Materials and methods
Of the 16,839 patients included in the “Registry of Coronary Angiography Operations” [5] from 1998 to 2013, patients with stenosis of >75% of the lumen of at least one coronary artery, without acute or anamnestic myocardial infarction, without congenital and acquired heart defects: 75 patients with RV dilatation and 1134 without it. The transverse size of the pancreas in the parasternal position was 26 mm or less [6]. For a clearer division of the groups, patients with pancreatic dilatation included patients with a pancreatic size of 30 mm or more; patients with a slight enlargement of the pancreas (>26 and <30 mm) were not included in the study. A clinical, comprehensive echocardiographic examination was performed (one-dimensional, two-dimensional, Doppler echocardiography using Imagepoint NX ultrasound devices, Agilente Technologies, Phillips, USA; Vivid 3, 4, 7, 9 Systems, Vingmed-General Electric - Horten, Norway), determination of lipid composition of blood serum, Holter monitoring, selective coronary angiography according to Judkins (1967) (angiographic complexes Diagnost ARC A, Poly Diagnost C, Integris Allura, Phillips, Holland). Linear echocardiography (EchoCG) parameters were indexed to height; myocardial mass, calculated using the Devereux formula, to the body surface area [7]. Echocardiographic syndromes were diagnosed according to standard criteria: the LV was considered dilated when its end-diastolic diameter index was more than 32 mm/m2 in women and more than 33 mm/m2 in men [2], LV systolic function was reduced when the LV ejection fraction was less than 50%, hemodynamically significant mitral regurgitation (≥II degree) - with an effective area of the regurgitant orifice ≥0.2 cm2, regurgitant volume ≥30 ml [8].
Statistical processing of data was carried out using a package of applied statistical programs (SPSS Inc., version 17.0). Indicators are presented in the form M
±
SD
_
The distribution of variables was determined using the Kolmogorov–Smirnov test. To compare values with their normal distribution, t
; for a non-normal distribution, the nonparametric Mann-Whitney test was used.
When analyzing qualitative indicators, Pearson's χ2 test was used. Differences at p
<0.05 were assessed as statistically significant. Multivariate analysis was performed - binary logistic regression analysis with calculation of odds ratio (OR).
Patient K., 16 years old, complained
of attacks of rapid heartbeat that occurred during moderate physical activity, accompanied by shortness of breath, dizziness, sweating and a single loss of consciousness;
noted an irregular rhythm at rest. From the anamnesis
it is known that the above-described complaints first began to bother me 4-5 years ago (i.e., from the age of 11-12).
For about a year, the patient began to notice a deterioration in his condition, progression of shortness of breath, attacks of rapid heartbeat occurred once every 2 days, and during severe physical exertion a prolonged attack of tachycardia followed by loss of consciousness developed. He was hospitalized, where a paroxysm of sustained ventricular tachycardia with a frequency of 200 beats/min was recorded, which was stopped by intravenous administration of cordarone. Cordarone was prescribed as continuous antiarrhythmic therapy at a dose of 200 mg/day for 3 months. During the therapy, frequent ventricular extrasystole of high grades persisted, but attacks of sustained VT did not recur. From the life history it is known that he suffers from acute respiratory diseases no more than once a year. There was no hereditary history of cardiovascular pathology, and there were no cases of sudden death in close relatives. Objective status
upon admission to the Scientific Center for Cardiovascular Surgery named after.
A.N. Bakulev RAMS. The condition is satisfactory. Height – 171cm, weight – 57kg. Breathing is vesicular, carried out in all parts, there is no wheezing. NPV 15 per minute. Heart sounds are muffled, arrhythmic, heart rate 57 beats/min, blood pressure 110/60 mm Hg. The liver is not enlarged. Data from instrumental examination methods. ECG:
Sinus rhythm, correct. Heart rate – 58 beats/min. The EOS position is normal. PQ – 160 ms, QRS – 90 ms, QT – 400 ms. Intraventricular conduction disturbance, T wave inversion in leads V2-V4, ventricular extrasystole of the bigeminy type with the morphology of left bundle branch block (Fig. 1).
