Modern methods of myocardial revascularization
CABG surgery under conditions of artificial circulation and cardioplegia remains today the “gold standard” for the treatment of coronary artery disease. However, there are a number of modern techniques that are currently used for myocardial revascularization.
1. Multiple myocardial revascularization using both IAVs
2. Minimally invasive myocardial revascularization
2.1. Operations without IR via mini access (MIDCAB)
2.2. Operations without IR through sternotomy (OPCAB)
2.3. Operations using the port access method
2.4. Operations with video endoscopic support
2.5. Totally endoscopic myocardial revascularization (TECAB)
3. Transmyocardial laser revascularization (TMLR)
4. Therapeutic angiogenesis and cell therapy
Minimally invasive myocardial revascularization (MIRM) is a coronary artery bypass surgery on a beating heart without cardiopulmonary bypass (CPB).
The operation has become widespread since the mid-80s in Russia, the USA and Western European countries. Most surgeons operating on the beating heart (without IR) perform myocardial revascularization through sternotomy (OPCAB - Off-pump coronary artery bypass).
To work on a beating heart, special devices have been created that make it possible to stabilize a limited area of the myocardium in the area where the anastomosis with the coronary artery is performed. Currently, two main types of stabilizer are used, one of which stabilizes the myocardium by local pressure, the other by vacuum. The most widely used system is the “Octopus” system, based on the vacuum principle.
Special anesthetic techniques have been developed to successfully perform such operations. Modern advances in surgery and anesthesiology make it possible to perform bypass surgery of up to 6 coronary arteries without IR.
The advantages of coronary bypass surgery without IR are:
1. no traumatic damage to blood cells,
2. shorter duration of the operation,
3. faster postoperative rehabilitation,
4. absence of complications associated with cardiopulmonary bypass.
Indications for MIRM are the same as for myocardial revascularization with CPB. At the same time, there are contraindications that do not allow operations without IR: for example, post-infarction aneurysm of the left ventricle, congenital or acquired heart disease requiring surgical correction.
Transmyocardial laser revascularization (TMLR)
TMLR is intended for patients with diffuse coronary artery disease who cannot undergo direct myocardial revascularization. During this operation, channels are formed in the thickness of the cardiac muscle of the left ventricle using laser radiation, opening into the cavity of the heart. This effect on the myocardium stimulates the formation of a new vascular network, due to which myocardial perfusion is compensated and ischemic phenomena are eliminated, despite the existing narrowing of the coronary arteries.
The positive clinical effect is also explained by the mechanism of sympathetic denervation of the heart, since laser exposure leads to the destruction of myocardial axons and the elimination of the pain impulse. Recently, the positive mechanism of action of TMLR has been associated with stimulation of angiogenesis. In our country, the pioneer of the clinical use of TMLR is Academician of the Russian Academy of Medical Sciences L.A. Bockeria. At the Scientific Center for Sports Culture named after. A.N.Bakuleva TMLR is used in two versions: isolated and in combination with CABG (with diffuse damage to one of the coronary vessels).
Therapeutic angiogenesis and cell therapy
Vasculoendothelial angiogenic growth factor (VEGF) and stem cell marker CD 133+
Minimally invasive myocardial revascularization (coronary artery bypass surgery on a beating heart without artificial circulation) with the introduction of angiogenic factors
In reality, we are talking about surgical procedures. The essence of this newest method of treating coronary artery disease lies in the genetic effect on the endothelium, leading to its proliferation and the formation of new vessels. The effect is produced by transferring genetic information into the cell using carriers, which are some viruses and plasmid complexes. In the cell, genetic information is read and protein synthesis occurs, the so-called angiogenic factors, the most important of which are vascular endothelial growth factor (VEGF) and fibroblast growth factor (FGF). In 1998, they were first used in clinical practice to stimulate angiogenesis in patients with diffuse lesions of the coronary arteries. Angiogenic factors are injected directly into the myocardium using a syringe during CABG or TMLR surgery. There are also catheter methods for introducing these factors (endocardial and intracoronary).
