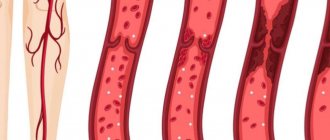
The vessels of the venous system are often exposed to various inflammatory processes, the direct consequence of which is thrombophlebitis. When inflammation occurs, a blood clot forms on the wall of the vein - a thrombus, which partially or completely blocks the blood flow in the vessel. Both superficial and deep veins can suffer from this pathology, and the signs of thrombophlebitis in both cases can differ in intensity. Acute and chronic forms of the disease are known, and the subacute form is also classified. In some cases, purulent formation and even gangrene develop. The disease much more often affects the lower extremities, although thrombophlebitis of the upper extremities is also not a rare occurrence.
Thrombophlebitis: symptoms and signs
External signs of thrombophlebitis depend on the form of the disease. In addition, it is often associated with other pathologies. It is often preceded by varicose veins, so patients with this pathology need to consult a qualified doctor as soon as possible, who will develop an effective program to prevent the formation of blood clots.
In any case, the appearance of thrombophlebitis does not go unnoticed, since the walls of the vein undergo significant changes, blood pressure increases due to impaired blood flow, and the inflammatory process causes an increase in body temperature. Pain occurs in the area of the affected vessel (especially sharp in the acute form). Regional lymph nodes may enlarge.
A blood clot that breaks away under the pressure of the bloodstream clogs smaller vessels. This can also happen in the brain, lungs, and heart. The patient has symptoms of myocardial infarction, stroke, mesenteric thrombosis of intestinal vessels, and pulmonary embolism. The most common signs of a broken blood clot are:
- sharp pain;
- cold extremities;
- blue skin;
- lack of air.
It is necessary to urgently consult a doctor, as a blocked vessel can cause death .
Thrombophlebitis of the superficial veins of the lower extremities
It is this form of thrombophlebitis of the legs that is considered the most common, and it is most often preceded by varicose veins. A blood clot is indicated by a seal on the vessel, which, as a result of varicose veins, has taken on a convex shape and is clearly visible under the skin. As the blood clot expands and lengthens, the vein becomes like a subcutaneous cord.
The tissue around the clot swells and the skin turns red. The process is accompanied by acute pain, which increases when you press on the area where the blood clot forms. Typically, thrombophlebitis of the veins of the lower extremities does not prevent the patient from moving the leg, but movement can be very painful. Body temperature does not exceed 37.5 degrees. Sometimes inflammation can spread to neighboring tissues - periphlebitis occurs.
The acute form mainly occurs due to infectious exposure. A blood clot forms at the site of infection, provoking, in turn, inflammation of the vessel wall. Acute superficial thrombophlebitis of the lower extremities causes the temperature to rise to 38o, and then it normalizes. Lumps are felt under the skin, the size of which depends on the diameter of the vein in which the blood clot has formed.
The chronic form is characterized by prolonged congestion in the lower limb, increased swelling and pain after exertion on the legs. In addition, pus may form in the affected tissues, and abscesses may form on the skin.
How does the venous system of the legs work?
Relatively speaking, the veins in the legs form two levels - superficial and deep.
Superficial veins provide only about 10% of venous blood flow, but they perform a very important function. In addition to collecting blood and moving it to the heart, these veins can act as a kind of reservoir, which, if necessary, can receive blood from the deep veins. Thus, the load on the veins is regulated by internal mechanisms. Veins from the deep and superficial layers are connected to each other by so-called perforating veins. Due to this, balance is maintained in the venous system.
Superficial veins are at risk of excessive stretching: if a person moves little, eats poorly, is overweight or simply has a hereditary predisposition, then the blood flow slows down and the vein wall stretches. Special valves that block the reverse flow of blood do not close tightly, and we are talking about varicose veins. Deep veins are located in the thickness of the tissues and ensure that the main volume of blood moves to the heart. The surrounding muscles maintain the tone of these vessels and facilitate blood flow, so the deep veins are not susceptible to varicose veins.
