- How does ascites manifest?
- What causes fluid to accumulate?
- Risk factors for ascites
- Classification and types of ascites
- How to treat ascites?
- Clinical case
- What causes ascites to develop in cancer?
- Features of the treatment of ascites in cancer patients
- Conservative therapy
- Surgical treatment of ascites
- Methods for diagnosing ascites
- Possible complications of ascites
- Forecast
- Prevention of ascites
- Prices
Euroonco doctors specialize in working with patients with ascites. Features of our treatment of ascites:
- We provide comprehensive treatment. During laparocentesis (a puncture of the abdominal wall to remove fluid from the abdomen), we install temporary or permanent peritoneal catheters, as well as port systems. This allows the patient not to be limited in movement.
- If this is indicated, the patient is prescribed a special diet with limited water and salt load.
- If ascites occurs due to cancer, chemotherapy may be performed. Thanks to this, we achieve improvement in the condition of patients with ascites in advanced ovarian and colon cancer.
- Intracavitary chemotherapy is effective. After the fluid is removed, a chemotherapy drug is injected into the abdominal cavity. In approximately half of the cases, repeated evacuation of the fluid is not required for at least 2 months.
When a patient with cancer and ascites switches to complex therapy, laparocentesis is required 2–3 times less often than usual.
How does ascites manifest?
If there is a small amount of fluid in the abdominal cavity, this does not manifest itself in any way. In addition, this is normal: the human body produces and absorbs approximately 1.5 liters of fluid in the abdominal cavity per day. At the initial stage of ascites, patients have no special complaints, and the pathological condition can only be detected during an ultrasound examination.
When ascites progresses, a person feels heaviness in the abdomen and dull aching pain in the lower part. Subsequently, difficulty breathing, indigestion (nausea, belching, stool disorders) and urination problems occur. In the most severe forms, ascites significantly worsens health, discomfort appears in the abdomen, shortness of breath occurs, early satiety occurs, an umbilical hernia forms, and swelling of the lower extremities appears.
5–10 liters of fluid, and sometimes 20 liters, can accumulate in the abdominal cavity. Because of this, internal organs are strongly compressed, intra-abdominal pressure increases, and the diaphragm is pushed into the chest cavity. This entails severe difficulty breathing. Due to the fact that resistance to blood flow increases in the abdominal organs, heart failure occurs. The consequence of long-term ascites is a violation of the drainage of the lymphatic system. Because of this, there is also a violation of lymphatic drainage in the lower extremities and, as a result, their swelling. There may also be a backflow of lymph into the internal organs. As a result, cancer cells enter healthy organs from the affected lymph nodes. This can trigger the development of metastases in the liver, stomach, pancreas and other organs.
When there is more than one liter of fluid in the abdominal cavity, ascites can be noticed during a routine examination: the abdomen is enlarged or deformed, in an upright position it looks saggy, in a supine position the abdomen is flattened, the sides look swollen (the so-called “frog belly”). In thin patients, the navel often protrudes. A person may also experience hydrothorax, the presence of fluid in the pleural cavity. Typically, this condition develops in patients with congestive heart failure with long-standing ascites.
Mild or moderate ascites develops in 15 to 50 percent of patients in the early stages of cancer. In later stages, severe ascites occurs in 7 to 15 percent of patients.
In patients with advanced advanced cancer, exudative pleurisy is most common.
Book a consultation 24 hours a day
+7+7+78
What causes fluid to accumulate?
With ascites, a pathological accumulation of fluid occurs in the abdominal cavity. The fact is that in some diseases the regulation of water-salt metabolism and normal fluid circulation in the abdominal cavity are disrupted. The reason may be:
- Oncological diseases: secondary peritoneal carcinomatosis, lymphoma and leukemia, metastases in the hepatic portal area, primary mesothelioma.
- Diseases of the liver and its vessels: liver cancer, portal hypertension, liver cirrhosis, veno-occlusive disease, Budd-Chiari disease.