Another new approach to the treatment of coronary disease is the use of cellular technologies, that is, the introduction of stem cells into the myocardium, or more precisely, mononuclear cells - the precursors of endothelial cells. It is believed that this may lead to the formation of new vessels, which will compensate for the deficiency of coronary blood flow in diffuse damage to the coronary arteries. The results of using these methods require further study.
Alshibaya M.M. "Clinical cardiology: diagnosis and treatment", 2011. edited by Bockeria L.A., Golukhova E.Z.
EECP treatment protocol
All potential patients to receive EECP sessions had detailed medical documentation, in addition, they underwent a thorough physical examination, during which attention was paid to symptoms of the disease, previous revascularization procedures, and documentation confirming CAD (Table 1). Special precautions were taken to identify whether patients had any contraindications to this procedure (Table 2).
The principle of operation of EECP is to sequentially fill and deflate air from cuffs wrapped around the patient's calves and thighs. The inflation and deflation of air in the cuffs is synchronized with the cardiac cycle, and is controlled by ECG signals, which are processed by a microprocessor (Fig. 1). As a result of compression of the muscles of the lower extremities, diastolic pressure in the aorta increases, which leads to an increase in perfusion pressure in the coronary arteries. Sessions usually last 1 hour per day, the total course consists of 35 hours over 7 weeks.
Table 1. Indications for EECP treatment
| Symptoms of myocardial ischemia (corresponding to FC III-IV), despite optimal drug therapy. The patient is not a candidate for surgical or percutaneous revascularization. IHD is confirmed by the presence of: stenosis >70% in at least 1 of the main epicardial coronary arteries and/or bypass, or scintigraphic or echocardiographic evidence of myocardial infarction and/or myocardial ischemia, or a history of myocardial infarction. |
Table 2. Relative contraindications to EECP
| Persistent, persistent ischemia. Decompensated congestive heart failure. Severe pathology of the valve apparatus. Uncontrolled arterial hypertension (> 180/110 mmHg). Malignant arrhythmias. Severe pathology of peripheral vessels. A history of phlebitis, deep venous thrombosis, severe varicose veins, or trophic ulcer. Bleeding diathesis, including continued use of warfarin with INR >2.0. Increased risk of bleeding (within 7 days after angiography or other invasive procedure). Pregnant or fertile women who do not use a reliable method of contraception in order to avoid pregnancy. |
How is transmyocardial laser revascularization (TMLR) performed in Germany?
You usually need to go to the hospital the day before surgery. The operation is performed under anesthesia. In other words, you will be asleep during the procedure.
The heart surgeon will make an incision in the left side of the chest to reach the left ventricle of the heart. The surgeon will then use a special laser to create small channels in the heart muscle. The canals may bleed for a few seconds, but the bleeding will stop when the surgeon applies gentle finger pressure to the canals. The tops of the channels are closed by a blood clot, but inside the heart the channels remain open.
The duration of the operation is about 2 hours.
In some cases, cardiac bypass and TMLR may be performed simultaneously.
Discussion
The presented case is an impressive example of the capabilities of EECP used to reduce the symptoms of myocardial ischemia. At the beginning of therapy, the patient was bedridden due to severe angina. After 7 weeks of EECP treatment, she was able to exercise daily without angina and had no evidence of myocardial ischemia on repeat myocardial scintigraphy. This positive clinical result was maintained for 9 months after treatment.
There is growing evidence of the effectiveness of EECP used for angina for 2 decades. This procedure, first proposed by Kantrowitz and Kantrowitz, is non-invasive and non-traumatic, it increases diastolic blood pressure and perfusion pressure in the coronary arteries, and also helps unload the left ventricle, similar to intra-aortic counterpulsation. The first hydraulic counterpulsation devices were cumbersome and have been modified over several years and now include computerized, ECG-controlled pneumatic compression cuffs that are wrapped around the lower extremities, which improves diastolic augmentation and reproducibility. The use of new EECP devices has demonstrated long-lasting reductions in symptoms of myocardial ischemia and improved quality of life in a heterogeneous group of patients with coronary artery disease.
Recovery period and life after TMLR
After the operation you will need to stay in the clinic for 4-7 days. At first, it will be necessary to limit physical activity. Your doctor may recommend a special exercise program for cardiac rehabilitation.