Thrombophlebitis of deep veins
The signs of this type of pathology largely depend on the location of the affected vessel. Among the acute forms, thrombophlebitis of the deep veins of the leg stands out in its frequency. It is characterized by the appearance of sudden pain, bursting the muscles of the lower leg. The pain may subside a little if you put your leg in a horizontal position. However, an almost painless manifestation is possible in the presence of other symptoms of thrombophlebitis: swelling, bluish color of the skin and its tension. When pressing on the skin, a dimple remains, which gradually smoothes out.
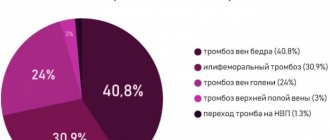
On the other hand, the disease can pass without any obvious signs at all. With thrombophlebitis of the femoral vein and deep veins of the pelvis, the presence of a blood clot may be indicated by slight swelling on the inner surface of the thigh and mild pain in the groin area. Thrombophlebitis of the iliofemoral segment of the main vein also has subtle signs. It manifests itself as mild pain in the lower back, near the sacrum, and in the lower abdomen. And in some cases, the only symptom may be thromboembolism - when the blood clot has already broken off.
Thrombophlebitis of the deep veins of the lower extremities also manifests itself as a general malaise. Body temperature can rise to 40o. And if the common femoral vein is affected, the patient may have a fever and there are signs of intoxication of the body.
The acute form in almost all cases is characterized by the appearance of acute pain at the site of blood flow disturbance. The swelling may be loose at first and then gradually harden. In the affected area, veins clearly appear on the surface of the skin, and the temperature rises significantly. When making a diagnosis, the doctor places a sphygmomanometer cuff near the affected area and monitors the increase in pressure that causes acute pain. In acute cases, a pressure of 45-60 mmHg is sufficient.
The chronic form by a long course, and the symptoms of thrombophlebitis can appear from time to time for 2-3 years without significant deterioration. The thrombus may be partially destroyed, the patency of the vessel temporarily improves, and the vein wall is overgrown with connective tissue. But since the outflow of blood from the lower extremities is impaired, the symptoms return:
- swelling becomes stable;
- a feeling of fullness and heaviness in the leg haunts when walking;
- severe muscle cramps occur at night;
- dense formations appear under the skin;
- the skin itself acquires ring-shaped pigmentation.
Since such symptoms of thrombophlebitis of the lower extremities are extremely likely to cause dermatitis, eczema, and trophic ulcers, it is necessary to start treatment as early as possible.
Vein thrombosis (phlebothrombosis) - symptoms and treatment
Treatment tactics for superficial and deep vein thrombosis differ from each other.
Superficial thrombophlebitis is most often treated on an outpatient basis under the supervision of a surgeon or cardiovascular surgeon. Antiplatelet therapy that prevents thrombus formation (acetylsalicylic acid preparations, etc.) and non-steroidal anti-inflammatory drugs (for severe pain) are usually prescribed.
Local treatment is of particular importance. The most popular are heparin-based ointments and gels; semi-alcohol compresses are also used. Heparin has a local anticoagulant anti-inflammatory effect and also improves microcirculation. The mechanism of action of semi-alcohol compresses is based on the decongestant effect of alcohol and its antiseptic properties. Compression hosiery plays an important role in the favorable outcome of treatment of superficial thrombosis of the veins of the lower extremities. Thanks to moderate elastic compression, a frame is created around the limb, which stabilizes the venous walls, preventing increased stretching. In addition, the risk of a blood clot breaking off and migrating to the heart and lungs is reduced, since it becomes fixed to the vessel wall.
If it is impossible to provide outpatient medical observation, the patient should be hospitalized in a hospital [15].
Deep vein thrombosis requires more serious approaches to treatment. Anticoagulant therapy is mandatory, which significantly reduces the risk of pulmonary embolism. It must be remembered that timely and adequate prescription of anticoagulants can minimize the consequences of thrombosis and significantly reduce the severity of postthrombophlebitis syndrome [1][2].
Modern anticoagulants are divided into two groups: direct and indirect. Direct drugs include heparin and its low molecular weight analogues. Direct anticoagulants are prescribed in the acute period of deep vein thrombosis of the lower extremities. The duration of use is about two weeks, depending on the specific clinical situation and the general condition of the patient.
