A separate area on my leg hurts. The skin is thick, hot, marble-white. Suddenly there was a high fever, weakness and severe swelling of the leg. Accompanied by cold-like symptoms, but antibiotics do not help...
Phlebitis is an inflammation of the walls of a vessel, which leads to the gradual destruction of the vessel completely. The danger of the disease lies in complications due to the patient’s lack of desire to seek medical help.
The appearance of blood clots (thrombophlebitis), blockage of veins, thrombosis, abscess - these are the consequences of lack of treatment. To avoid them, listen carefully to your own body. He will definitely indicate the first signs of the disease. A qualified specialist, a phlebologist, will help determine the disease.
It is important to see a doctor at the first symptoms. Timely help will help you get rid of phlebitis, possible complications and causes of the disease almost without a trace. Let's figure out how to recognize and treat phlebitis in time.
What it is?
Phlebitis
is an inflammatory disease of the walls of venous vessels, which can occur in acute or chronic form. The acute form is characterized by severe pain in the affected veins, fever and general weakness. With chronic phlebitis, the disease is asymptomatic for a long time and appears only during exacerbations. Inflammation can occur in the veins of the legs, arms, and other parts of the body, but phlebitis of the lower extremities is most common. A serious complication of this disease can subsequently be thrombophlebitis (inflammation with the formation of a blood clot).
Prevention of phlebitis during pregnancy
During pregnancy, every woman may experience phlebitis, especially if she was previously diagnosed with varicose veins of the lower extremities. During pregnancy, most drugs used to treat phlebitis are strictly contraindicated. Therefore, it is necessary to take all measures to help prevent such vascular disease. Throughout the entire period of bearing a baby, it is useful to follow these simple recommendations:
- take daily walks in the fresh air;
- regularly do exercises that have a general strengthening effect;
- control weight;
- Healthy food;
- If you have suspicious symptoms, consult a doctor rather than wait for the situation to resolve on its own.
Types of phlebitis
Phlebitis can be divided into three groups (depending on the location of the inflammatory process):
- Endophlebitis – inflammation of the inner lining of the vein wall occurs
- Periphlebitis - the outer lining of the vein becomes inflamed
- Panphlebitis is an inflammatory process that affects all the membranes of the venous wall.
Based on the reasons for the development and localization of inflammation in the body, phlebitis is classified into:
- Post-injection - develops as a result of chemical irritation of the veins after the administration of a drug, blood sampling, etc.;
- Migratory - phlebitis with a chronic form, manifested by periodic inflammation of the venous walls, difficult to diagnose;
- Painful – more common in women after childbirth, characterized by acute intense pain;
- Cerebral - with this form of the disease, the blood vessels of the brain are affected, provoked by infections;
- Allergic – occurs as a result of exposure to allergens, has a chronic course;
- Pylephlebitis is an inflammation of the portal vein (occurs with complications in the abdominal cavity).
Diet
If you have phlebitis, you need to radically reconsider your eating habits and give up foods containing large amounts of salt, animal fats, preservatives and other chemical additives. It is advisable to eat often, but little by little. Prepare dishes using gentle methods: steamed, oven, grilled, or simply boiled in water. Diet for thrombophlebitis For thrombophlebitis, the diet should consist of the following food groups:
- fish, seafood;
- lean meat;
- cereals: buckwheat, rice, oatmeal;
- fresh vegetables, fruits, berries, herbs;
- dairy and fermented milk products;
- freshly squeezed juices, fruit drinks;
- dried fruits, seeds, nuts.
The main causes of phlebitis
The main reason for the development of phlebitis of the lower extremities is varicose veins. This is one of the most common causes of phlebitis. Also, this disease can occur as a result of infection (the causative agents of which are streptococci), mechanical damage to venous vessels (intravenous injection or infusion (infusion), blood sampling), chemical burns after injections. Other causes of phlebitis include: excessive weight of the patient; prolonged immobility or tightness of the limb; bruises and injuries; complications after childbirth, etc.