Rice. 1. ECG of patient K. with ARVD: frequent ventricular extrasystole of the bigeminy type, T wave inversion in leads V2-V4
Holter monitoring:
The study was conducted for 23 hours without antiarrhythmic therapy. During the day, sinus rhythm was recorded. Average heart rate 67 beats/min. Min. Heart rate 37 beats/min during sleep. Max. Heart rate 179 beats/min when climbing stairs. Supraventricular ectopic activity is represented by 54 extrasystoles. Ventricular ectopic activity is represented by 6812 PVCs of 3 morphologies, mainly during the daytime. Single – 3644, bigeminy type – 1403, trigeminy type – 1671, paired – 37. 2 episodes of unstable VT of 8 and 9 complexes were registered (Fig. 2). No pauses, changes in ST-T, or QT interval were detected.
Rice. 2. Holter monitoring of patient K.: paroxysm of unsustained VT with a frequency of 200 beats/min
Surface multichannel ECG mapping
on a specialized computer electrocardiological system “Kardiag” (Czech Republic): ECG registration simultaneously from 80 electrodes located regularly throughout the chest, 12 conventional leads and 3 orthogonal Frank leads with subsequent processing in a personal computer. The study was carried out at rest. On the ECG, against the background of sinus rhythm with heart rate = 87 per minute, single PVCs of two morphologies were recorded. When analyzing data from 80 synchronous ECG leads, the sequence of excitation of different zones of the ventricular myocardium, the “normal” or abnormal onset of excitation of the ventricular myocardium can be assessed using isopotential maps (Fig. 3), which correspond to the onset of excitation from the posterobasal part of the interventricular septum (IVS). on the right (Fig. 3-B - extrasystole 1) and from the midbasal part of the anterior wall of the right ventricle (Fig. 3-B - extrasystole 2). Let us note the identified features of the repolarization process during sinus contraction (Fig. 4.). On ECG QTcorr. = 460 ms. A conclusion was made about repolarization disturbances in the projection of the apex, anterior wall of the pancreas and the anterior part of the IVS, as well as signs of myocardial changes in the middle/3 anterior part of the IVS. Fig. 3. Surface ECG mapping of patient K. Isopotential maps constructed for the initial moments of excitation of the ventricular myocardium. A) 16th ms from the beginning of the QRS complex during sinus contraction; B) Extrasystolic complex of the 1st morphology corresponds to the onset of excitation from the posterobasal part of the interventricular septum; C) Extrasystolic complex of the 1st morphology corresponds to the onset of excitation from the midbasal part of the anterior wall of the right ventricle.
The isopotential map is built on a rectangular diagram of the surface of the chest, cut along the right posterior axillary line. Above the map is the moment of the cardiac cycle to which it corresponds; ° – electrode application points; √ – position of the sternal line, · – position of the vertebral line. Potential values are displayed on the map in the form of a color that characterizes the sign and amplitude: blue gamma corresponds to negative values, red to positive; a more intense color reflects a greater potential value. The maximum and minimum potential values (in mev) are indicated = in digital form. The arrows are directed from the initial minimum of the surface potential in the negative zone to the initial maximum in the positive zone on isopotential maps.
Fig. 4. Surface ECG mapping of patient K. A) ECG. Negative T waves in the projection of the anterior part of the interventricular septum; B) Difference map. Deviations of the surface manifestations of repolarization processes from normal, negative values are indicated by a blue gamma.
EchoCG:
The study was conducted against the background of frequent ventricular extrasystole. LA – 3.0 cm. LV: EDS – 2.9 cm, EDS – 4.5 cm, EDS – 32 ml, EDS – 60 ml, EF – 65%. Mitral valve: leaflets are tonic, mobile, multidirectional movement, prolapse of the anterior mitral leaflet, FC 28 mm, no regurgitation. Ascending aorta – 2.5 cm, Aortic valve: intact, FC 21 mm, no regurgitation.
