
Why do blood clots form in the heart?
An embolus can enter the heart cavity from other vessels in the bloodstream. But intracardiac formation of a blood clot is possible, its growth with subsequent severe harm to blood circulation.
The reasons for the primary location in the area of the atria and ventricles are:
- damage to the heart wall and valves, causing turbulence in the blood flow;
- slow blood flow;
- increased blood clotting.
Similar conditions occur in the following diseases:
- heart defects (most often a blood clot forms inside the left atrium with mitral stenosis of rheumatic etiology);
- myocardial infarction of the right and left ventricle with spread to all walls (transmural), thinning of the heart wall during scarring after a heart attack causes the formation of a sac-like protrusion (aneurysm);
- arrhythmias associated with uneven contraction of areas of the heart muscle.
The altered direction of blood flow in the atria during fibrillation contributes to thrombus formation
A significant role is played by the addition of pneumonia, tonsillitis, and influenza to the clinical course of heart and vascular diseases. In these diseases, the production of fibrin (one of the components of a blood clot) is significantly activated.
Treatment and prevention of thrombosis
Treatment of thrombosis includes anticoagulant and antiplatelet therapy, thrombolytic therapy, installation of an inferior vena cava cava filter, and surgical removal of the thrombus [5].
Complications of anticoagulant therapy must be kept in mind: major bleeding, heparin-induced thrombocytopenia and warfarin-induced skin necrosis [5]. To reduce the risk of continued thrombus formation, NSAIDs are used [2]. For the purpose of secondary prevention, small doses of heparin are prescribed. Non-drug treatment methods are also prescribed - elastic bandaging, compression hosiery, local hypothermia and exercise therapy [2, 4].
Prevention of thrombosis includes a number of measures used in situations of increased risk of thrombosis.
Primary prevention of atherothrombosis:
- systematic physical activity in the form of walking or morning exercises;
- blood pressure control, maintaining working blood pressure below 140/90 mmHg;
- control of blood sugar levels (less than 6 Mmol/l), early detection and treatment of diabetes mellitus;
- weight loss, body mass index less than 25 kg per m2;
- a diet limited in cholesterol and high-density fat (total cholesterol less than 5 mmol/l), fruits and vegetables;
- smoking cessation [3,7].
Primary prevention of venous thrombosis:
- compression underwear;
- bandaging with elastic bandages;
- drinking plenty of fluids, especially after surgery;
- regular exercise, walking, especially when traveling;
- prohibition of taking alcohol and sleeping pills in large doses;
- prohibition of the use of compressive shoes and clothing [2,5,6].
Sometimes, during periods of particular risk, anticoagulants are prescribed several days before the flight. There is no point in taking aspirin in such cases [5].
Preparing for treatment
In the case of acute thrombosis, surgery to remove blood clots should be performed according to urgent indications in order to save the limb. The urgency of the operation depends on the degree of circulatory failure and the duration of the disease. Preparation for such an intervention is minimal.
- General blood and urine analysis
- Biochemical blood test (urea, creatinine, electrolytes)
- ECG
- Echocardiography - to identify the causes of thrombosis
- Ultrasound of the arteries of the affected limb and possible aneurysms.
- Installation of a urinary catheter
- Installation of an intravenous line catheter
- Cleansing enema
- Shaving surgical access sites
Bibliography
- Consensus position of experts of the Eurasian Association of Therapists on some new mechanisms of the pathogenesis of COVID-19: focus on hemostasis, issues of blood transfusion and the blood gas transport system / G.P. Arutyunov, N.A. Koziolova, E.I. Tarlovskaya, A.G. Arutyunov, N.Yu Grigorieva, etc. // Cardiology. 2020;60(6). DOI: 10.18087/cardio.2020.5.n1132.
- Thrombophlebitis (thrombosis of superficial veins): modern standards of diagnosis and treatment / V.Yu. Bogachev, B.V. Boldin, O.V. Jenina, V.N. Lobanov//Hospital-substituting technologies: Outpatient surgery. 2016.- 3-4 (63-64)- P.16-23.