- Peritonitis (inflammation of the peritoneum) of various origins: pancreatic, fungal, parasitic, tuberculous.
- Congestive heart failure, constrictive pericarditis.
- Other diseases: ovarian tumors and cysts (Meigs syndrome), pancreatic cyst, Whipple's disease, sarcoidosis, systemic lupus erythematosus, myxedema.
Euroonco treats ascites of various origins. But since our main work is related to the treatment of malignant neoplasms, a significant part of our patients are cancer patients.
Classification and types of ascites
Classically, depending on the level of protein in ascitic fluid, ascites is divided into exudative (25 g/l or more) and transudative (<25 g/l). This allows us to indirectly judge the reasons. Currently, a more accurate indicator is used - the serum albumin-ascitic albumin gradient (SAAG):
- When SAAG is more than 1.1, the cause of ascites is usually pathologies such as cirrhosis, congestive heart failure, and Budd-Chiari disease. They are associated with increased pressure in the portal vein.
- If SAAG is less than 1.1, it can be assumed that the accumulation of fluid in the abdomen is caused by pancreatitis or cancer.
According to the clinical course, the following types of ascites are distinguished:
- Depending on the severity of the course: 1 degree. There are no clinical manifestations; the diagnosis is established by ultrasound (determining the level of free fluid in the abdominal cavity).
- 2nd degree. Slight visual enlargement of the abdomen.
- 3rd degree. Significant visual enlargement of the abdomen.
- Resistant to diuretics: treatment with diuretics in combination with a diet in which sodium chloride intake is limited to less than 2 g per day is ineffective (no effect after 1 week of therapy).
Diet
A very important goal is to restore nutritional status and normalize the level of proteins that were lost during the evacuation of the liquid mass.
Restriction of fluid and salt intake is required. It is necessary to exclude canned food, marinades and fast food from the patient’s diet, as they contain excess salt.
Insufficient protein levels are compensated by IVs and a selected diet. Patients with cancer need to consume protein at the rate of one and a half grams for every kilogram of weight.
How to treat ascites?
There are several main methods for treating ascites in patients with cancer:
- conservative therapy (aldosterone antagonists, diuretics) - aimed at normalizing water-salt metabolism and reducing the formation of fluid in the abdominal cavity;
- laparocentesis - puncture of the abdominal wall under ultrasound control; used not only for removing fluid, but also for installing drainage, which will serve for long-term removal of fluid;
- palliative surgical operations - peritoneovenous shunt, omentohepatophrenopexy, deperitonization of the abdominal walls and others.
Traditional methods of treating ascites caused by cancer do not have proven effectiveness and safety, therefore they are not used at Euroonko.
If you come to our clinic with ascites due to cancer, we recommend getting a second opinion regarding the treatment of the underlying disease from our clinical oncologists and chemotherapists.
Clinical case
A 59-year-old woman, Sh., was diagnosed with stage IV ovarian cancer (adenocarcinoma), ascites, and chronic pain syndrome 2 b according to the ShVO. The patient noticed an increase in the abdomen up to 120 cm in circumference, difficulty breathing, and weight loss. Specific treatment at the place of residence was denied. According to the patient, she was “sent home to die.” Read more…
A 59-year-old woman, Sh., was diagnosed with stage IV ovarian cancer (adenocarcinoma), ascites, and chronic pain syndrome 2 b according to the ShVO.
The patient noticed an increase in the abdomen up to 120 cm in circumference, difficulty breathing, and weight loss. Specific treatment at the place of residence was denied. According to the patient, she was “sent home to die.” Patient Sh. was urgently hospitalized in the specialized department of Euroonko, after active symptomatic therapy aimed at normalizing blood counts and restoring water and electrolyte balance, a peritoneal port was installed. Resolution of ascites was carried out under the control of plasma protein levels. The use of peritoneal ports allows for the removal of ascitic fluid in fractional doses, which ultimately eliminates the occurrence of serious complications in the form of hemorrhagic syndrome associated with hemodilution and coagulopathy as a result of massive entry of ascitic contents into the venous bed.