Rice. 5a. EchoCG of patient K. Dilatation of the cavity of the right ventricle. Arrows indicate pronounced trabecularity of the right ventricle, thickening of the moderator cord.
Rice. 5 B. EchoCG of patient K. Dilatation of the cavity of the right ventricle (parasternal position of the short axis of the left ventricle at the level of the mitral valve).
Dilatation of the pancreatic cavity (Fig. 5a, b): ESR – 3.8 cm, EDV – 5.4 cm, EDV – 164 ml, ESV – 113 ml, RV EF – 30% (according to Simpson). Enlargement of the right ventricular outflow tract (RVOT) (Fig. 5c).
Rice. 5th century EchoCG of patient K. Enlargement of the outflow tract of the right ventricle.
The estimated pressure in the pancreas is 30 mm. Hg Pronounced trabecularity of the pancreas and increased echogenicity of the moderator strand are visualized. Decrease in the speed parameters of the free wall of the pancreas and the fibrous ring of the mast cell in the Strain Rate Imaging mode (Fig. 5d).
Rice. 5g. EchoCG of patient K. Assessment of the systolic velocity of movement of the free wall of the pancreas and IVS at the basal and middle levels in the Strain Rate Imaging mode. Decrease in the velocity parameters of the free wall of the pancreas and the fibrous ring of the mast.
Right atrium: 4.5 x 4.2 cm. Tricuspid valve: leaflets are thin, movable. FC – 36 mm, regurgitation 2.5 (+). Pulmonary valve: FC – 25 mm, regurgitation 2 degrees. MZhP movement is correct. No data for UPS was received. Conclusion: Dilation of the right ventricle, decreased contractility of the RV, EF 30%. Tricuspid valve insufficiency 2.5 (+). Pulmonary valve insufficiency grade 2.
X-ray of the chest organs: no inflammatory or focal changes were detected. The pleural sinuses are free. The pulmonary pattern is enhanced. The roots of the lungs are not changed. The heart is positioned normally, the size is not enlarged, the CTI is 49%. The vascular bundle is not changed. The arc of the aircraft bulges moderately. The aorta is without features. The superior vena cava is not dilated. The diaphragm is without any features.
According to laboratory studies
Clinical tests of blood, urine and biochemical analysis revealed no pathological changes.
Based on the clinical picture, laboratory and instrumental research methods, a diagnosis was made: Arrhythmogenic dysplasia of the right ventricle (?). Dilatation of the cavities of the right heart. Tricuspid valve insufficiency grade 2, pulmonary valve insufficiency grade 2. Rhythm disturbances: ventricular extrasystole grade 5 according to Lown. Paroxysmal ventricular tachycardia. Syncope from March 2008. NC II according to NYHA.
Magnetic resonance imaging:
The study was conducted against the background of frequent PVCs. On a series of tomograms, the heart is located in a typical location and is enlarged in size (CTI = 58%). The MR signal from the myocardium is normal. Vessel diameter: SVC 12x17 mm, IVC 15x35 mm, AO ascending at the level of the bifurcation of the pulmonary artery trunk is not expanded to 19 mm, AO descending - 15 mm, aortic arch 19 mm. LA barrel - 14 mm, PLA - 11 mm, LLa - 11 mm. Heart chambers: RA expanded, 60x36 mm, LA 20x30 mm. LV EDV 45mm, LV ESV 34mm, LV ESD 155 ml, LV ESV 68 ml, LVEF 87 ml, EF 56%, minute volume 6.1 l/min, CI 3.1 l/min/m2. EDV of the pancreas 42 mm, ESV of the pancreas 40 mm, EDV of the pancreas 278 ml, ESV of the pancreas 231 ml, PVS 47 ml, EF of the pancreas 17%. The thickness of the anterior wall of the pancreas is 2-3 mm, with an uneven systolic increment of up to 2 mm, hypokinesis of the walls of the pancreas is noted with the presence of small areas of effusion and dyskinesis of up to 2-4 mm (like microaneurysms) (Fig. 6a, b).
