How common is extrasystole?
It is believed that extrasystole is observed in every person at some periods of life. With a single ECG recording in a group of healthy individuals, it is detected in 1.5-5% of cases. Daily monitoring reveals supraventricular extrasystoles in 14-91% and ventricular extrasystoles in 46-89% of healthy individuals. Although most of them are represented by single extrasystoles, complex forms can also be detected.
How often do doctors encounter extrasystoles?
Doctors deal with this diagnosis every day. Extrasystoles are diagnosed in 50-70% of all patients with rhythm disturbances, coronary heart disease and heart failure.
Causes of VES
PVC is always a secondary heart rhythm disorder, which means there is some underlying cause. The doctor needs to find her and influence her.
The reasons can be different: from stress and the presence of bad habits - smoking, alcohol, overeating, to pathologies of the cardiovascular system - ischemic heart disease, angina pectoris, hypertension, cardiomyopathy, heart defects, myocarditis. The reason may also be pathologies of other internal organs - lungs, gastrointestinal tract, cancer.
How dangerous is ventricular extrasystole?
Typically, doctors never tell a patient that something is threatening his life until they have carried out a comprehensive diagnosis and identified the root cause of the disease. There are safe extrasystoles that you shouldn’t even begin to treat, and there are those that require immediate action!
What is the diagnosis of VES?
The main thing is to understand whether the extrasystole threatens the patient’s life, whether it can lead to the most serious complication - sudden cardiac death!
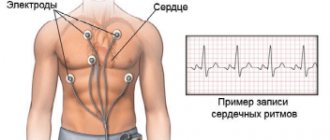
First, the doctor records the patient’s complaints, then refers him to functional tests of the heart. First of all, on a 12-lead ECG, then on 24-hour Holter monitoring and ultrasound of the heart. To exclude coronary pathology - stress tests. Depending on the results obtained, we may prescribe a CT scan, MRI, gastroscopy, blood tests, intracardiac electrophysiological study or genetic testing.
Are all patients eligible for treatment?
Not every PVC requires correction. Sometimes, on the contrary, you should not touch it, as therapy can cause even greater harm to health.
The choice of treatment tactics depends on whether the patient has organic heart damage or whether it is structurally normal.
In treatment, it is necessary to achieve three goals: reducing symptoms, eliminating hemodynamic disturbances, and improving prognosis.
But the key goal is to prevent sudden cardiac death. It must be emphasized that the main thing is to determine whether the patient has a risk of sudden cardiac death due to extrasystole.
Treatment approaches and techniques
PVC is of a secondary nature, so at the beginning of treatment it is important to identify the primary disease and act on it.
Next, this is the prescription of medications, including antiarrhythmics, sedatives, potassium and magnesium preparations.
If drug therapy is ineffective, radiofrequency ablation or implantation of a cardioverter-defibrillator is prescribed if the arrhythmia is prognostically dangerous.
If there is no heart damage, patients are advised to change their lifestyle. Elimination of overeating, heavy food, alcohol, smoking. Sometimes extrasystole can go away even after rest or a vacation trip.
Ventricular extrasystole - symptoms and treatment
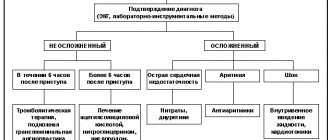
Once ventricular extrasystoles are detected in a patient, treatment should be selected taking into account the symptoms and the presence of dangerous types of extrasystoles.
The tactics for managing patients with ventricular extrasystole are as follows:
- observation without prescribing medications for patients with benign PVC, which is subjectively well tolerated (it is recommended to change lifestyle, eat a balanced diet, eliminate factors that provoke arrhythmia, adjust physical activity, etc.);
- in case of functional ventricular extrasystole (extrasystole caused by non-cardiac diseases) and extrasystole associated with heart pathologies, drug therapy is prescribed aimed at treating the underlying disease;
- treatment with antiarrhythmic drugs;
- the use of surgical treatment (radiofrequency ablation of the arrhythmogenic area of the myocardium, heart transplantation).