Indirect anticoagulants act indirectly and are used for a long period of time (4 months or more). The mechanism of action of indirect anticoagulants is to block the synthesis of blood coagulation factors in the liver, as well as a number of biochemical reactions. This group of drugs is completely safe. A number of patients with cardiovascular pathology take them for life. However, taking some drugs is necessarily accompanied by laboratory monitoring of blood coagulation parameters (international normalized ratio - INR, prothrombin index - PTI, fibrinogen, etc.).
Modern medicine and pharmacology have in their arsenal such drugs that do not require laboratory control. Their dosage is calculated per kilogram of the patient’s body weight. Important! Anticoagulants are taken under the mandatory supervision of the attending physician.
The main risk of anticoagulant therapy is gastrointestinal bleeding. Patients should monitor the condition of the gastrointestinal tract: carry out timely drug therapy for gastric ulcers and chronic gastritis, and also, if necessary, undergo fibrogastroscopy (only as prescribed by a doctor).
If signs of gastrointestinal bleeding appear (black stools, vomiting “coffee grounds”), you should immediately seek medical help in a surgical hospital.
Despite the fact that a number of deep vein thromboses, depending on the location of the clots, can be treated on an outpatient basis, groups of patients who have:
- signs of pulmonary embolism (shortness of breath, chest pain, cough, sometimes with hemoptysis, drop in blood pressure, rapid pulse, cyanosis of the skin);
- iliofemoral (iliofemoral) and more extensive thrombosis;
- thrombosis of the superior and inferior vena cava;
- primary localization of thrombophlebitis on the thigh with damage to the great saphenous vein;
- primary localization of thrombophlebitis in the upper third of the leg with damage to the small saphenous vein;
- ascending thrombophlebitis - superficial thrombophlebitis, spreading to the above segments, despite adequate therapy;
- a floating thrombus in the superficial or deep vein system, identified by duplex ultrasound scanning at the prehospital stage.
Surgical treatment for venous thrombosis depends on the location of the clot.
In case of thrombophlebitis of the superficial saphenous veins above the knee joint, it is necessary to raise the question of performing a Troyanov operation - ligation of the great saphenous vein to prevent the spread of a blood clot into the deep vein system.
For deep vein thrombosis, surgical approaches may be as follows:
- deep vein thrombectomy - surgical removal of a blood clot;
- thrombolysis - the introduction of special drugs into the vascular bed that dissolve blood clots;
- placement of vena cava filters (clot traps);
- a combination of these methods.
Rehabilitation of patients who have suffered venous thrombosis is always complex. It is aimed at preventing relapse of the disease and includes:
- preventing the action of provoking factors;
- active motor mode;
- body weight control;
- taking pharmaceutical drugs;
- wearing elastic knitwear;
- pneumomassage of the limbs;
- physiotherapeutic and sanatorium-resort treatment.
How to treat thrombophlebitis?
Depending on the form and severity, thrombophlebitis is treated at home or on an outpatient basis. Treatment can be carried out at home for damage to the superficial vessels of the hand, forearm, foot, and leg. In this case, the patient’s physical activity is limited, special ointments are applied locally to improve blood circulation, cold, and elastic bandages. Inside – anti-inflammatory drugs, antibiotics. Physiotherapeutic procedures are prescribed - magnetic therapy, pulsed currents, etc. Particular attention is paid to prevention.
Treatment for symptoms of thrombophlebitis of the lower extremities, characterized by damage to the deep veins , is carried out exclusively in a hospital, as there is a threat of embolism. Surgery may be necessary to remove a large blood clot, suppuration, gangrene, etc.
Symptoms
They do not make themselves felt immediately, but as the blood clot grows. Often, the presence of the disease is discovered only if a blood clot breaks off and enters the lungs. The most striking symptoms include:
- bursting pain in the legs, which appears when walking and disappears when the lower extremities are elevated;
- cyanosis of the skin;
- frequent swelling in the leg area (thigh, foot, calf or calf muscle);
- sore calves;
- increased temperature of the calf muscle (heat flush);
- brown skin tone (late stage).
Compression treatment
This method is used most often in the chronic course of the disease, after inflammation has subsided, and for prevention. In addition, it is effective only for thrombophlebitis of the superficial veins . It is not prescribed for deep vein pathology.