Fig.6a. MRI of the heart of patient K. Dyskinesis of the anterior wall of the pancreas (marked with a pointer) (diastole phase)
Fig.6b. MRI of the heart of patient K. Microaneurysms of the anterior wall of the pancreas (marked with a pointer) (systole phase)
Pronounced trabecularity of the pancreas, thickening and compaction of the moderator cord are determined. The RVOT is dilated to 42 mm (Fig. 6c, d).
Fig.6c. MRI of the heart of patient K. Expansion of the outflow tract of the pancreas (longitudinal section)
Fig.6d. MRI of the heart of patient K. Dilation of the outflow tract of the pancreas (cross section)
Fatty infiltration of the pancreatic myocardium (Fig. 6d). The thickness of the IVS is about 7 mm, the posterior wall of the LV is 8 mm, the lateral wall is 6 mm, and the anterior wall is 5 mm. In the pericardium, fluid is detected with a maximum separation of the pericardial leaves up to 4-5 mm. Conclusion: MRI signs of cardiomegaly, dilatation of the cavities of the right heart, decreased contractility of the RV (EF - 17%); hypokinesis with areas of uneven thinning of the pancreatic walls; fatty infiltration of the pancreatic myocardium.
Fig.6d. MRI of the heart of patient K. Area of fat (marked with arrows)
Contrast angiography of the right heart:
the heart is right-formed, left-sided. The vena cava is located to the right of the spine and drains into the RA. Dilatation of the pancreatic cavity (Fig. 7a), the outflow tract of the pancreas is significantly expanded (Fig. 7b), contractile function is reduced. The pulmonary artery arises from the pancreas. The branches are not narrowed or hypoplastic. The pulmonary veins drain into the LA. There is no communication between Ao and LA. There is no data on the presence of messages on the MZhP and MPP. Pressure in the cavities: RV(syst)=30 mmHg, RV(diast_v)=2 mmHg, LAST(syst)=30 mmHg, LAST(diast)=16 mm. Hg, LAST(avg)=20.67 mmHg. Conclusion: Dilatation of the pancreatic cavity. Decreased contractile function of the pancreas. There is no evidence for the presence of congenital heart defects.
Rice. 7a. Angiocoronary angiography of patient K. Dilatation of the pancreas
Rice. 7b. Angiocoronary angiography of patient K. Expansion of the excretory tract.
Electrophysiological study:
Sinus rhythm is initially recorded. Antegrade Wenckebach point = 600 ms. AERP AVU = 470 ms, ERP LA = 210 ms, ERP PP = 260 ms, Retrograde VA dissociation. RV ERP = 280 ms. With programmed stimulation of the RV S1=300, S2=280, S3=340, a paroxysmal form of VT is induced from the anterior wall of the RV outflow tract with DC = 300 ms, self-limiting after 3 sec.
As a result of a detailed examination of the patient, the following diagnostic criteria for ARVD were identified: pronounced dilatation and decrease in systolic function of the RV in the absence of changes in the LV; localized pancreatic aneurysms; T wave inversion in the corresponding leads; unsustained VT with left bundle branch block morphology (documented with Holter monitoring)
Since this pathology is characterized by progressive replacement (initially focal, then diffuse) of the myocardium of the right ventricle with fatty and connective tissue and is manifested by threatening ventricular arrhythmias, the patient underwent radiofrequency ablation of foci of ectopic ventricular arrhythmias from the right ventricle and antiarrhythmic therapy was selected (cordarone 200 mg/day ), however, during 24-hour Holter ECG monitoring, episodes of ventricular tachycardia continued to be recorded.
For the purpose of secondary prevention of SCD, the patient was implanted with a Medtronic GEM III VR 7231 Cx automatic cardioverter defibrillator with a primary endocardial system.
The postoperative period proceeded without complications. The patient noted improved health and the absence of attacks of sustained ventricular tachycardia. Positive dynamics were also confirmed according to ECG and Holter monitoring (ventricular ectopic activity is represented by PVCs of 2 morphologies, of which: single - 1227, bi- and trigeminic - 95, paired - 46, triplets - 6). During the hospital stay, no defibrillator discharges were recorded.
