What is PV and where is it located?
The subclavian vein is located in front of the scalene muscle and receives the veins of the arm and neck. It serves as a continuation of the axillary vein, which receives blood from the arm belt and free upper limb.
The anatomy of the vessel is as follows: it has valves that are located from the lateral edge of the 1st rib to the sternoclavicular joint. The subclavian vein forms a venous angle due to its connection with the internal jugular vein.
The brachiocephalic veins are formed due to the confluence of the subclavian and internal jugular veins. The subclavian vein is separated from the artery of the same name by the anterior scalene muscle.
Subclavian vein tributary
The venous wall is fused with the fascia of the neck, the periosteum of the 1st rib and the tendon. It is for this reason that the lumen of the vein does not collapse. This factor plays an important role, because when a vein is injured, there is a high probability of developing an air embolism.
The tributaries of the subclavian vein are:
- the dorsal scapular vein corresponds to the basin of the artery of the same name;
- sternal veins, which carry blood from the pectoral muscles.
On the right side of the neck, the Pirogov venous angle is located in front of the subclavian vein, into which the jugular vein flows.
Functions
The main function of the vein is considered to be the outflow of blood saturated with carbon dioxide and metabolic products.
In addition, thanks to it, hormones from the endocrine glands and nutrients that are absorbed in the gastrointestinal tract penetrate into the bloodstream.
The subclavian vein occupies an important place in the regulation of general and local blood circulation, as well as in the spread of various inflammatory processes occurring in the human body.
What diseases are associated with PV?
The circulatory system is considered a complex structure, which plays the role of transferring blood from other channels.
One of the common diseases of the subclavian vein is thrombosis, in which the blood flow along the entire upper limb changes significantly. The reason for the development of this disease lies in blood clotting disorders and excessive physical stress on the body.
Mostly the pathology is diagnosed in young patients and predominantly in men.
With timely diagnosis and effective therapy, the prognosis is quite favorable.
With high physical stress on the body, one arm becomes overstrained, which leads to compression of the veins. The result of this is thrombosis, and this is facilitated by increased blood clotting and too slow blood flow.
A common developmental anomaly of the subclavian arteries is the aberrant right subclavian artery. As a result of compression of the aberrant subclavian artery of the underlying structures, symptoms may appear that directly depend on the patient’s age and anatomical features of development.
Tests and diagnostic methods
To make an accurate diagnosis of vein damage, a specialist carefully studies the patient’s medical history. The doctor clarifies with the patient all the signs that bother the patient. The collected information allows us to clarify the duration of thrombosis.
In order to identify venous pathology in acute or chronic form, the following diagnostic methods are usually used:
- MRI and radiography help not only to identify the cause of the disease, but also the location of the thrombus;
- Ultrasound examination of deep veins;
- Dopplerography, which evaluates blood circulation in the damaged vein;
- X-ray using a contrast agent;
- duplex scanning of a vein;
- venography;
- shoulder girdle.
If puncture is necessary, subclavian access is preferably used.
Complications
The most common complication is the phenomenon of vertebral-subclavian steal (steal syndrome). To compensate for blood circulation in the arm, cerebral blood flow is used, which moves in the opposite direction from the brain to the arm through the vertebral artery. In this case, physical work with the hand can cause disruption of cerebral circulation, including loss of consciousness.
Occasionally, atheroembolic complications may occur. Pieces of atherosclerotic plaque may be carried downstream into the arm. This is manifested by a sharp deterioration in blood circulation in the hand, blueness and pain in the fingers. If help is not given in a timely manner, necrosis of the finger may develop, which will require its amputation.
Symptoms of PV pathologies
The main cause of subclavian vein thrombosis is considered to be high physical stress on the body. It is this factor that plays the leading role in the formation of a blood clot. Sometimes it is possible for a blood clot to break off, regardless of the degree of physical stress on the body, but this is extremely rare.
With thrombus formation in the subclavian vein, both increasing and disappearing symptoms may be observed, manifested by certain influxes.
As a result of injury to the subclavian vein, certain symptoms are noted:
- pronounced pain in the arm area;
- too bright pattern of veins, visible through the epidermis;
- severe swelling of the limb and the appearance of a glossy sheen on the skin.
When the subclavian vein is injured, the patient exhibits signs of a neurological disorder. They manifest themselves in the form of numbness of the limbs and their twitching.
Often patients do not notice the appearance of a venous pattern on the arm. The diameter of the veins is determined by the size and increase in hypertension of the thrombus.