- Modern problems of thrombosis of arteries and veins / I.N. Bokarev, L.V. Popova // Practical Medicine, 2014. - No. 6 (82) – P13-17.
- Treatment of thrombophlebitis. Current recommendations and clinical practice / P.F. Kravtsov, K.V. Mazaishvili, S.M. Markin, H.M. Kurginyan // Thrombosis, hemostasis and rheology, 2020 No. 2 – P 68-72.
- Venous thrombosis: modern treatment / P.S. Laguta // Atherothrombosis, 2015 - No. 2 - P. 7-16.
- Deep vein thrombosis of the lower extremities / A.K. Lebedev, O.Yu. Kuznetsova // Russian family doctor, 2015.
- National recommendations for the diagnosis and treatment of diseases of the arteries of the lower extremities, Association of Cardiovascular Surgeons of Russia, Russian Society of Angiologists and Vascular Surgeons, Russian Society of Surgeons, Russian Society of Cardiology, Russian Association of Endocrinologists, M, 2021.
- Diagnosis and pharmacotherapy of acute venous thrombosis / N.V. Sturov, G.N. Kobylyanu// Difficult Patient, 2013., No. 12., T. 11. –P.19-22.
- Principles of management of patients with venous thromboembolism during the COVID-19 pandemic // V.Ya. Khryshchanovich // Surgery News, 2021.- t28 No. 3 – P329-338.
What causes blood clots?
Thrombi, in the form of blood clots, form in blood vessels in response to damage to the vascular wall, slowing of blood flow and changes in blood composition. “Thrombosis does not occur out of nowhere; there must be some prerequisites. This is facilitated by the presence of varicose veins in the lower extremities. If it is, you should pay attention to compactions that may appear in the veins,” says phlebologist, surgeon Fedor Shpachenko .
According to the phlebologist, compactions may indicate that blood clots have already formed in the veins. “Often, these blood clots may not occur in the superficial veins that we see, but in deep veins, and it is impossible to visualize them without special research methods,” warns Shpachenko.
Prognosis after treatment method
Arterial thrombosis is a complication of various diseases. This means that removing a blood clot (thrombectomy) is an intervention that eliminates complications. Thus, the prognosis after treatment depends on eliminating the causes of thrombosis. If this is thrombosis associated with narrowing of the arteries, then restoration of the lumen by angioplasty and stenting eliminates the causes of thrombosis and provides a good long-term prognosis. If thrombosis or thromboembolism is associated with diseases of other arteries or the heart, then treatment of these diseases is necessary to prevent repeated episodes of blood clot transfer.
Varicose veins
According to official statistics, every fourth Russian suffers from chronic venous insufficiency of the leg veins. However, the real incidence of venous vessels significantly exceeds the official indicators, because those suffering from this disease, as a rule, turn to a doctor already at those stages when swollen varicose veins not only clearly spoil the beauty of the legs, but also significantly worsen the quality of life.
Article on the topic
In spite of varicose veins. How to help your blood vessels
How to warn. The best way is not to start the disease by contacting a phlebologist at the first symptoms. They are famous. Among the subjective ones (those that the patient feels) are pain, heaviness, and fatigue of the legs. There may also be cramps, itching and burning. Objective (visual) – varicose veins, intradermal reticular varicose veins (spider veins), swelling of the legs.
Symptoms associated with spinal pathology (this is exactly what Dmitry Maryanov ), flat feet, and joint disease are often mistaken for venous disease. Only a phlebologist can correctly assess the patient’s complaints, who will prescribe ultrasound Dopplerography of the vessels of the legs, and, if necessary, prescribe anticoagulants (blood thinners) and elastic compression products (stockings, knee socks, tights). Modern surgical techniques make it possible to avoid removing veins and making skin incisions.
Our information
At different times, the following died from pulmonary embolism: Wilhelm II (Emperor of Germany), Frida Kahlo, Francoise Sagan, Lyudmila Gurchenko, Leonid Gaidai. Other recent victims of a detached blood clot are football player Alexey Arifullin and Zenit sports director Konstantin Sarsania.