Treatment under the compulsory medical insurance policy is possible!
Submit your application
Follow the news, subscribe to our social networks
Details
Paget-Schroetter syndrome is a thrombosis of the subclavian vein, extending to the subclavian and axillary veins, as well as to the veins of the shoulder, which leads to impaired venous outflow in the arm. The syndrome is also called traumatic thrombosis or effort syndrome. Despite its relative rarity, it has become increasingly diagnosed in the last decade. The main complaints are swelling of the tissues of the upper limb and bursting pain.
The first case of the syndrome was described by James Paget in 1875, and in 1894 von Schrötter identified vascular injury as a potential cause of the disease. The term Paget-Schroetter syndrome was first used in 1948.
Causes and risk factors
Subclavian vein thrombosis is associated with compression of the thoracic outlet. The subclavian vein originates from the first rib from the axillary vein, and at the level of the sternoclavicular junction with the jugular vein it forms the brachiocephalic vein. Compression of the vein walls in the area between the collarbone and the first rib leads to slower blood flow and thrombosis. It can be considered the venous equivalent of thoracic outlet syndrome.
One of the causes of thrombosis is muscle hypertrophy (increase in the volume or mass of skeletal muscles). As a result, the subclavian vein can become compressed between the ribs (in front of it), the muscle (behind it), and the collarbone (above it).
Another reason is that a person has a congenital small anatomical space between the collarbone and the first rib. In this case, compression of the subclavian vein is possible even without major muscle hypertrophy.
Other causes of thrombosis include:
- incorrect posture,
- bone pathology (in the subclavian region),
- collarbone fractures
- use of subclavian catheters
- incorrect sleeping position
- thoracic outlet syndrome
- Risk factors include excessive physical activity. People who undergo intense physical activity and athletes (wrestlers, weightlifters or bodybuilders) have a higher risk of developing thrombosis due to repeated damage to the subclavian vein from frequent mechanical compression of the vessels between the collarbone, first rib and joint.
The average age of patients with Paget-Schroetter syndrome is 30-40 years, and the male to female ratio is approximately 2:1. It is more common on the right side, probably due to the frequency of right hand dominance, and 60% to 80% of patients have this condition. who performed vigorous exercise involving the upper limbs.
Causes of jugular vein thrombosis
The most common cause of jugular vein thrombosis is exogenous interventions, namely, placement of a catheter during infusion therapy. Thrombosis develops while the patient is in a hospital, but sometimes the symptoms of this pathology occur hidden. Indeed, during therapy, most patients receive antiplatelet agents and anticoagulants. Therefore, acute jugular vein thrombosis is observed after discharge from the hospital.
Other causes of jugular vein thrombosis include:
- Mechanical compression of the vein.
- Features of the anatomical structure of the human skeleton.
- Heavy physical activity.
- Installation of a pacemaker.
- The patient undergoes radiation therapy.
- Virchow's triad as a cause of thrombosis of the internal jugular vein. It includes:
- Damage to the inner layer of the vein, for example, when a catheter is left in it for a long time. Sometimes such disorders are typical for people who inject drugs.
- Slowing of blood flow in the vein, which may be due to the presence of a tumor compressing the vein.
- Blood clotting disorders, for example, due to chronic or acute diseases.
In addition to the main causes of jugular vein thrombosis, there are additional risk factors that increase the likelihood of its occurrence.
These include:
- Senile age.
- Excess body weight.
- Infectious diseases that can damage the venous wall.
- Bad habits: drug addiction, smoking, alcohol abuse.
- Previous surgical interventions on the neck.
- Diseases of the cardiovascular system.
- Kidney damage.
- The period of menopause in women.
- Uncontrolled use of oral contraceptives.
- Physical inactivity.
- Systemic diseases of the body.
Course of the disease
The course of the disease is divided into two stages: acute (lasts about three weeks; at the initial stage, symptoms appear during physical activity) and chronic (symptoms last for more than two months).
The acute phase is characterized by increasing swelling of the arm, pain, and a feeling of fullness. The patient's ability to work decreases. Gradually, tense saphenous veins develop, which take on the function of outflow of venous blood and contribute to the subsidence of the process.
The chronic phase is the consequences of thrombosis. With inadequate treatment, occlusion of the subclavian vein persists and chronic Paget-Schroetter syndrome develops. It is characterized by the development of a powerful collateral network of saphenous veins around the shoulder joint. Patients are concerned about the increase in volume of the sore arm, sometimes there is pain and increased fatigue.
Features of the disease and ICD classification
This disease is a pathological condition caused by blockage of the vessel cavity with a blood clot, which causes blood flow disturbances and, as a result, some organs and systems suffer. The lack of adequate therapy can cause the development of a number of rather dangerous complications, so it is extremely important to stop not only its manifestations, but also the cause itself.