Initially, pain occurs during physical exertion on the body. Over time, discomfort can be constant and a feeling of fullness appears.
The pain syndrome is felt throughout the entire surface of the arm, in the shoulder area and collarbone. Sometimes it can radiate to the upper back and chest.
With thrombosis, the entire arm is affected by edema. When pressing on the swollen area, the hole in this area is not preserved. The hand becomes too hard and the unusual heaviness bothers you. With a prolonged inflammatory process, problems with blood circulation are noted, and the manifestations of thrombosis noticeably increase.
The patient may experience twitching of the fingers, a tingling sensation and a slight burning sensation.
During the transition of a patient's thrombosis from an acute to a chronic form, the clinical picture is blurred, and it becomes less pronounced. With this pathology, the patient’s motor activity is limited, muscle atrophy develops, and pain occurs with increased physical activity.
Sometimes, with a disease such as subclavian vein thrombosis, the patient is given a disability.
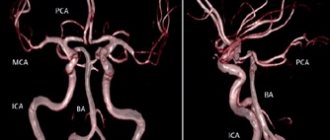
Surgical interventions on the subclavian artery and brachiocephalic trunk
When the brachiocephalic trunk or subclavian artery is blocked in the area before the origin of the vertebral artery, retrograde blood circulation occurs behind the blockage, through the vertebral and also through the right carotid artery. Thus, in this situation, the just named vessels do not improve blood supply to the brain, but, on the contrary, “rob” it. Conform syndrome occurs. With functional load on the upper limbs, their need for blood flow increases, the outflow through the arteries of the upper limbs, vertebral arteries and the right carotid artery, which function as collaterals, increases, which further impoverishes the blood supply to the brain and aggravates ischemic symptoms.
There are many reasons for the phenomenon of “robbery”. Among the most common, as well as more clinically important, the following are known:
a) “stealing” from the left vertebral artery when the left subclavian artery is blocked;
b) general “stealing” of the right carotid artery and vertebral arteries during blockage of the brachiocephalic trunk; part of the blood drawn by the vertebral arteries can return through the right carotid artery back to the substance of the brain (“carotid return phenomenon”);
c) “stealing” the right vertebral artery when the right subclavian artery is blocked.
The subclavian artery, with an adjacent blockage, is characterized by a “stealing” symptom, going in two directions and giving a combined disorder of blood circulation to the brain and upper limb. This phenomenon is interesting because the withdrawal of blood (“stealing”) through the vertebral artery is accompanied by more severe symptoms than when this artery is blocked.
Indications for surgery for steal syndrome are primarily symptoms from the central nervous system. The blood supply to the upper extremities in most cases has enough time to compensate for the slow progression of the occlusion process due to the good development of the collateral network.
Operations for recanalization of the subclavian artery are indicated if
a) there are pronounced symptoms of disorders of the central nervous system;
b) ischemic symptoms develop in the upper limb when performing even minor work;
c) there is a combination of symptoms from the central nervous system and the upper limb.
In older patients with poor general condition, to reduce the onset of cerebral circulatory disorders, a simple ligation of the vertebral artery that interferes with blood circulation can be performed.
Isolation of the left subclavian artery
The middle part of the subclavian artery can be isolated on both sides from the supraclavicular approach. This access is convenient for applying a bypass shunt. It is very difficult to perform an endarterectomy from it. In addition, if necessary, the surgical field cannot be expanded from this access.
The incision is made transversely above and parallel to the clavicle, from the posterior edge of the sternocleidomastoid muscle to the anterior edge of the trapezius muscle. The patient's scapula is retracted upward, which creates, due to the elevation of the clavicle, a more convenient approach to the subclavian artery. Under the platysma, at the lower edge of the wound, the external jugular vein, which flows into the subclavian vein, intersects between the ligatures. Excretion in fatty tissue, rich in small vessels and nerves, is quite difficult. The scapulohyoid muscle is retracted upward and outward, after which it is possible to navigate the deeper tissues. By palpating, the attachment site of the anterior scalene muscle and the first rib are determined, and the brachial plexus is found. In a triangle, the sides of which are the named anatomical formations, the subclavian artery passes between the subclavian vein and the brachial plexus. If there is a need for this, the clavicle is intersected, which allows for somewhat expanded access.
