During a consultation with a cardiologist or surgeon, the patient may be diagnosed with an enlarged jugular vein in the neck; the causes of this phenomenon vary. Depending on the predisposing factors, a treatment regimen is prescribed.
The function of the jugular veins is to be responsible for the process of blood flow from the brain to the neck. Thanks to these blood veins, unpurified blood flows to the heart muscle so that the filtration process can take place.
Jugular veins are divided into several types:
- Internal. It is located at the base of the skull, and its end is in the region of the subclavian fossa. At this site, the vein pours unpurified blood into the brachiocephalic vessel.
- The external one begins under the auricle, goes down to the sternum and collarbone, enters the internal jugular vein, as well as the subclavian vein. This vessel has valves and processes.
- The anterior one originates from the outer part of the mylohyoid muscle and flows near the midline of the neck. This vein enters the subclavian and external, thereby forming an anastomosis.
Why is this happening
Phlebectasia disrupts the functioning of valves and blood vessels. The regulation of venous blood flow is suspended. Clots appear. With a large number of such formations, dysfunction of the entire venous network develops.
If the jugular vein is dilated even slightly, it is manifested by the following symptoms:
- swelling of the cervical vessels, their enlargement;
- the appearance of a blue sac on the upper section of the vein;
- swelling of the neck;
- a feeling of tightness that occurs when turning the head;
- breathing problems;
- pain when touching the neck;
- loss of voice.
Signs of pathology depend on the stage:
- Swelling of blood vessels in the neck. The patient does not feel any discomfort. A sign of pathology is identified during a visual examination.
- Drawing pain. The patient's intravenous pressure increases if he makes rapid and sudden head movements.
- Acute pain of high intensity. The man's voice is hoarse. Breathing is difficult.
When the left or right internal jugular vein expands, disturbances in the activity of the circulatory system occur.
Phlebectasia can occur at any age. Probable reasons:
- Injuries to the ribs on the left or right, neck, spinal column, which leads to stagnation of unpurified blood.
- History of concussion.
- Osteochondrosis in a patient.
- Pathologies of the cardiovascular system. Phlebectasia affects people with heart failure, ischemia, and hypertension.
- Endocrine pathologies.
- Prolonged work at the computer.
- Benign and malignant tumors.
The disease takes time to develop. Even if a person has predisposing factors, this does not mean that he is already sick. It is necessary to monitor your health more carefully.
Predisposing factors include:
- insufficient development of connective tissue cells;
- hormonal changes in the body;
- back injuries, including fractures;
- intervertebral hernia;
- staying in an uncomfortable position for a long time;
- wrong diet.
Hormonal causes of pathology are more common in women. During puberty and pregnancy, there is a risk that the veins will swell.
Other factors include depression and stress. The jugular veins have nerve endings. If all is well, these endings form venous vessels of high elasticity. But when a person is stressed, intravenous pressure increases, which impairs the elasticity of the veins.
Other unfavorable factors include:
- alcohol abuse;
- smoking;
- eating foods with toxins;
- increased stress on the body - at the physical and mental levels.
Types and location
The venous vein consists of 3 independent venous channels. Accordingly, their anatomy is separate.
The veins of the head and neck, which are responsible for the correct outflow of blood from the brain cavity, are divided into 3 types. These are the anterior, external and internal jugular veins.
Internal
It has a relatively wide trunk, compared to the other 2. In the process of pushing out blood, it easily expands and contracts, thanks to its thin walls and diameter of 20 mm. The outflow of blood in a certain amount occurs with the help of valves.
As the lumen expands, the superior bulb of the jugular vein is formed. This occurs at the moment when the IJV enters from the hole.
Typical anatomy diagram:
- start – area of the jugular foramen;
- localization - the skull, or rather its base;
- further - its path goes down, the place of localization is in the posterior muscle, the place of attachment is the collarbone and sternum;
- the place of intersection with the posterior muscle is the area of its lower and posterior parts;
- after that the path is laid along the trajectory of the carotid artery;
- a little lower it comes forward and is located in front of the carotid artery;
- then, together with the carotid artery and the vagus nerve, they are directed through the site of expansion;
- as a result, a powerful bundle of arteries is created, which includes the carotid artery and all jugular veins.