It is impossible to unambiguously answer the question about the age category of patients suffering from this disease. Both young people and elderly people are susceptible to it, but in the latter the disease is somewhat more common. Doctors also note that gender may be a risk factor. Thus, among patients who come to medical institutions with a similar problem, the majority are men.
According to the international classification of diseases, created to systematize the statistical information obtained, this pathology has ICD 10 code I82.
Forecast
Life-threatening complications are rare. Pulmonary embolism is observed in only 2% of cases of subclavian thrombosis. Even with immediate intervention, some patients do not fully regain arm function and may have residual symptoms or require continued treatment. Severe venous insufficiency of the arm usually does not occur. Thrombosis of the subclavian vein does not pose a serious threat to life. After adequate treatment, the edema decreases significantly, but complete patency is rarely restored. If the causes for subclavian thrombosis persist, relapses of the disease may occur, so it is necessary to identify and eliminate them. As a reminder of the history of venous thrombosis, the patient is left with an increase in the volume of the shoulder and a network of visible saphenous veins in the area of the shoulder joint.
Diagnosis of jugular vein thrombosis
Diagnosis of thrombosis of the internal jugular vein most often does not cause difficulties for the doctor. It is based on the listed symptoms, but must be supplemented with instrumental methods. Preference should be given to computed tomography or MRI, as the most informative diagnostic methods. Although most often the patient undergoes an ultrasound (duplex scanning, Doppler sonography). In principle, the jugular vein is well accessible to ultrasound, so most often the diagnosis is correct. In this case, it is imperative to distinguish thrombosis from an abscess, necrotic tumor and inflamed lymph nodes.
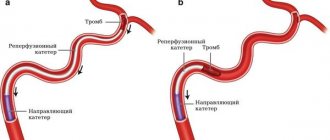
The extent of thrombosis can be assessed and the location of the thrombus can be determined using phlebography using a contrast agent. However, venography should be prescribed only to those patients who will receive thrombolytic therapy. After the procedure, a fibrinolytic agent is immediately administered into the vein.
Surgical intervention
If conservative therapy does not bring the desired result, minimally invasive surgical procedures can be used to eliminate the blood clot. The frequency of surgical treatment for this disease is significantly inferior to classical therapy.
The most common methods are:
- Aspiration thrombectomy is the mechanical removal of thrombolytic mass through a puncture made through the skin.
- Endovascular thrombolysis is the delivery of a thrombolytic drug directly to the site of a vascular lesion by subcutaneous insertion of a special catheter. Thus, its patency is partially or completely restored.
Read about the manifestations and methods of treating varicocele on both sides in our material.
Drug treatment
The basis of therapy for the formation of blood clots in the circulatory system is the use of direct and indirect anticoagulant drugs. They are aimed at thinning the blood by reducing the level of fibrinogen, a substance whose concentration increases to form clots.
Direct anticoagulants include:
- Fibrinolysin,
- Fraxiparine,
- Heparin.
After a decrease in the prothrombin index, they switch to medications with an indirect anticoagulant effect, such as Curantil or Aspirin.
Another important aspect in complex therapy is the prescription of phlebotonics, whose action is aimed at improving metabolic processes and eliminating inflammation.
Remember! The dosage of any medications and the method of their use are prescribed exclusively by a competent medical professional.
If necessary, antispasmodics are prescribed to reduce the tone of the vascular walls and relieve pain. The addition of sepsis indicates the need for antibacterial therapy.
You can find out what varifort for varicose veins is and the opinion of Elena Malysheva from our article.
Causes
Thrombosis of the internal, external and external jugular veins, in contrast to the venous system located in the lower extremities, is much less common in medical practice.
It is impossible to unambiguously identify the factor influencing the formation of a blood clot that clogs the lumen of blood vessels.
Most often, the cause of the development of the pathological condition is damage to the vascular walls due to mechanical stress. Due to the intensive production of platelets and fibrin, the body independently “patches” damage, thereby forming blood clots.
However, there are a number of reasons not related to mechanical damage. Depending on their origin, thrombosis factors are conventionally divided into three groups: hereditary, acquired and complex. Let's look at each of them in more detail.
Hereditary
These factors include:
- congenital mutations;
- anomalies in the structure of the venous system;
- deficiency of C and S – proteins and antithrombin 3 substance;
- congenital changes in coagulation;
- some autoimmune diseases, such as systemic lupus erythematosus.
Purchased
There is a fairly large number of reasons that form the tendency to the appearance of this pathology, acquired during life. These include:
- Carrying out orthopedic operations and the postoperative period.
- Insertion of intravenous catheters.
- Obesity and low physical activity.
- Postpartum period.
- Long-term fixation of the limbs with a plaster cast.
- Taking hormonal contraceptives and increasing estrogen levels.
- Frequent and long flights.
- Smoking.
- Peptic ulcer disease.
- The presence of benign or malignant neoplasms.
- Receiving chemotherapy.
Complex
Doctors include increased levels of fibrinogen, some coagulation factors and homocysteine as complex factors.