The peripheral part of the subclavian artery can be reached from the subclavian approach. For this part of the artery, the subclavian approach is more appropriate than the supraclavicular approach. With the subclavian approach, a large number of thin nerve branches are spared, which are often accidentally damaged, resulting in very unpleasant postoperative complications. After dissecting the skin and subcutaneous tissue, the pectoralis major muscle is easily separated along its fibers. After disconnecting the pectoralis minor muscle, you can easily find the neurovascular bundle in the fatty tissue. Its isolation is facilitated by raising and abducting the shoulder upward and anteriorly.
The initial part (orifice) of the subclavian artery on the left side is most easily reached through an anterolateral thoracotomy in the 1st II-IV intercostal space. To ensure good dilation of the thoracotomy wound, a roller is placed under the chest of the patient lying on the right side of the body, and the upper part of the operating table is raised. A large incision should be made, since it will be difficult to understand and act from a small incision in the “deep well” of the surgical wound. It is not difficult to navigate in the chest cavity to find the necessary vessel. The last major branch of the aortic arch is the left subclavian artery. It is placed on a holder after dissection of the mediastinal pleura and adventitia. This technique protects against possible damage to the clearly visible trunk of the vagus nerve and its posterior branch, the recurrent nerve.
Isolation of the initial part of the brachiocephalic trunk and the right subclavian artery
The ascending aorta is isolated from the median sternotomy. Its branch going upward, to the right and anteriorly is the brachiocephalic trunk.
Access to this vessel is crossed by one single formation located in loose fatty tissue (remnants of the thymus gland) - the left brachiocephalic (innominate) vein passing here. This vein should be isolated, if possible, atraumatically, over a wide area. It is taken on a rubber holder and easily moved to the side. The brachiocephalic trunk is found by its branching into the right carotid and subclavian arteries. During the isolation of the subclavian artery, it is necessary to remember the vagus nerve passing close here, going back behind the vessel of the branch of the recurrent nerve.
If access is intended to be continued to the carotid or subclavian arteries, then the incision is extended along the anterior edge of the sternocleidomastoid muscle or in the transverse direction above the clavicle.
Isolation of the vertebral artery
The incision is made parallel to and above the clavicle in the same way as when accessing the middle part of the subclavian artery. Then the external jugular vein is crossed between the ligatures. If necessary, the sternocleidomastoid muscle can be incised. After this, the medial edge of the anterior scalene muscle is sought, along which the vertebral artery rises upward. When using a left-sided approach, care must be taken not to damage the thoracic duct. In addition, you should also be careful about the phrenic nerve running along the anterior scalene muscle. In the adjacent segment of the subclavian artery there are the orifices of the vertebral artery, the cervical-thyroid trunk and the internal thoracic artery.
The vertebral artery passes in the direction of the transverse process of the 6th cervical vertebra, converging medially, posteriorly and upward. It has no branches in this area!
Surgical interventions on the left subclavian artery
Stenosis or occlusion of the subclavian artery and brachiocephalic trunk, as a rule, is localized over a short distance of the initial (central) segment of these vessels.
First of all, they try to perform an endarterectomy. For this purpose, from the left-sided anterolateral thoracotomy, according to the method described above, these vessels are approached, isolated and taken onto a tourniquet. The opening of these vessels in the aortic region is isolated along with the corresponding section of the aortic arch so that a small section of the aortic wall can be squeezed out. At the same time, select the desired vascular clamp and apply it provisionally. The first branches of the subclavian artery, the internal mammary artery, the thyroid-cervical trunk and the vertebral artery are isolated and taken onto a tourniquet.
After applying a wall clamp to the aortic arch in the area of the mouth of the operated vessel, an arteriotomy is performed, moving slightly onto the aortic wall. An endarterectomy is performed in the layer required for this and, when indicated, the exfoliated distal part of the intima is fixed. The arteriotomy hole is closed with a continuous suture if possible, and only in the case of possible narrowing of the lumen of the vessel is plastic surgery with a synthetic patch applied. An important point is to remove all air from the recanalized vessel, since entry of air bubbles through the vertebral artery can cause cerebral embolism. Therefore, removal of the clamps from the vertebral artery is done last, after blood circulation in the vessels of the upper limb has been restored within 2-3 minutes. In cases where endarterectomy cannot be performed, a shunt is placed between the aorta and the subclavian artery from the same access. The prosthesis is sewn in at the border between the aortic arch and its descending part.