There are several main areas of treatment depending on the course, form and severity of PVCs.
1. If a person has no complaints, and the study reveals rare single monomorphic premature ventricular complexes that do not cause hemodynamic disturbances, no special therapy is required. In this case, the patient should give up caffeine-containing and alcoholic drinks, eliminate smoking, establish a daily routine, and ensure adequate sleep and rest. If there are any dysfunctions of the body associated with insufficient mobility, you need to increase physical activity in accordance with the body's capabilities. At the same time, it is necessary to exclude excessive physical activity (weight lifting, weightlifting). Your diet should include foods rich in potassium and magnesium: they have a beneficial effect on the cardiovascular system.
| Products containing potassium | Products containing magnesium |
| ⠀•⠀dried apricots; ⠀•⠀cocoa powder; ⠀•⠀wheat bran; ⠀•⠀raisins; ⠀•⠀sunflower seeds; ⠀•⠀nuts (pine nuts, almonds, peanuts, walnuts); ⠀•⠀legumes (peas, lentils, beans); ⠀•⠀jacket potatoes; ⠀•⠀avocado; ⠀•⠀ceps; ⠀•⠀bananas; ⠀•⠀citrus fruits; ⠀•⠀Brussels sprouts and kohlrabi; ⠀•⠀milk and fermented milk products; ⠀•⠀cereals (oatmeal, buckwheat, pearl barley, rice); ⠀•⠀fruits (peaches, pears, watermelon, apples, prunes, apricots, melon); ⠀•⠀chicory; ⠀•⠀vegetables (carrots, spinach, green onions, eggplant, cucumbers); ⠀•⠀chicken eggs; ⠀•⠀fish and meat; ⠀•⠀apple juice. | ⠀•⠀oil (sesame, flaxseed, peanut); ⠀•⠀cheese (Dutch, Poshekhonsky, goat, with mold); ⠀•⠀cottage cheese (low-fat and low-fat, curd cheese); ⠀•⠀bitter chocolate; ⠀•⠀almost all types of meat; ⠀•⠀fish (halibut, sturgeon, perch, haddock, cod, saury); ⠀•⠀duck eggs; ⠀•⠀cereals (rolled oats, chickpeas, peas, buckwheat, brown rice, lentils); ⠀•⠀fruits and berries (cherries, kiwi, pineapple, feijoa, raspberries, pears, peach, persimmon); ⠀•⠀many varieties of tea (for example, “Ivan-tea”) and juices; ⠀•⠀ginger; ⠀•⠀mustard; ⠀•⠀vanilla. |
2. When attacks of extrasystole are detected, which are accompanied by clinical symptoms, but do not disturb hemodynamics and have a benign course, beta-blockers (Bisoprolol, Metoprolol) are first prescribed. Sometimes, especially with functional ventricular arrhythmia against the background of vegetative-vascular dystonia and stressful conditions, drugs with sedative (Valemidin, Valerian) and anti-anxiety effects (Stresam, Adaptol), magnesium preparations (Magnerot) help in complex treatment , "Magne B6 forte"). It must be emphasized that the number of PVCs is taken into account when determining the degree of its malignancy. Frequent (up to 1000 or more per day) ventricular extrasystole in itself, even in the absence of obvious heart disease, is an indication for antiarrhythmic therapy.
Frequent PVCs and the appearance of paired, polytopic extrasystoles disrupt the movement of blood through the vessels, therefore, to reduce the risk of ventricular fibrillation and cardiac arrest, antiarrhythmic drugs are prescribed. It is preferable to use class I antiarrhythmics, and only if they are ineffective - Amiodarone or Sotalol. In parallel, drugs must be used to treat the underlying disease that caused the extrasystole[10]. To assess the results of treatment, as a rule, daily ECG monitoring is performed. A decrease in the number of PVCs by 75-80% indicates the effectiveness of therapy.
3. For PVCs of a malignant nature, it is necessary to prescribe highly effective drugs, such as Amiodarone and Sotalol. Sometimes they are combined with maintenance doses of beta-blockers. Treatment is usually carried out in a hospital setting, under ECG monitoring. In the hospital there are more opportunities to adjust hemodynamics and significantly reduce the risk of death in patients with cardiac arrhythmias.