How to treat
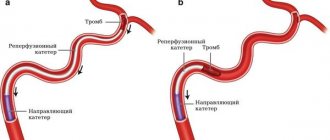
To treat thrombophlebitis, modern medicine uses various methods, from drug therapy to surgical intervention, depending on the severity of the disease and its stage. Most patients are usually prescribed conservative therapy, the goal of which is to stop the inflammatory process and reduce the risk of vascular thrombosis. For this purpose, the doctor prescribes:
- anti-inflammatory non-steroidal drugs;
- anticoagulant medications;
- enzyme therapy;
- treatment with phlebotonics;
- local compresses and ointments;
- in the presence of a purulent process - antibiotic therapy.
The patient is prescribed bed rest, but he can be treated at home if there is no risk of complications. Mechanical support of the blood vessels is important: it is necessary to bandage the affected limb with an elastic bandage and/or wear special compression garments. If there is a risk of disease progression and transition to deep veins, surgical removal of the thrombosed vessel is prescribed.
Symptoms of phlebitis of the veins of the upper and lower extremities
Symptoms of phlebitis are quite varied and depend on the form and type of disease.
The following symptoms are characteristic of acute and chronic phlebitis of the superficial veins:
- the vein becomes tense and very painful;
- there is redness and thickening of the skin, local hyperthermia (increased temperature of a given area of the body);
- the appearance of red stripes along the location of the venous vessel.
Acute and chronic phlebitis of the deep veins are accompanied by:
- pain and swelling in the area of inflammation;
- increased temperature of the whole body (general hyperthermia);
- the skin takes on a milky white hue.
With cerebral phlebitis the following occurs:
- headache;
- blood pressure increases;
- neurological symptoms.
A characteristic symptom of pylephlebitis
is severe purulent intoxication.
Symptoms of the disease and the patient’s feelings
Phlebitis usually manifests itself within 24 hours after intravenous administration of the drug. The patient experiences redness at the site of the catheter or injection. It is removed with a catheter. However, the inflammatory process may continue to worsen and be accompanied by the following symptoms:
- due to the accumulation of blood at the injection site, the veins thicken and protrude outward;
- soft tissues thicken, which becomes noticeable upon palpation;
- severe pain occurs that radiates to the fingers;
- the hand swells (and several hours after the injection), severe swelling appears;
- blue discoloration of the affected area;
- The elbow and axillary lymph nodes are noticeably enlarged.
The patient's condition continues to deteriorate, the body temperature rises, and on the 3-4th day the limb stops bending and straightening at the elbow joint. If treatment is not started, the pathology will begin to spread to the adjacent vessel. Suppuration of the venous walls is also possible.
Diagnostic methods
- Examination of affected veins by a specialist
- Blood tests
- Duplex/triplex angioscanning of the veins of the lower extremities
- Duplex/triplex angioscanning of arteries and veins of the upper extremities
- Ultrasound Dopplerography of veins (USDG).
Specialists to contact (depending on symptoms):
- Phlebologist consultation
- Cardiologist
- Surgeon
- Traumatologist-orthopedist
- Therapist
To establish a diagnosis and prescribe immediate treatment, we invite you to contact specialists from the Central Clinical Hospital of the Russian Academy of Sciences in Moscow.
How to prevent further development of the disease
Measures to prevent thrombophlebitis are equally effective both for those who have already suffered from an acute form of the disease and for people who are at risk of developing inflammation of the veins. These include:
- constantly wearing compression hosiery or supporting veins with elastic bandaging;
- proper organization of work and rest;
- moderate physical activity on the legs, providing support for the function of venous valves and preventing the progression of varicose veins;
- following a special diet;
- providing regular unloading for the legs in the form of a lying position with the legs raised above the body.
If these rules are followed, the risk of thrombophlebitis is significantly reduced.
Treatment
Phlebitis in most cases is subject to complex treatment using conservative methods. Outpatient treatment is possible, and if the disease is severe, the patient must be hospitalized. For certain indications, surgical intervention is prescribed.