Outdoor
Location: neck tissue. Blood is directed from the face, head and outer part of the cervical region. Perfectly visible visually when coughing, screaming or stress.
- origin - lower angle of the jaw;
- further down the muscle that attaches the sternum and clavicle;
- crosses the outer part of the muscle. The place of intersection is the area of the rear and lower part.
It has only 2 valves located in the initial and middle parts of the neck.
Front
The main task is to carry out drainage from the chin area. Location: neck, middle line.
- passes along the muscle of the tongue and jaw (along the front), downwards;
- Then, on both sides, the veins connect with each other, and a venous arch is formed.
Sometimes an arc of channels collected together forms a middle one.
What to do
If an increase is noticed on the right or on the other side, there is a possibility that this is only the first stage. But you should not self-medicate. With such a sign, you need to consult a doctor, who will make a diagnosis based on a visual examination.
To identify pathology that has reached the second or third stage, research is carried out. If a patient comes to an appointment complaining of pain, there is a possibility that blood flow is disrupted. The doctor prescribes laboratory tests - CBC - and instrumental research methods:
- CTG of the skull, as well as the cervical and thoracic regions;
- Ultrasound of the same areas;
- MRI using contrast agent;
- puncture for diagnostic purposes.
Sometimes a joint consultation with a vascular surgeon, general practitioner, neurologist, cardiologist, endocrinologist and a doctor specializing in oncological pathologies is necessary.
When prescribing treatment, take into account:
- localization of the disease;
- research results;
- the degree to which symptoms affect the body.
For example, the presence of venous cervical seals on the right does not pose a significant threat. But the disease on the left side is more dangerous: there is a risk of disorders of the lymphatic system if a thorough diagnosis is carried out.
The patient may be prescribed a course of medication. Drugs are prescribed that can remove inflammatory processes, eliminate swelling, and strengthen vascular walls.
If the patient is diagnosed with the third stage, surgical treatment is indicated. Operations are performed to remove the affected areas of the veins. The healthy parts of the veins are connected to form a new vessel.
The same methods are used to treat children. During therapy at an early age, surgical intervention is more often required.
What to do to prevent the disease from occurring is to take preventive measures. Among them:
- avoiding excessive physical or mental stress;
- if possible, no stress on the cervical spine if there is a predisposition to phlebectasis or primary signs of vein dilation;
- timely treatment of diseases that can lead to phlebectasis;
- Regular examinations by specialists will help identify the disease at an early stage and quickly treat it;
- maintaining a healthy lifestyle;
- moderate sports activity;
- balanced diet.
Treatment
Pre-hospital assistance
In case of traumatic injuries, the neck must be secured with a cotton-gauze collar. In other cases, it is recommended to provide functional rest to the neck and not self-medicate, since swelling occurs in many diseases that require different approaches to therapy. In case of intense pain, the use of painkillers is allowed. You should not warm your neck - this can intensify inflammatory and other pathological processes.
Conservative therapy
The conservative treatment regimen includes a protective regimen, etiopathogenetic and symptomatic drug therapy, and physical therapy. The following medications are used:
- NSAIDs
. They are used in the form of tablets, injections, and local remedies. They have analgesic and anti-inflammatory effects. - Antibiotics
. Broad-spectrum medications are prescribed, and after culture results are obtained, medications are replaced taking into account the sensitivity of the pathogen. For extensive purulent processes, combinations of two drugs are recommended. - Antithyroid drugs
. Hyperthyroidism is considered as an indication for the use of medications. For hypothyroidism, replacement therapy is carried out. - Antihistamines
. Necessary for neck swelling caused by allergic reactions.
After eliminating acute phenomena, UHF, laser therapy, electrophoresis with novocaine, and anti-inflammatory drugs are used. Patients with cancer undergo chemotherapy and radiation therapy.
Surgery
For acute pain, blockades with local anesthetics are performed. Taking into account the nature of the pathology, the following operations are performed:
- Traumatic injuries
: transoral fixation, application of a Halo-apparatus, PSO of neck wounds, tracheostomy, chordectomy, resection of the larynx, laryngopexy, removal of foreign bodies of the larynx, reconstructive interventions. - Maxillofacial pathologies
: parotidectomy, opening of abscesses and phlegmons of the neck, dilation of the excretory duct of the salivary gland. - Endocrine diseases
: enucleation of the node, subtotal resection of the thyroid gland, hemithyroidectomy. - Otolaryngological diseases
: removal of a median or lateral neck cyst, opening of a retropharyngeal abscess. - Tumors
: excision of lipomas and fibromas of the neck, removal of the thyroid gland, radioiodine therapy for thyroid cancer, laryngectomy, laryngopharyngectomy, hemilaryngectomy, installation of a voice prosthesis, Krail, Vanach operations.