After stabilization of the general condition, against the background of nutritional support, antiemetic and antisecretory therapy, patient Sh. received specific chemotherapy treatment with good effect. Upon resolution of ascites in the presence of a peritoneal port, intra-abdominal chemotherapy became possible.
Six months after the described hospitalization, the patient returned to her usual lifestyle and continues to receive systemic treatment on an outpatient basis under the supervision of a team of Euroonco specialists. The response to treatment is regarded as positive in the absence of ascites and a total reduction in the size of the lesions by more than 70%. Combined treatment in the format of systemic and local (intra-abdominal) therapy with implantation of a port system is the optimal treatment regimen for this group of patients. In the practice of Euroonco doctors, such cases occur on a regular basis. Hide
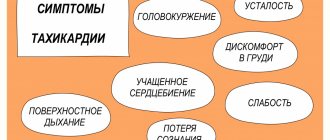
Symptoms
Symptomatic manifestations of the disease depend on three main factors - the cause, the volume of accumulated liquid mass, and the rate of accumulation.
Symptoms can appear at any time: sometimes it’s weeks and months, sometimes hours.
As we have already noted, one of the visual symptoms is an enlarged abdomen. Let's add weight gain here.
The patient may develop a feeling of bursting pain, flatulence, belching, heartburn, and nausea.
An increase in the volume of the abdomen entails the appearance of severe shortness of breath, swelling of the extremities, difficulty moving and bending.
Another number of symptoms that a patient may encounter are hemorrhoids, hernias, intestinal prolapse, and the development of varicocele.
Common symptoms of the disease include:
- Feverish state;
- Toxic state;
- Losing weight and at the same time growing belly;
- The saphenous veins of the abdomen are dilated;
- Blueness on the limbs.
What causes ascites to develop in cancer?
The most common cancers that cause fluid accumulation are:
- ovarian cancer (in 25–30 percent of patients),
- mammary cancer,
- uterine cancer,
- stomach cancer,
- colon cancer.
The accumulation of fluid in the abdominal cavity during cancer occurs due to the fact that the peritoneum (the membrane lining the inside of the abdominal wall and covering the organs located in it) is affected. Tumor cells settle on its parietal and visceral layers, resulting in disruption of lymphatic drainage. This causes deterioration in fluid absorption. Typically caused by tumors of the gastrointestinal tract and ascites in ovarian cancer.
When a tumor or metastases forms in the liver, the cause of ascites is different: the venous system of the liver is compressed and the natural venous outflow from the intestine is disrupted. This type of ascites develops quickly and usually lasts longer and is more severe. 15 percent of cases of fluid accumulation in the abdominal cavity due to cancer occur in this particular form.
Abdominal lymphoma causes ascites through blockage and effusion (leakage) of lymph from the intra-abdominal lymph ducts.
Features of the treatment of ascites in cancer patients
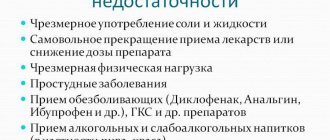
In hospitals that do not specialize in the treatment of cancer, the approach to patients with ascites may be ineffective due to the characteristics of this condition. For example, the main treatment may be the use of diuretics, aldosterone antagonists, and dietary changes to limit water and salt load. The effectiveness of this approach for reducing portal hypertension is relative; in cancer patients, ascites is caused by peritoneal carcinomatosis. Therefore, conservative therapy cannot be the main treatment method in such patients.
Typically, fluid is removed from the abdomen using laparocentesis (abdominal paracentesis). This is a surgical procedure that is performed by a surgeon and an anesthesiologist-resuscitator.
Conservative therapy
Conservative therapy is used in the treatment of small and moderate ascites. In other words, if there are no tiring and debilitating symptoms: pain, rapid breathing (tachypnea), etc. Up to 65% of patients have an improvement in their condition when treated with diuretics - this way you can remove up to 1 liter of fluid per day.