How typical is our observation for ARVD? What are the current trends in the treatment of this disease? And finally, have our views on its pathogenesis, principles of diagnosis, treatment and possible predictors of sudden cardiac death undergone evolution?
Read on the pages of the magazine “Creative Cardiology”.
results
The majority in both groups were men, but in contrast to the group of patients with normal pancreatic size, men were more common in the group with pancreatic dilatation. Patients in this group showed a tendency toward older age (Table 1).
Table 1. Comparative characteristics of clinical, functional and laboratory parameters of patients with coronary artery disease without myocardial infarction, depending on the presence of pancreatic dilatation Note. Here and in the table. 2: data are presented as mean ± standard deviation or number of patients (in%). SBP—systolic blood pressure; DBP—diastolic blood pressure; FC - functional class; NYHA - New York Heart Association; nd - statistically insignificant differences.
The groups did not differ in the frequency of smoking, alcohol consumption, levels of SBP and DBP, the frequency of detection of arterial hypertension, diabetes mellitus, hypothyroidism and heredity burdened with ischemic heart disease. The average BMI in both groups corresponded to obesity, but in patients with a dilated pancreas it was statistically significantly higher. Patients with RV dilatation more often demonstrated a higher (III) FC of CHF according to the New York Heart Association (NYHA) classification, as well as NRPS with less frequently detected severe (III-IV) FC of exertional angina. There were no intergroup differences in basic laboratory parameters and coronary angiography data. When analyzing EchoCG parameters in patients with dilated RV, higher indices of the linear dimensions of the heart and LV myocardial mass were revealed with no statistically significantly different index of the thickness of the interventricular septum and a tendency towards a lower index of thickness of the posterior wall of the LV. The groups did not differ in the LV asynergia index; the LV ejection fraction was lower in the group with an enlarged RV. Dilatation of the left ventricle, a decrease in its contractility, as well as significant mitral regurgitation and signs of atherosclerotic lesions of the aorta were more often detected in patients with dilatation of the right ventricle (Table 2).
Table 2. Comparative characteristics of echocardio-, electrocardio- and angiographic parameters of patients with coronary artery disease without myocardial infarction, depending on the presence of RV dilatation Note. * — degree of coronary lumen stenosis >75%.
According to the results of multivariate analysis, an independent relationship with RV dilatation was demonstrated by a decrease in myocardial contractility, male gender, NRPS, significant mitral regurgitation, an increase in the FC of CHF and BMI, as well as a decrease in the FC of angina pectoris (Table 3).
Table 3. Parameters independently associated with pancreatic dilatation in patients with coronary artery disease without myocardial infarction
Differential diagnosis for dilatation of the right chambers of the heart.
One of the most difficult differential diagnostic situations in echocardiography is dilatation of the right heart chambers in a patient. The percentage of patients with dilatation of the right chambers of the heart of unknown etiology is quite high. In some cases, an echocardiographer can determine the cause of this dilatation, as, for example, with a large atrial septal defect, or suggest to the clinician the tactics and direction for further examination of the patient, excluding a number of pathologies.
It is necessary to distinguish between dilatation of all right chambers of the heart, i.e. right atrium, right ventricle and pulmonary artery, and isolated dilatation of the right atrium only, right ventricle only and pulmonary artery only.
Dilation of the right heart can occur in any age category and in some cases be an echocardiographic finding. To avoid mistakes during the study, it is necessary to clearly understand the differential diagnostic range in which dilatation of the right parts of the heart occurs.
Causes of dilatation of the right atrium, right ventricle and pulmonary artery.