Symptoms
The manifestation of classic symptoms of such a disease directly depends on the degree of blockage of the vessel by a blood clot. If its size is insignificant and the blood flow is practically not disturbed, the disease is asymptomatic, without causing discomfort to the person. Therefore, the patient most often does not suspect its presence.
If thrombosis of the jugular vein in the neck is provoked by an almost complete blockage of its cavity, then the following typical signs are inevitable:
- Painful sensations in the neck and collarbone area . Sometimes the pain spreads to the shoulder and arm, which significantly interferes with identifying the location of the blood clot. The pain syndrome in this pathology is constant, aching in nature.
- Swelling of the neck in the area where the affected vessel is located , with its obvious bulging, which is noticeable even in the absence of stress on the throat, such as singing or screaming. The swelling can increase in the first hours, the neck at the site of its appearance hurts with any influence (palpation, contact with clothing).
- Change in the skin in the affected area to a red-bluish color.
- There may be limited mobility of the upper limbs due to muscle weakness.
- Headache caused by poor blood flow.
Such symptoms do not become permanent. There are two possible options for the further development of the disease: the onset of a subsiding stage or transition to a chronic form. If the first is characterized by a gradual decrease in negative manifestations, up to their almost complete disappearance, then in the second case, the unpleasant sensations are dulled, but do not completely disappear.
If any of the above clinical manifestations appear, you should immediately seek medical help.
Prevention
To prevent the development of pathology, you first need to be attentive to your own health and undergo regular medical examinations. If a person is at risk, it is necessary to systematically conduct a study such as coagulometry - a blood test for clotting. Thus, it is possible to promptly detect hypercoagulation leading to the formation of blood clots in the vascular system.
Particular attention should be paid to the choice of clothing. It should not hinder movement or squeeze the body. For everyday wear, preference should be given to loose items made from natural fabrics and of appropriate size. We described how to avoid varicose veins on the legs in our article.
Compliance with the drinking regime will prevent dehydration of the body and, as a result, thickening of the blood. Therefore, the minimum amount of clean water consumption should be 2 liters per day.
Giving up bad habits, adjusting your diet and diet, and daily moderate physical activity have a beneficial effect on the general condition of the body. Excluding fried and fatty foods from the menu reduces the chances of developing thrombosis, both of the superior jugular vein and similar pathologies everywhere.
We talked about whether an exercise bike will help with varicose veins here.
Anatomical features
In order to better understand the mechanisms of occurrence and possible localization of pathology, one should turn to anatomy.
In the human body there are 3 main pairs of jugular veins susceptible to thrombosis:
- Internal . The largest among the listed vessels, responsible for the drainage of blood from the skull and normal metabolism in the brain. The venous line begins from the jugular foramen, descends to the area of the sternoclavicular junction, and merges with the subclavian artery. In medical practice, it is most often used for the purpose of catheterization for hemodialysis, plasmapheresis, and long-term infusion therapy.
- Outdoor _ In terms of its size, it ranks second among the vessels of this system and is responsible for draining blood saturated with carbon dioxide from the external parts of the cervical spine and head. It is located close enough to the surface that it can be seen and felt.
- Front . The pair is located under the chin and is part of the venous arch.
Each of these pairs is susceptible to thrombosis, but as statistics show, it is the outer vessel that most often clogs the thrombus.
Diagnostics
If characteristic complaints appear, the first priority is to consult a doctor. This may be a therapist or phlebologist who will collect an anamnesis of the disease based on the patient’s complaints and visual examination.
However, for an accurate diagnosis, it is necessary to conduct instrumental and laboratory studies to establish the location, extent of the lesion and determine the quality of blood parameters. The following diagnostic methods are widely used:
- Ultrasound examination with Dopplerometry of the vascular network of the neck and head. The most informative diagnostic method, which allows not only to determine the exact location of the blood clot, but also to determine the disturbance of blood flow. When symptoms of jugular vein thrombosis appear, this study is prescribed first.
- Magnetic resonance imaging. MRI is used to study the condition of internal organs and tissues. Has the highest accuracy of any commonly used imaging modality such as radiography or computed tomography.
- Thrombodynamics . With its help, clotting disorders are identified and, based on the results obtained, the most effective therapy and dosage of thinning drugs are selected.
- Thrombin generation test . Thrombin acts as a catalyst in the process of transforming fibrinogen into fibrin. It is also often used in the practice of cardiologists and phlebologists.
- Thromboelastography . An instrumental method for assessing the viscosity of a blood clot, the result of which is displayed on paper.
- Prothrombin time test . Shows the clotting time of plasma under the influence of specially added thromboplastin.
Also, the attending physician may prescribe additional diagnostic methods, at his discretion, based on the specific situation. Read about how to diagnose and treat internal varicose veins in the legs in our material.
This is interesting! Contraindications to magnetic resonance venography include installed dental implants, braces and braces.