In the later stages of cancer, reducing salt and water intake can reduce quality of life. Therefore, at Euroonko such diet correction is rarely prescribed.
Book a consultation 24 hours a day
+7+7+78
Education
Excessive accumulation of liquid mass does not occur immediately, so human organs during this process adapt to changes in intraperitoneal pressure.
The international classification distinguishes three degrees of pathology:
- The first degree is characterized by a minimal volume of liquid mass, which is detected by ultrasound of the peritoneal cavity;
- Stage two - accumulation of liquid mass is determined by liters, the stomach increases;
- The third degree is called tense ascites, the person’s condition is assessed as serious.
As a rule, tense ascites is characterized by the accumulation of more than 10 liters of fluid in the peritoneal cavity.
Surgical treatment of ascites
Ascites in cancer must be treated surgically when it:
- Refractory, that is, ascites that cannot be treated conservatively.
- Large ascites, that is, if it is necessary to remove up to 6–10 liters of fluid at a time (this difficult procedure is carried out for strict medical reasons).
- Giant ascites. In this case, a combined operation is needed, which includes removing a large volume of fluid (up to 5–7 liters) on the first day and removing the remaining volume at a rate of no more than 1 liter per day for 7–10 days.
In the classic version, laparocentesis is performed on an empty bladder, the patient sits down, and the seriously ill person is placed on his side.
It is dangerous to perform laparocentesis without observing the rules of asepsis and antisepsis. Therefore, the release of fluid is carried out only in a specialized medical institution with a license to perform surgical interventions and with a hospital. If the patient is in serious condition, it is difficult for him to move, an ambulance team is called for him.
First, local anesthesia is performed, then, under ultrasound guidance, a puncture is made with a trocar (an instrument in the form of a thin tube with a sharp end) along the midline of the abdomen or along the line connecting the navel to the iliac crest. Usually no more than 5–6 liters of liquid are removed at a time. To prevent blood pressure from dropping sharply and vascular collapse, the fluid is released slowly.
In accordance with the classical technique, the patient needs to lie for several hours on the side free from the puncture. If at this time a small amount of liquid continues to be released, then a reservoir is applied, which is removed after a day or two.
If it is necessary to remove a large amount of liquid, then a loss of protein and salts occurs, which becomes the cause of protein deficiency. To prevent such a complication, the patient is given albumin. With repeated puncture, another complication may arise - fusion of the omentum (part of the peritoneum) or intestine with the anterior wall of the abdomen. Because of this, intestinal function deteriorates significantly, and during subsequent punctures serious complications can develop.
With the modern approach to laparocentesis, fluid drainage occurs primarily through a permanent peritoneal catheter. At the same time, the deficit in circulating blood volume is replaced by plasma expanders (from the English plasma expander - increasing plasma volume). Typically, 10–20% albumin solutions are used for this. In some cases, aminosteril, polyglucin, rheopolyglucin (dextran-40), hemacell and new starch-based preparations (refortan, stabizol, HAES-steril) can be used instead of albumin. This alternative only helps to compensate for fluid deficiency in the blood, but these drugs do not affect protein deficiency.
Some patients with ascites undergo omentohepatophrenopexy. This is a laparoscopic operation in which the omentum is sutured to areas of the surface of the liver and diaphragm. Due to the fact that contact occurs between the omentum and the liver, conditions appear for the absorption of ascitic fluid by nearby tissues. If the patient has peritoneal carcinomatosis, surgery is performed to a limited extent. Typically, in such patients, omentohepatophrenopexy becomes part of palliative treatment.
Dropsy: symptoms and treatment methods
Contents: [hide]
One of the dangerous consequences of malignant tumors of various organs in the human abdominal cavity and liver damage due to cirrhosis is ascites (dropsy). It is expressed in the accumulation of fluid in the abdominal cavity due to poor circulation in the portal vein. Ascites leads to a sharp increase in the volume of the human abdomen. Symptoms of dropsy depend on the type of disease and, in addition to ascites, can appear with some types of heart muscle defects, with kidney damage (rarely), and with other diseases. Dropsy (edema) may appear gradually over several months or appear suddenly.