Medical knitwear is used: tights, stockings, knee socks of different lengths and with compression class 2 or 3. The use of special elastic bandages is effective. Bandaging is carried out at the beginning of the day, and the bandages are removed at night. This helps maintain limb tissue in good shape. Knitwear and bandages prevent the expansion of veins and the separation of a blood clot. After a few days it may completely resolve.
Also, in chronic and subacute forms, warm compresses are prescribed. They improve blood circulation and elasticity of tissues and blood vessels.
Physiotherapy
Physiotherapeutic treatment of thrombophlebitis of the lower extremities is effective for the chronic form of superficial thrombophlebitis and includes a number of measures:
- infrared rays;
- Sollux;
- magnetic therapy;
- electrophoresis;
- ultraviolet irradiation;
- pulse currents.
These methods are not used in the presence of trophic formations and during periods of exacerbation. A trip to a balneonological resort is possible only after consultation with a doctor and requires a special appointment.
Separately, it is worth noting hirudinotherapia - treatment with leeches. This method is applicable in the acute form and if the patient experiences intolerance to anticoagulant drugs (reducing blood viscosity). In this case, the role of these drugs is played by hirudin, contained in the glands of leeches and entering the patient’s blood. However, their use is strictly individual, has serious contraindications and requires mandatory consultation with the attending physician.
Drug treatment
Prescription of medications for thrombophlebitis should be comprehensive:
- anticoagulants reduce blood clotting;
- non-steroidal anti-inflammatory drugs and antibiotics act on the very cause of blood clots – infection;
- for severe pain, painkillers are used;
- special external ointments help dissolve blood clots; anti-inflammatory gels are also applicable;
- Enzyme therapy is carried out to dissolve the blood clot and eliminate swelling;
- the action of venotonics is aimed at strengthening the walls of blood vessels and increasing their elasticity;
- Angioprotectors may also be additionally prescribed.
For the treatment of thrombophlebitis, the use of rutin is important. It increases the tone of large vessels, strengthens their walls, reduces swelling and inflammation. Heparin contained in ointments is no less important. Their use allows you to avoid taking medications internally.
In the absence of severe complications, the effect of drug therapy is felt within a few days.
Surgical intervention
The main indication for surgery is progressive thrombosis, when there is a high probability of embolism and other complications.
Modern medicine offers a wide range of the latest minimally invasive procedures to get rid of complex blood clots without extensive surgery.
- A vena cava filter implanted in the inferior vena cava is an effective tool for trapping blood clots and reducing the risk of complications.
- Radiofrequency vessel obliteration involves sealing the vein and excluding the thrombus from the circulatory system.
- Laser coagulation , using high heat, can also isolate the affected vein and create a new path for blood flow.
- The use of sclerosants , which “glue” the vein together, reduces interference in the body to a minimum.
- Venous thrombectomy is the removal of a blood clot through a tiny incision using endoscopic instruments and a catheter.
It should be noted that most of these procedures take no more than 3 hours, after which the patient spends about a day in the outpatient clinic under the supervision of doctors, and the next day goes home.
Why are blood clots dangerous?
Thrombosis is so insidious that it can not make itself felt for a long time, and then lead to dire consequences. What is the nature of a blood clot, why are these formations so dangerous and how to identify them, said surgeon-phlebologist Andrei Maryasov.
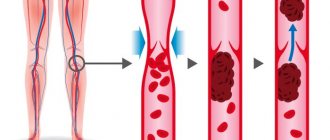
— What is thrombosis? — Thrombosis is the formation of dense masses from the blood. They are capable of blocking blood vessels, moving along them with the blood flow (for example, from the vessels of the lower extremities to the pulmonary artery) and can be fatal.
— Why do blood clots form? — In order for the blood to coagulate and form a blood clot, 3 conditions must be met: a violation of the integrity of the inner wall of the vessel, a slowdown in blood flow and a change in blood viscosity. The prerequisites for this triad are different: taking hormonal drugs or hormonal imbalance, lack of mobility, some chronic diseases, injuries (for example, when wearing a cast for a long time), extensive surgical interventions, varicose veins and others. By the way, studies have shown that varicose veins increase the risk of deep vein thrombosis of the lower extremities by 5 times. Statistics also show that the vast majority (more than 90%) of thrombosis is associated with the deep veins of the lower extremities. Blood clots formed in these vessels are able to migrate and move to the heart and pulmonary artery.