Class I antiarrhythmics should not be taken if the patient has the following pathologies:
- severe signs of heart failure (low ejection fraction according to echocardiography);
- acute forms of coronary heart disease (acute infarction, progressive angina);
- previous myocardial infarction (especially if it was less than 6-12 months old);
- angina pectoris of functional classes III and IV (especially with proven coronary atherosclerosis);
- severe hypertrophy of the left ventricle with a thickness of more than 14 mm and/or the right ventricle (according to echocardiography);
- chronic heart failure class III-IV according to NYHA (New York Heart Association) and/or left ventricular ejection fraction less than 35%;
- pronounced dilatation (expansion of the chamber) of the left ventricle, cardiomegaly;
- active myocarditis;
- bundle branch block;
- severe bradycardia, etc.
If the patient does not have these contraindications and has moderately severe heart pathology, then the use of class I drugs can be considered [10]. It should be noted that antiarrhythmic drugs can have a proarrhythmic effect, i.e. cause a more dangerous arrhythmia, so only a doctor can prescribe them and only with appropriate indications.
Work has appeared that has shown the possibility of a beneficial effect of Omacor on ventricular arrhythmia, in particular in patients with coronary heart disease and chronic heart failure [6]. The addition of this drug to antiarrhythmics increases the effectiveness of treatment of ventricular arrhythmias. If the problem is associated with an electrolyte imbalance, then the patient is prescribed Magnesium sulfate or Potassium chloride.
The question of the duration of antiarrhythmic therapy is practically important. In patients with malignant ventricular arrhythmias, antiarrhythmic therapy should be continued indefinitely, in most cases for life. For less malignant rhythm disturbances, treatment should continue for up to several months with the possibility of gradual (due to the danger of rebound syndrome) its withdrawal. After stopping continuous therapy, the patient is advised to always carry a successfully used antiarrhythmic with him and take it in case of resumption of cardiac dysfunction.
4. For ventricular extrasystole, surgical treatment is possible. Indications for surgical intervention are:
- frequent (from several thousand to 20-30 thousand per day) ventricular extrasystole with an identified arrhythmogenic focus;
- ineffectiveness or impossibility of long-term use of antiarrhythmics in combination with poor tolerability or poor prognosis.
The high activity of the lesion makes it possible to detect it when drawing up a map of the electrical activity of the heart and perform radiofrequency ablation (RFA) of this myocardial zone[11]. The essence of the RFA technique is that a catheter is inserted into the patient through a large-caliber vessel, which is guided under the control of equipment to the very heart. First, using a special technique, the focus of pathological impulses is diagnosed, and then the site of ectopic excitation is exposed to a radiofrequency pulse, which leads to its destruction.
It is also possible to install an electrical pacemaker (ECS). The pacemaker is a device with electrodes that are attached to the ventricle and atrium during surgery. The electrodes create electronic impulses that cause the myocardium to contract. A pacemaker essentially replaces the sinus node, which is responsible for rhythm. It relieves a person from extrasystole and allows him to return to a full life.
In acute and chronic coronary heart disease, the development of ventricular arrhythmia is directly related to myocardial ischemia. In this regard, surgical myocardial revascularization (stenting, coronary artery bypass grafting) can improve electrical stability and reduce the likelihood of developing ventricular arrhythmias.
In patients with a high risk of sudden death and congestive heart failure, heart transplantation remains the main treatment option.
General information
The factors that caused the development of the disease can be of physiological and pathological origin. An increase in the tone of the sympathetic-adrenal system leads to an increase in the occurrence of extrasystoles. Physiological factors influencing this tone include the consumption of coffee, tea, alcohol, stress and nicotine addiction. There are a number of diseases that lead to the formation of extrasystole:
- cardiac ischemia;
- myocarditis;
- cardiomyopathy;
- heart failure;
- pericarditis;
- hypertonic disease;
- osteochondrosis of the cervical spine;
- prolapse of the mitral valve leaflets;
- cardiopsychoneurosis.