Why is the phenomenon dangerous?
It is important to prevent complications, for which you should adjust your lifestyle, especially if there were people with phlebectasis in your family.
It is especially dangerous if the pathology occurs in a child. The disease is diagnosed immediately after birth, sometimes at 3-5 years. This is indicated by tumor-like neoplasms, vasodilatation, and elevated temperature.
Thrombosis becomes a complication. A clot forms inside the vessel. This indicates the presence of chronic diseases in the body. The danger of a blood clot is that it can break off and block the functioning of vital veins.
For those who experience thrombosis, the doctor recommends anticoagulants. Antispasmodics, venotonics, and nicotinic acid are used to relieve inflammation, relax muscles, and make the blood more fluid. The drugs also help in resolving the blood clot. If the therapeutic regimen is successful, there is no need to perform surgery.
To avoid complications, when signs appear, you need to come for a diagnosis and take therapeutic measures. If you do not control the course of the pathological process, consequences arise. For example, the affected area may rupture, causing hemorrhage. The most unfavorable outcome is the death of the patient.
Diseases and changes
The reasons for the expansion make it known about the dysfunction of the circulatory system. This situation requires an immediate solution. You should know that there are no age restrictions for YV pathologies. They affect both adults and children.
Phlebectasia
A thorough, accurate diagnosis is necessary, the result of which should be the identification of the causes of the pathology, as well as the prescription of comprehensive effective treatment.
Extensions occur:
- in case of stagnation, due to injury to the neck, spine or ribs;
- for osteochondrosis, concussion;
- for ischemia, hypertension, heart failure;
- for endocrine disorders;
- with prolonged sitting at work;
- for malignant and benign tumors.
Phlebectasis can also be caused by stress and nervous tension. With nervous excitement, pressure can increase, resulting in a loss of elasticity of the walls of blood vessels. This can lead to valve dysfunction. Therefore, phlebectasia needs to be detected early.
Circulation can be negatively affected by factors such as: alcohol consumption, smoking, toxins, excessive mental and physical stress.
Thrombosis
It may occur due to the presence of a chronic disease in the body. If they are present, as a rule, blood clots form in the vessels. Once a blood clot has formed, there is a possibility of it breaking off at any time, which entails blocking vital arteries.
Signs of thrombosis:
- sometimes pain occurs in the hand;
- swelling of the face;
- appearance of venous networks on the skin;
- When turning the head, pain occurs in the cervical region and neck.
The result of thrombosis can be rupture of the jugular venous channels, which leads to death.
Phlebitis and thrombophlebitis
Inflammatory changes occurring in the mastoid process or middle ear are called phlebitis. The cause of phlebitis and thrombophlebitis can be:
- bruises, wounds;
- placement of injections and catheters in violation of sterility;
- penetration of medications into the tissues around the vessel. This can often be triggered by calcium chloride when it is injected past an artery;
- infection from the skin.
Phlebitis can be uncomplicated or purulent. The treatment of the 2 pathologies is different.
Aneurysm
A rare pathology is an aneurysm. It can even occur in children at an early age from 2 to 7 years. The pathology has not been fully studied. It is believed that its occurrence occurs from improper development of the base of the venous bed, or rather its connective tissue. It is formed during intrauterine development of the fetus. The anomaly does not manifest itself clinically. It can only be noticed when a child cries or screams.
Jugular vein and its diseases
Have you been struggling with HYPERTENSION for many years without success?
Head of the Institute: “You will be amazed at how easy it is to cure hypertension by taking it every day.
The jugular veins belong to the superior vena cava system and are responsible for the outflow of blood from the head and neck. Another name for them is jugular. These are three paired vessels: internal, external, anterior.