- Pathology of the left chambers of the heart with the formation of pulmonary hypertension
- Pulmonary embolism (PE)
- Chronic cor pulmonale (variant with dilatation of the right chambers of the heart)
- Atrial septal defect (ASD)
- Ventricular septal defect (VSD) (muscular or membranous)
- Patent ductus arteriosus (PDA) (ductus ductus arteriosus)
- Pulmonary valve stenosis or its combination with PDA
- Damage to the right heart valves (tricuspid valve and pulmonary valve) in infective endocarditis
- Rupture of the interventricular septum due to myocardial infarction with the formation of an acquired defect
- Infarction with transition to the right ventricle
- Portal hypertension
- Long-term pacing
- Ebstein's anomaly
- Accessory superior vena cava
- Eisenmenger complex
- Primary pulmonary hypertension
- Abnormal pulmonary vein drainage
- Tetralogy of Fallot
- Congenital absence of pericardium
- Abnormal drainage of hepatic veins
- Operated congenital heart defects
- Tumors of the right chambers of the heart
- Ull's anomaly, or arrhythmogenic dysplasia of the right ventricular wall
- Condition after pericardiectomy
- Carcinoid heart disease
- Left ventricular-right atrial fistula after mitral and aortic valve replacement due to infective endocarditis or oblique VSD.
Causes of isolated dilatation of the right atrium.
- Tricuspid valve stenosis
- Infectious endocarditis with damage to the leaflets and chords of the tricuspid valve and pronounced “acutely occurring” tricuspid regurgitation against this background.
Causes of isolated pulmonary artery dilatation.
- Pulmonary valve stenosis (poststenotic dilatation)
- Some forms of PDA
- Combination of pulmonary valve stenosis and PDA
- Double origin of vessels
- Coronary fistula (arteriovenous) – shunting of blood from the left coronary artery into the trunk of the pulmonary artery
Discussion
It is known that ventricular dilatation after MI is more pronounced in patients with a larger area of LV myocardial damage [9]. Therefore, in patients with coronary artery disease, one can expect to find a connection between RV dilatation and multiple coronary stenoses or with a larger size of LV asynergia. RV MI often develops as a result of damage to the proximal part of the non-dominant right coronary artery [10, 11], so RV dilatation in our patients could be associated with damage to this localization in the left type of coronary circulation. However, there were no intergroup differences in the type of coronary circulation, the prevalence or localization of coronary lesions, and the LV asynergia index. The negative relationship between right ventricular dilatation and the FC of angina pectoris necessitates further study.
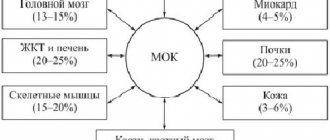
An increase in the size of the pancreas in patients with coronary artery disease can serve as a sign of increased pulmonary vascular resistance and load on the pancreas, determined by the condition of the left chambers of the heart [2]. Left ventricular dysfunction, causing postcapillary pulmonary hypertension, is the most common cause of right ventricular dilatation [8]. In the present study, LV systolic dysfunction was observed in 25% of patients with dilated RV, and it was the strongest predictor of RV enlargement in multivariate analysis.
The risk of RV dilatation also increased with NRPS, significant mitral regurgitation and with an increase in the FC of CHF - the same as in patients with MI [3].
Among the factors associated with RV dilatation and not related to the LV condition were male gender and an increase in BMI (the same connections were found in patients with MI [3]). The fact is that obese patients often develop obstructive sleep apnea syndrome due to hypoventilation and hypercapnia, accompanied by the development of pulmonary hypertension and, as a consequence, pancreatic dilatation [12]. Perhaps it is this factor that explains the connection between pancreatic dilatation and obesity.
A limitation of this study was that the only parameter of the pancreas was analyzed - its transverse size in the parasternal position. This is explained by the fact that the collection of data for the Register began in 1998, when not all patients had other indicators characterizing the structure and function of the pancreas. The point of our study is to use a large amount of material to study the general patterns of the course of IHD, in particular the factors associated with pancreatic dilatation in a specific population. Inclusion in the analysis only of patients with a complete set of pancreatic characteristics would significantly reduce the sample and would not allow obtaining the most reliable result. Thus, limitations of the study stem from its retrospective nature. Since P.Zh. is a chamber that is extremely sensitive to changes in afterload, and the assessment of the size of the pancreas is an integral part of the characteristics of its function [13], we consider it possible to judge the state of the pancreas by assessing its linear size alone.