Treatment includes:
- Drug therapy (painkillers, antiviral drugs, antibiotics, anti-inflammatory drugs, blood thinners, etc.)
- Physiotherapeutic procedures
- Wearing compression garments
- Prevention of disease.
Prevention of complications
Many cytostatics damage veins, the aggressive cisplatin, anthracyclines and vinca alkaloids, as well as the relatively “mild” gemcitabine with fluorouracil, are especially zealous in initiating chemical phlebitis. Based on their effect on tissue, anthracyclines with vinca alkaloids are classified as blister agents, cisplatin is only an irritant, and gemcitabine is definitely not a blister agent. Nevertheless, any chemotherapy drug, and even more so a combination of cytostatics, can damage a vein, therefore, during intravenous administration, personnel must strictly follow the instructions for the duration and method of injection.
Physiotherapeutic procedures and acupuncture, phototherapy and infrared irradiation, and magnetic field stimulation help recovery.
In our Clinic, each patient undergoes a specific program of support for chemotherapy and recovery after treatment, focused on the characteristics of the body and tissue resistance.
Book a consultation 24 hours a day
+7+7+78
Bibliography:
- Russian clinical guidelines for the prevention and treatment of venous thromboembolic complications in cancer patients // M.: Planida; 2012
- Somonova O.V., Antukh E.A., Elizarova A.L., et al. /Practical recommendations for the prevention and treatment of thromboembolic complications in cancer patients // Malignant tumors: Practical recommendations RUSSCO #3s2; 2017 (vol. 7).
- Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines // Chest Am Coll Chest Phys.; 2012.
- Jones S., Holmes F., O'Shaughnessey J., et al. /Docetaxel with cyclophosphamide is associated with an overall survival benefit compared with doxorubicin and cyclophosphamide: 7-year follow-up of US Oncology Research trial 9735// JCO 2009; 27.
- International Society of Lymphology. The diagnosis and treatment of peripheral lymphedema: 2013 Consensus Document of the International Society of Lymphology // Lymphology; Mar 2013; 46(1).
- Khorana AA, Kuderer NM, Culakova E., et al./ Development and validation of a predictive model for chemotherapy-associated thrombosis// Blood 2008; 15.
Risk factors for the development of thrombophlebitis
- pregnancy, childbirth, gynecological operations (including abortions).
- varicose veins;
- prolonged bed rest (for example, after surgical and orthopedic operations);
- infectious diseases;
- stroke leading to paralysis of the limbs;
- motionless body position during a long trip by car or plane;
- obesity;
- oncological diseases (including surgical treatment of malignant neoplasms, radiation therapy and chemotherapy);
- dehydration;
- the use of hormonal contraceptives and other sex hormone preparations for the purpose of replacement therapy;
- increased blood clotting (hyperhomocysteinemia, antiphospholipid syndrome, etc.);
- puncture and/or venous catheterization.
The more risk factors a patient has, the higher the risk of developing thrombophlebitis.
If you have one or more factors from the above list, consult a specialist about methods of preventing venous thrombosis.
Confirmation of the diagnosis of thrombophlebitis
During the examination, the specialist individually selects the required minimum of research for each specific case. To confirm or exclude thrombophlebitis of the lower extremities, your doctor may choose one of the following diagnostic methods:
- Blood tests (clinical blood test, coagulogram, D-dimer);
- Venography (X-ray examination of the venous bed using the injection of a contrast agent that stains the vessels from the inside). Currently, due to the development of low-traumatic and highly informative research methods (primarily duplex angioscanning), it is used extremely rarely;
- Computed tomography and magnetic resonance imaging in vascular mode - performed in situations where ultrasound diagnostic methods are not very informative;
- Ultrasound diagnostic methods (Dopplerography and duplex angioscanning) are currently the “gold standard” for diagnosing thrombophlebitis.
After a diagnosis has been established, you may need additional diagnostics to identify the causes of thrombophlebitis, as well as control studies to clarify the nature of the dynamics of the pathological process.