Causes of dropsy
The main role in the occurrence of this disease and the accumulation of transudate is played by an imbalance between the inflow and outflow of fluid circulating through the tissues of the human body. Its breakthrough through the wall of the vessel into the surrounding organs and the accumulation of fluid in any place leads to the occurrence of edema or dropsy. By localization it is local or general in nature.
Due to its occurrence, the disease is caused by mechanical impact or pressure on a certain part of the body (organ). There is a sharp narrowing of the lumen in the veins in the affected area, but at the same time, deep-lying blood vessels and arteries continue to function normally, which prevents lymphatic fluid from leaving the narrowed veins in the required quantity. It gradually accumulates in the intercellular areas, and swelling appears.
If a person suffers from kidney failure or has scurvy, then the composition of the blood changes, the arteries are damaged and the nutrition of the body's cells is disrupted. Lymph penetrates along with liquefied blood components into the intercellular space and causes swelling. Such dropsy also manifests itself when the patient’s diet is unbalanced.
With disorders of the peripheral and central nervous system, another type of dropsy occurs. This occurs when spasms cause constriction of the veins due to paralysis, trauma and various damage to the nerve trunks, spinal cord and central nervous system.
Types of disease and its symptoms
The following types of dropsy are distinguished:
- swelling of subcutaneous structures;
- symptoms of heart failure;
- signs of disease in ovarian cancer in women;
- hydrocele in newborns and men;
- ascites in diseases of the abdominal organs or cirrhosis of the liver.
With the development of this disease, edema forms in the subcutaneous tissue. This can usually happen in those parts of the human body where the fiber structure is loose. With such swelling, the patient’s skin is dry and smooth to the touch, pale in appearance. Sometimes it shines in the affected areas, which helps to correctly diagnose the disease.
When the heart muscle is damaged, the skin takes on a blue or blue tint when swelling. Dropsy in such cases provokes a violation of venous circulation and its stagnation. At the first stage of the disease, swelling of the feet begins to appear, and then the dropsy moves to the patient’s ankles and begins to progress in the upper part of the body, especially in the patient’s abdominal cavity (ascites). Heart failure in this case is diagnosed when the patient has difficulty breathing and swelling of both legs.
The same phenomena occur in diseases of the stomach and liver, and ovarian cancer in women.
Another type of this disease is testicular hydrocele in men. It is divided into acquired type and congenital.
The main cause of such dropsy is acute inflammation of the testicles themselves or disruption of the cardiovascular system. During the development of the disease, the membranes of the testicles themselves thicken, which causes fluid accumulation.
Congenital dropsy and its symptoms appear during the formation of the fetus, when the testicles are still in its abdominal cavity. During this period, fluid accumulation may occur as the young testicle descends into the scrotum, which contributes to the development of hydrocele. With this development of the disease, two types are distinguished:
- isolated dropsy;
- its communicating appearance.
In the first case, part of the newborn's scrotum swells due to the penetration of fluid into the testicular cavity, from where it has no way out.
In most cases, this disease goes away on its own in children.
With communicating hydrocele, the fluid passes into the abdominal cavity and from it through the so-called processus vaginalis it flows to the testicles and causes a hydrocele, which is treated surgically. Such an intervention is performed when there is a significant increase in the size of the scrotum and an increase in swelling, leading to discomfort for the patient. If surgery is not performed during this period, the hydrocele becomes infected and a hernia may form in the man’s groin.
Dropsy of the abdomen (ascites) is easily determined due to the increase in its volume. In the supine (horizontal) position of the patient, the abdomen has a “frog” shape, and when the anterior abdominal wall is palpated, its fluctuation occurs. Difficulties appear when the patient bends his body. Other symptoms are also detected:
- swelling of the legs;
- shortness of breath when moving;
- change in skin color on the abdomen and others.