— How can you suspect thrombosis? — Some blood clots do not manifest themselves at all, but in most cases thrombosis is an acute condition. Swelling of the limb occurs (if we are talking about deep vein thrombosis of the legs) and bursting pain, the temperature of the limb decreases, and this condition requires an urgent call to the ambulance. Thrombosis of the superficial veins is less dangerous and has pronounced symptoms: swelling, redness, pain in the projection of the vein. In this case, it is easier to make a diagnosis and you can start treatment faster. With such symptoms, they turn to a surgeon, and urgently, otherwise the disease progresses and the blood clot can move into the deep veins.
— Are there degrees of complexity of the disease, when will prevention help, when will medications help, and when will only surgery help? - It depends on the blood clot itself. If it is floating, that is, there is an unattached element in the lumen of the vein, there is a high risk that it will come off, especially if it is more than 7 cm. In such cases, hospitalization and surgery are required. Small blood clots, securely attached to the walls of the vessel, are treated with medication. But in order to identify the type of blood clot, you must undergo an examination, do an ultrasound or MRI of the blood vessels and begin treatment.
— How long does it take for a blood clot to “mature” and why does it break off? “This happens very quickly, the blood clots in seconds. Blood clots tend to enlarge, so they can grow. And separation occurs because the part of the thrombus not attached to the wall becomes too long and heavy. A fresh blood clot is a soft, jelly-like structure, so in the first days blood clots are most dangerous. Gradually, the formation thickens, becomes stronger, and the risk of blood clot rupture decreases.
— Does the separation of a blood clot always lead to death? - Not always. Sudden death occurs if the blood clot is very large and, having come off, it closes the entire lumen of the vessel. But small blood clots are also dangerous: they can, for example, clog small pulmonary arteries and lead to partial death of some segment of the lung.
— There is a lot of advice on the Internet on how to thin the blood. Some people advise taking Aspirin. What blood thinning tips work and are universal? — You should not take any medications without a doctor’s prescription, and even more so, diagnose yourself with increased blood clotting. Only a doctor can come to this conclusion after studying the patient’s coagulogram, and if high blood viscosity is detected, medications are prescribed if necessary.
Prevention of thrombosis is an active lifestyle, proper drinking regimen and wearing compression stockings for people with chronic diseases (for example, varicose veins).
Still have questions? You can make an appointment with a phlebologist.
Why is it important to undergo treatment in a modern clinic?
Thrombophlebitis can be easily cured without surgery if the patient does not delay going to the doctor and does not self-medicate at home. This is why it is important to see a doctor at the first symptoms. The causes of the disease - inflammation of the vessel wall and blood clotting disorders - can only be eliminated through professional medical care provided by experienced doctors in a modern clinic. Not to mention acute forms of the disease, treatment of which is carried out only on an outpatient basis, since there is a risk of a threat to life.
What to do?
The appearance of symptoms of deep vein thrombosis of the lower extremities suggests that the patient should immediately consult a doctor and begin treatment. The specialist will assess the location and nature of the blood clot and help prevent it from breaking off or completely blocking the vessel.
Treatment usually includes blood thinners (heparin) and compression stockings to help promote proper venous blood flow. For several days, the patient may be recommended to rest in bed, with the legs positioned slightly elevated.
Surgical treatment is also possible, during which the blood clots are removed, and a special filter is installed in the vena cava to catch all moving blood clots.
Vein diseases associated with the formation of blood clots do not just make you feel worse and cause discomfort. They pose a real threat to life, so when the first symptoms of thrombophlebitis or thrombosis appear, you should consult a doctor. Only he will make an accurate diagnosis and prescribe treatment that will help avoid negative consequences. Self-administration of medications may not improve the situation, but may worsen it. The only thing that the patient is recommended to do on his own before visiting the doctor is to bandage his leg with an elastic bandage or wear compression stockings.