There is a certain connection between the patient’s age, time of day and the frequency of extrasystoles. Thus, more often the ventricular type is present in people over 45 years of age. Dependence on circadian biorhythms is manifested in the registration of extraordinary heart contractions, more in the morning hours.
Ventricular extrasystole threatens the patient’s life. Its formation increases the risk of sudden cardiac arrest or ventricular fibrillation.
Reasons for development
Irregularities and heart diseases are the main reasons why PVCs develop. Also, ventricular arrhythmia can be triggered by heavy physical work, chronic stress and other negative effects on the body.
From cardiac pathologies:
| Heart failure | Negative changes in the muscle tissue of the heart muscle, leading to disruption of the inflow and outflow of blood. This is fraught with insufficient blood supply to organs and tissues, which subsequently causes oxygen starvation, acidosis and other metabolic changes. |
| Coronary heart disease (CHD) | This is damage to the heart muscle due to impaired coronary circulation. IHD can be acute (myocardial infarction) or chronic (with periodic attacks of angina). |
| Cardiomyopathy | Primary myocardial damage, leading to heart failure, atypical beats and heart enlargement. |
| Heart disease | Defect in the structure of the heart and/or major outflow vessels. Heart disease can be congenital or acquired. |
| Myocarditis | An inflammatory process in the heart muscle that disrupts impulse conduction, excitability and contractility of the myocardium. |
Taking certain medications (incorrect dosage, self-medication) can also affect the functioning of the heart:
- Ventricular extrasystole
| Diuretics | Medicines in this group increase the rate of urine production and excretion. This can provoke excessive excretion of the “heart” element - potassium, which is involved in the formation of the impulse. |
| Cardiac glycosides | The drugs are widely used in cardiology (they lead to a decrease in heart rate and an increase in the force of myocardial contraction), but in some cases they cause side effects in the form of arrhythmia, tachycardia, atrial fibrillation and ventricular fibrillation. |
| Drugs used for heart blocks (M-anticholinergics, sympathomimetics) | The side effects of the drugs manifest themselves in the form of stimulation of the central nervous system, increased blood pressure, which directly affects heart rhythm. |
Also, the development of PVCs can be affected by other pathologies not associated with disruption of the cardiovascular system:
- Diabetes mellitus type 2 . One of the serious complications of the disease associated with carbohydrate imbalance is diabetic autonomic neuropathy, which affects nerve fibers. In the future, this leads to a change in the functioning of the heart, which “automatically” causes arrhythmia.
- Hyperfunction of the thyroid gland (moderate and severe thyrotoxicosis). In medicine, there is such a concept as “thyrotoxic heart,” which is characterized as a complex of cardiac disorders - hyperfunction, cardiosclerosis, heart failure, extrasystole.
- In diseases of the adrenal glands, there is an increased production of aldosterone, which in turn leads to hypertension and metabolic disorders, which is interconnected with the work of the myocardium.
Ventricular extrasystole is not of an organic nature (when there are no concomitant cardiac diseases), caused by a provoking factor, often has a functional form. If you remove the negative aspect, then in many cases the rhythm returns to normal.
Functional factors of ventricular extrasystole:
- Electrolyte imbalance (reduction or excess of potassium, calcium and sodium in the blood). The main reasons for the development of the condition are changes in urination (rapid production or vice versa, urinary retention), malnutrition, post-traumatic and postoperative conditions, liver damage, and surgery on the small intestine.
- Substance abuse (smoking, alcohol and drug addiction). This leads to tachycardia, changes in material metabolism and disruption of myocardial nutrition.
- Disorders of the autonomic nervous system due to somatotrophic changes (neuroses, psychoses, panic attacks) and damage to subcortical structures (occurs with brain injuries and pathologies of the central nervous system). This directly affects the functioning of the heart and also provokes surges in blood pressure.
Ventricular extrasystoles disrupt the entire heart rhythm. Pathological impulses over time have a negative effect on the myocardium and the body as a whole.