Ascites itself is divided into the following stages:
- Transient phase - the amount of liquid (up to 0.4 liters) is not determined visually. In this case, treatment can be carried out using a diet and maintaining the patient’s water and salt balance.
- Moderate type of disease - the patient has a soft stomach. It is treated by albumin infusion or the use of any diuretic. In some cases, it becomes necessary to puncture the abdominal cavity (laparocentesis) to remove fluid. If this method is abused, the patient develops the next phase of the disease, ascites, and develops renal failure.
- Resistant type of disease - the patient has more than 15 liters of fluid in the abdominal cavity. Treatment is carried out using the above method of laparocentesis, otherwise there will be a sharp increase in the patient’s weight and the volume of his abdominal cavity, which can lead to serious consequences for his health.
The disease causes flatulence and a feeling of pain and heaviness in the abdomen.
Treatment of dropsy with traditional methods
You can get rid of the disease in different ways and techniques:
- using traditional medicine recipes;
- traditional treatment in a hospital.
The most developed methods for treating ascites are traditional medicine. Here are some recipes:
- The husks of 14 bean pods are placed in 1 liter of water and boiled for 8-10 minutes. Then the broth is infused for 1/3 hour and filtered. They start taking the medicine at five o'clock in the morning - 0.2 liters, then drink the same amount before breakfast (30 minutes before meals), and half an hour before lunch take the same dose. The remaining portion can be taken in any amount, but no later than eight o’clock in the evening. If the symptoms of the disease do not go away within 3 days, then the medicine should be changed. During treatment, you should not drink other liquids.
- Take equal parts of dried bearberry leaves and hernia herb, chop and mix, place in a tightly sealed glass container. ½ cup of the mixture is poured into 0.2 liters of water and boiled for a quarter of an hour, and then filtered. You should drink on an empty stomach, 30 minutes before breakfast.
- A decoction is prepared from fresh apricots - pour 1 glass of fruit with a liter of water and boil for ¾ hours. You need to drink up to 0.4 liters per day, and the rest of the liquid is replaced with diuretics.
- Fresh parsley (0.3 kg) is boiled in a liter of water and the broth is filtered. Take half a glass every hour throughout the first half of the day. Treatment is carried out for three days.
For the treatment of other types of dropsy, traditional medicine offers the following recipes:
- Grind pumpkin and carrots on a fine grater, squeeze out the juice from the mixture and take half a glass per day.
- Pass the black radish through a meat grinder with a fine mesh, squeeze out the juice and mix with honey. Take the medicine gradually - drink 1/3 cup on the first day. Then, over the course of several days, increase the dose to two glasses.
- Cut 2 onions into small pieces and cover them with sugar, leaving the mixture until the morning. The juice released overnight is squeezed out using gauze and 2 tbsp. drink on an empty stomach.
Treatment of illness using modern medicine methods
Treatment of dropsy using modern medicine methods is carried out conservatively. For this purpose, painkillers are used, and a suspensor is prescribed for the patient to wear. Antibacterial drugs are also used. Chronic dropsy is treated using abdominal puncture, which can be performed by injection or surgically. The first method, in addition to removing fluid, also uses medications, formaldehyde and alcohol.
Dropsy, which is caused by testicular disease, is treated mainly by surgical methods using abdominal puncture. Ascites (dropsy, the symptoms of which is bloating of the abdominal cavity) can be eliminated by diet (in mild cases of the disease). Since this is usually not an independent disease, it is important to remove the causes of the underlying disease. It is treated surgically with abdominal puncture.
When prescribing a diet, fats in the patient’s diet are reduced, replacing animal types with vegetable ones. The intake of carbohydrates and liquids is also limited (no more than 1 liter per day). Food is steamed or boiled in water (added salt is not recommended). Foods included in the diet include cottage cheese, various cereals, fruits, vegetables, fish, and herbs.