The literature on vascular surgery repeatedly describes a shunt between the carotid and subclavian arteries, but we do not recommend this operation. Surgical intervention involves placing a shunt between the common carotid artery and the subclavian artery from a small supraclavicular approach. If this operation is unsuccessful, it leads to the destruction of both of these vessels, leading to severe disorders due to a disorder of the blood flow of the carotid artery.
Surgical interventions on the brachiocephalic trunk and right subclavian artery
Difficulties and possible complications during this intervention on the brachiocephalic trunk and the right subclavian artery are associated with the fact that the common carotid artery departs from the brachiocephalic trunk. In some cases, during operations to maintain blood circulation in the carotid artery, it is necessary to use a shunt inserted into the lumen of the vessel. Access for surgery in this area is through a median sternotomy.
Due to the possible different localization of occlusion or stenosis, the following intervention methods are possible.
1. When the brachiocephalic trunk is occluded, this vessel is switched off by applying a clamp; the blood supply to the carotid artery is provided by reverse blood flow from the subclavian artery. The course of the operation is as follows: longitudinal arteriotomy, endarterectomy, closing the arteriotomy opening with a continuous suture, removing air from the lumen of the vessel. This particularly important measure, aimed at preventing the occurrence of embolism, is ensured by the sequential removal of the clamps and the gradual inclusion of branches in the blood circulation. The last, after 1-2 minutes, are the carotid and vertebral arteries.
2. In case of occlusion of the initial section of the subclavian artery with the transition of the atherosclerotic thrombus to the brachiocephalic trunk, the following intervention is performed. The brachiocephalic trunk, carotid and subclavian arteries are clamped. An arteriotomy is performed, extending to the brachiocephalic trunk and subclavian artery. Then a shunt is placed into the lumen of the brachiocephalic trunk and from it into the common carotid artery. After insertion of the shunt, you can safely, without fear of cerebral hypoxia, perform an endarterectomy. The arteriotomy hole is closed according to the method described above.
3. Closure of the initial section of the subclavian artery can be significantly complicated by narrowing of the mouth of the carotid artery by atherosclerotic plaque. With this double vascular lesion, a Y-shaped arteriotomy is performed through the mouths of the carotid and subclavian arteries and partially involving the brachiocephalic trunk. Since the length of the blockage is usually small, an endarterectomy is performed on the subclavian artery under the protection of a shunt inserted into the lumen of the vessel. A patch is applied to the arteriotomy hole at the end of the operation, which avoids narrowing of the lumen of these vessels.
4. When there is occlusion of only one subclavian artery, the operation is much simpler, since there is no need to insert a shunt into the lumen of the vessel. If access to the vessel is difficult, then the edge of the sternocleidomastoid and sternothyroid muscles is incised. After this, endarterectomy is performed according to all the rules.
If endarterectomy is not feasible, a bypass graft is performed. When closing the brachiocephalic trunk or subclavian artery, an aorto-subclavian shunt is applied. For this purpose, the wall of the ascending aorta is pressed out, and an end-to-side anastomosis is applied from a synthetic prosthesis.
Then an anastomosis is performed on the peripheral part of the subclavian artery. For this purpose, an incision is made under the collarbone, the peripheral part of the subclavian artery is isolated, and a tunnel for the graft is made behind the collarbone with a finger. The second anastomosis with the subclavian artery is performed in an “end to side” fashion.
What doctors treat
A phlebologist treats vein pathologies, including the subclavian vein. It is he who can explain to the patient in detail what the subclavian vein is, its importance for the functioning of the whole body and possible pathologies.
If the blood vessels are not significantly clogged, the problem can be dealt with using local treatment. It is necessary that the hand is at rest.
When in a horizontal position, the upper limb should be positioned slightly above the heart area. While the patient is in an upright position, you need to suspend your arm using a scarf or bandage, bending it slightly at the elbow.
Seldinger catheter insertion
Immediately after puncture of the vein, make sure that the blood flows easily into the syringe. Disconnect the syringe while holding the needle in place. Try to rest your hand on the patient’s body to minimize the risk of needle migration from the lumen of the vein. Close the needle pavilion with your finger to prevent air from entering;
Insert the flexible end of the guidewire into the needle. If there is any resistance to the conductor's advancement, carefully turn it and try to advance it. If this does not help, remove the metal conductor. Assess blood aspiration from the vein again. Change the angle of the needle or rotate it, check the flow of blood into the syringe. Try again. If it was not possible to insert a plastic conductor, in order to avoid cutting, it must be removed along with the needle.