A little anatomy
The main volume of blood is drained from the head and neck through the largest of the jugular ones - the internal one. Its trunks reach a diameter of 11-21 mm. It begins at the cranial jugular foramen, then expands to form the sigmoid sinus, and descends down to the place where the clavicle connects to the sternum. At the lower end, before connecting with the subclavian vein, it forms another thickening, above which, in the neck area, there are valves (one or two).
Our readers successfully use ReCardio to treat hypertension. Seeing how popular this product is, we decided to bring it to your attention. Read more here...
The internal jugular vein has intracranial and extracranial tributaries. Intracranial - these are the sinuses of the dura mater with the veins of the brain, orbits, hearing organs, and skull bones flowing into them. Extracranial veins are vessels of the face and the outer surface of the skull that flow into the internal jugular along its course. The extracranial and intracranial veins are connected to each other by ligaments that pass through special cranial foramina.
The internal jugular vein is the main line that drains blood saturated with carbon dioxide from the head. This vein, due to its convenient location, is used in medical practice to place catheters to administer medications.
The second most important is external. It runs under the subcutaneous tissue along the front of the neck and collects blood from the outer parts of the neck and head. It is located close to the surface and is easily palpable, especially noticeable when singing, coughing, screaming.
The smallest of the jugular veins is the anterior jugular, formed by the superficial vessels of the chin. It runs down the neck, merging with the external vein under the muscle connecting the mastoid process, sternum and clavicle.
Functions of the jugular veins
These vessels perform very important functions in the human body:
- They provide reverse blood flow after it is saturated with carbon dioxide, metabolic products and toxins from the tissues of the neck and head.
- Responsible for normal blood circulation in the cerebral sections.
Catheterization
For venous access in medical practice, the right internal jugular vein or the right subclavian vein is usually used. When performing the procedure on the left side, there is a risk of damage to the thoracic lymphatic duct, so it is more convenient to perform manipulations on the right. In addition, the left jugular trunk carries blood outflow from the dominant part of the brain.
According to doctors, puncture and catheterization of the internal jugular vein is preferable to that of the subclavian veins, due to fewer complications, such as bleeding, thrombosis, and pneumothorax.
Main indications of the procedure:
- Impossibility or ineffectiveness of drug administration into peripheral vessels.
- Upcoming long-term and intensive infusion therapy.
- The need for diagnostics and control studies.
- Carrying out detoxification using plasmapheresis, hemodialysis, hemoabsorption.
Catheterization of the internal jugular vein is contraindicated if:
- history of surgery in the neck area;
- blood clotting is impaired;
- there are ulcers, wounds, infected burns.
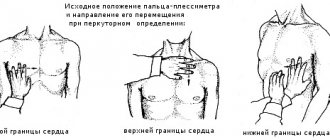
There are several access points to the internal jugular vein: central, posterior and anterior. The most common and convenient of them is the central one.
The technique for vein puncture using central access is as follows:
- The patient is placed on his back, his head is turned to the left, his arms are along his body, the table on the side of his head is lowered by 15°.
- The position of the right carotid artery is determined. The internal jugular vein is located closer to the surface parallel to the carotid vein.
- The puncture site is treated with an antiseptic and limited with sterile napkins, lidocaine (1%) is injected into the skin and subcutaneous tissue and the search for the location of the vein begins with an intramuscular search needle.
- The course of the carotid artery is determined with the left hand and the needle is inserted 1 cm lateral to the carotid artery at an angle of 45°. Slowly advance the needle until blood appears. Inject no deeper than 3-4 cm.
- If it is possible to find a vein, the search needle is removed and a needle from the set is inserted, remembering the path, or the needle from the set is first inserted in the direction found by the search needle, then the last one is removed.
Catheter placement is usually done using the Seldinger technique. The injection technique is as follows:
- You need to make sure that blood flows freely into the syringe and disconnect it, leaving the needle.
- A guidewire is inserted into the needle approximately half its length and the needle is removed.
- The skin is incised with a scalpel and a dilator is inserted through the guidewire. The dilator is taken with the hand closer to the body so that it does not bend and injure the tissue. The dilator is not completely inserted; it only creates a tunnel in the subcutaneous tissue without penetrating the vein.
- The dilator is removed, the catheter is inserted and the guidewire is removed. They do a test for an allergic reaction to the drug.
- By the free flow of blood, you can understand that the catheter is in the lumen of the vessel.