If you have an office job, you will be able to return to it in 4-6 weeks. Those with more physically demanding jobs may have to wait longer.
In most cases, symptoms of coronary artery disease and angina improve after TMLR, but this may take 3 months or more.
Over time, patients find that they can perform activities that once caused them pain. It will also be possible to refuse some cardiac medications.
Heart surgeries in Germany
EECP in the treatment of angina pectoris
The results of several studies have been published that report experience with the use of EECP in patients with angina refractory to drug therapy. These patients were not suitable candidates for percutaneous or surgical revascularization. Studies have shown a significant reduction in the Canadian Society of Cardiology classification of angina; the number of nitroglycerin tablets used daily; increasing tolerance to physical activity; and a decrease in myocardial ischemia according to objective data (Table 4). The disadvantages of these studies are that they involved a small number of patients and there was no control to rule out the placebo effect. A recent multicenter, randomized, placebo-controlled EECP trial randomized 139 patients with angina and documented CAD to active versus hemodynamically inactive counterpulsation. The active counterpulsation group showed a significant increase in the time to the development of ST segment depression during exercise, as well as its duration. The number of angina attacks also decreased significantly in the main group (Table 5). No serious complications were observed, and the impact on quality of life was maintained for 1 year. Radionuclide perfusion scintigraphy showed a decrease or disappearance of perfusion defects after a course of EECP. Also, EECP could increase perfusion from the initial level, which was proven by positron emission tomography data.
Table 4. Results of the first non-randomized EECP studies
| Author | Number of patients | Number of treatment sessions (hour) | Reduction in angina symptoms (%) | Perfusion improvement (%) |
| Zeng et al., 1983 | 200 | 12 | 97 | N.A. |
| Lawson et al., 1992, 1995 | 18 | 36 | 100 | 78 |
| Karim et al., 1995 | 38 | 36 | 86 | 78 |
| EECP=enhanced external counterpulsation; NA=not available. | ||||
Table 5. Change in exercise tolerance in MUST-EECP*
| Control group | EECP Group | ||||
| Options | № | Average (SE) changes (sec) | № | Average (SE) changes (sec) | R |
| Duration of load | 58 | 26(12) | 57 | 42(11) | .30 |
| Time to development of ST segment depression | 56 | — 4 (12) | 56 | 37 (11) | .01 |
| *MUST-EECP= Multicenter EECP Study | |||||
What is myocardial revascularization: description and methods
Coronary revascularization (“re” – restore, repeat; “vas” – vessel) is a method of restoring blood flow in the affected area of the myocardium, in which the patency of coronary vessels or bypass options for blood supply is restored.
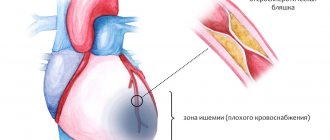
Most often, the development of myocardial infarction is associated with blockage of the lumen of the coronary artery by atherosclerotic plaque, which forms over several years in people with impaired fat metabolism. Damage to the vessel wall with the accumulation of free and bound lipids, activation of inflammation and the launch of the blood coagulation system contribute to the disruption of arterial patency.
The appearance of characteristic symptoms (pain behind the sternum, shortness of breath) develops when the lumen of the vessel decreases by 90%.
In modern cardiological practice, two main options for restoring blood flow are used:
- pharmacological using drugs for thrombolysis (“Metalise”, “Actelise”);
- surgical revascularization of the myocardium.
Carrying out pharmacological thrombolysis (splitting of a blood clot) has significant limitations in its use: the need to perform it in the first two hours after recording abnormalities on the electrocardiogram and the presence of such contraindications:
- use of anticoagulants;
- bleeding in the last six months;
- major surgical interventions in the previous six months;
- previous hemorrhagic stroke;
- pregnancy;
- chronic kidney disease, liver disease and others.
Surgical methods of revascularization do not imply a narrow therapeutic window (they are carried out both urgently and routinely), and are allowed while taking anticoagulants.
In addition, the method allows for local impact on the lesion without the development of systemic undesirable consequences. It is possible to carry out repeated intervention after a short period, which is prohibited after thrombolysis. Therefore, surgical methods of revascularization are considered the method of choice for impaired blood flow in the coronary vessels