Basically, everything is consumed in the form of jelly, casseroles, boiled and stewed. In case of kidney failure, cabbage, garlic, spinach, radish, sorrel, horseradish and various legumes are excluded from the diet. Dropsy, the causes of which are disorders in the spinal cord, is treated in a hospital setting using special medications.
Methods for diagnosing ascites
If more than 500 ml of fluid has accumulated in the abdomen, symptoms of ascites can be identified by a doctor during an examination. Ultrasound is used to confirm the diagnosis. Sometimes ascites is discovered accidentally during an ultrasound or computed tomography scan of the abdomen, which is performed for another reason.
Euroonco operates a comprehensive gastrointestinal screening program, which helps assess the condition of the digestive system. It, in particular, includes an ultrasound of the abdominal cavity with determination of the level of free fluid. This helps diagnose ascites at an early stage.
It is important not only to identify fluid in the abdominal cavity, but also to understand the reasons for its accumulation - this helps to assess the prognosis and prescribe effective treatment. In most cases, the examination includes the following laboratory tests:
- Biochemical blood test - complete biochemical panel. It helps assess the condition and function of the liver, kidneys, and electrolyte levels.
- Blood clotting study.
- Study of ascitic fluid obtained during laparocentesis. For analysis you need a little of it - usually 20 cm³, less than a tablespoon. It examines the level of red and white blood cells, total protein, albumin, amylase, glucose, and examines for pathogenic microorganisms. A cytological examination is performed to help identify cancer cells.
Possible complications of ascites
If a lot of fluid accumulates in the abdominal cavity, the functioning of the internal organs is disrupted, difficulties arise during breathing, as the mobility of the diaphragm is limited, and effusion forms in the pleural cavity.
With increased pressure in the portal vein, bacteria from the intestine can spontaneously penetrate the ascitic fluid and cause spontaneous bacterial peritonitis.
In rare cases, a very serious complication develops - hepatorenal syndrome. This term refers to impaired renal function with severe liver damage, up to severe renal failure. The exact mechanism of development of this condition is unknown, but it is believed to occur due to impaired renal blood flow, excessive use of diuretics and intravenous contrast agents.
Risk factors
The main risk factor is a malignant tumor. The peritoneum itself looks like a sheet covered with a mucous membrane and is an ideal place for the development of metastases.
They penetrate there through the blood vessels, breaking away from the tumor focus, and force the serosa to reproduce excess liquid mass.
In addition, in the lymph vessels, atypical cells grow and block them, thereby disrupting the absorption of the liquid mass.
Factors that contribute to the accumulation of excess fluid mass in oncology are:
- Cirrhosis;
- Liver dysfunction as a result of a chronic disease or toxic hepatitis;
- Heart disease that slows blood flow;
- Failure of kidney excretory function as a result of chemotherapy;
- Increased thrombus formation in the vessels of the peritoneal cavity;
- Changes in the protein composition of the blood as a consequence of gastrointestinal carcinoma.
Forecast
Ascites in cancer significantly worsens the prognosis. From the moment of diagnosis, only half of the patients remain alive within 1–4 months. The average life expectancy is from 20 to 58 weeks. Timely treatment in a clinic that specializes in working with such patients helps improve survival. With ascites caused by liver cirrhosis, when there is no cancer, the prognosis is better. And a patient whose accumulation of fluid in the abdominal cavity was caused by chronic heart failure, with appropriate treatment, can live for many more years.
Contraindications
Almost all contraindications for laparocentesis are relative. With the necessary preparation with the correction of the patient’s complications or compliance with conditions taking them into account, the procedure can be performed.
Such contraindications include:
- decreased platelet level (less than 20 × 103 / μl) (can be corrected by platelet transfusion before laparocentesis);
- bleeding disorders (corrected by infusions of fresh frozen plasma);
- adhesions in the abdominal cavity;
- cellulitis of the anterior abdominal wall;
- intestines dilated due to accumulation of gases;
- full bladder;
- pregnancy.
An absolute contraindication for laparocentesis is only an acute abdomen, which requires emergency surgery.