After inserting the guidewire halfway into the vein, remove the needle. Before inserting the dilator, incise the skin with a scalpel with a small blade; Insert a dilator through the guidewire. Try to take the dilator with your fingers closer to the skin to avoid bending the conductor and additional trauma to the tissue, or even the vein. There is no need to insert the dilator over its entire length; it is enough to create a tunnel in the skin and subcutaneous tissue without penetrating the lumen of the vein. Remove the dilator and insert the catheter. Remove the conductor. Perform an aspiration test. Free blood flow indicates that the catheter is in the lumen of the vein.
Therapy methods
Local therapy for damage to the subclavian vein can be carried out using certain groups of medications:
- gel-like products that contain rutoside and troxevasin;
- ointments with heparin;
- alcohol-based compresses;
- non-steroidal anti-inflammatory medications.
In case of acute thrombosis of the subclavian vein and the appearance of painful symptoms, the patient is admitted to the hospital. The course of therapy includes the use of:
- angioprotectors;
- anticoagulants;
- antiplatelet agents;
- fibrinolytic agents.
The main goal of drug therapy for subclavian vein thrombosis is to restore normal blood circulation.
When is surgery required?
If after 2 months the blood clot has not resolved, then surgery is prescribed.
If thrombosis of the subclavian vein is too long, there is a high risk of necrosis of the arm tissue. During the operation, a specialist removes tissue that has died.
If blood circulation through the veins is impaired and there is a chronic form of thrombosis of the subclavian vein, thrombectomy or recanalization may be performed. If it is impossible to carry out this type of operation, they resort to eliminating the damaged section of the main vein, performing plastic surgery and bypass surgery.
In a situation where the pathology is completely untreatable, the arm is amputated.
Puncture and catheterization of the subclavian vein is performed by a surgeon or anesthesiologist. Sometimes these procedures can be performed by a specially trained therapist.
Indications for catheterization are inaccessibility of peripheral veins, too long operations with loss of large amounts of blood and the need for parenteral nutrition.
In case of injuries and bleeding, taking into account the topography of the subclavian vein, it is necessary to ligate it or apply a special bandage from three zones: under, above and behind the collarbone. The patient is placed on his back, a cushion is placed under his shoulders and his head is turned in the direction opposite to where the operation is being performed.
Puncture of the right femoral vein
Position the patient on his back, with a cushion placed under the buttocks. The leg should be slightly abducted and turned outward. Determine the pulsation of the femoral artery below the inguinal ligament: the femoral vein is located more medially. Treat the skin with an antiseptic and limit the puncture site with sterile wipes. Next, infiltrate the skin and subcutaneous tissue with 5 ml of a 1% lidocaine solution. Incise the skin with a scalpel with a small blade.
2 cm below the inguinal ligament, determine the course of the femoral artery with two fingers of your left hand. The needle is inserted 1 cm medial to the femoral artery at an angle of 30° to the skin and directed along the vein, maintaining a vacuum in the syringe until blood is obtained. The vein is usually located at a depth of 2-4 cm from the surface of the skin. It is convenient to use a G14-16 peripheral venous catheter as a needle, after making sure that it passes the conductor.
If you do not find a vein, slowly remove the needle while maintaining a vacuum in the syringe. Rinse the needle and make sure it is clear. Try again, aiming the needle slightly to the right or left of the original puncture site.
The role of PV in the diagnosis and treatment of diseases
Thrombosis of the subclavian vein is considered a pathology that almost every person can encounter. It is possible to prevent the development of such a disease by excluding factors that influence thrombus formation.
The risk of damage to the subclavian vein is quite high with an abscess, which must be eliminated as soon as possible. In all other situations, it is almost impossible to avoid the development of pathology.
The role of PV in the treatment and diagnosis of diseases of various nature is high.
This blood vessel is mainly used for infusion therapy for cancer, in intensive care units, and intensive care units.
Causes and risk factors
The reasons for the development of atherosclerosis of the subclavian artery are the same as for other atherosclerotic plaques. Most often these are high cholesterol, diabetes, obesity, and smoking. Lesions most often occur in the initial section (proximally) of the subclavian artery, but can also occur in other segments. Damage to the subclavian artery may be associated with compression between the first rib and the clavicle (compression syndrome at the thoracic outlet). Proximal lesions of the subclavian artery can be insidious and are detected by measuring blood pressure on different arms or pulsations. However, complications related to blood circulation in the arm or brain often develop.