The human body is an almost perfect system in which each process has its own purpose. However, sometimes, if a number of circumstances coincide, the body’s defenses turn against us.
The formation of blood clots is a vital process, without which the slightest cut or damage to a vessel would result in serious consequences. But in some cases, the process of thrombus formation becomes pathological, which becomes the cause of venous thrombosis. Millions of people are diagnosed with the disease every year. This is an extremely life-threatening condition that requires immediate treatment.
What is venous thrombosis
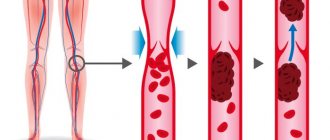
Venous thrombosis is a disease in which a blood clot forms in a vein, gradually blocking the blood flow. This provokes stretching and thinning of the walls of blood vessels. Blood circulation is disrupted, as a result of which tissues die, ulcers and necrotic tissue lesions appear. The most dangerous complication of venous thrombosis is the rupture and migration of a blood clot, which can travel to the heart or lungs in a matter of seconds. In 90% of cases this leads to death. Therefore, if pathology is present, you must immediately consult a doctor and begin treatment.
How it appears and develops
About 50 percent of patients initially do not feel any signs of thrombosis. The disease manifests itself when there is more pronounced inflammation and problematic blood flow. The calves, lower leg, foot or thigh begin to swell, depending on the location of the affected vessel. All of the above occurs due to the formation of blood clots, which at any moment can break away from the vascular walls and penetrate into the lungs.
Some of them turn into scar tissue, damaging the valves of the venous vessels. This causes even more swelling. Therefore, by the evening the patient can barely move. This is due to gravity, which further affects the swelling. It subsides during the night, as the blood vessels function better with the legs in a horizontal position.
One of the late signs of the disease is a brownish tint to the skin (above the ankle). The change in color is a consequence of the penetration of red blood cells into the skin from distended veins.
Causes of pathology
The main reasons for the development of vein thrombosis are:
- Damage to the walls of blood vessels. Injury can be caused by infections, atherosclerotic plaques, childbirth, surgery, poor nutrition, and excessive physical activity.
- Blood clotting disorder. The problem occurs due to metabolic disorders or hormone balance in the body.
- Stagnation of blood. Occurs as a result of a sedentary lifestyle.
- Infectious diseases, pathologies of internal organs (heart failure, diabetes mellitus).
- Oncology and its treatment (hormones, chemotherapy, radiotherapy).
Indirect risk factors that influence the likelihood of pathology occurring are bad habits, wearing tight clothing, and adverse effects of the external environment.
Risk group
This disease affects middle-aged and older men who have:
- injuries with vascular damage;
- addiction to smoking;
- problems with excessive body weight;
- slow blood flow;
- blood clotting dysfunction;
- undergone operations on any organs and parts of the body.
The risk group also includes pregnant women, women in labor and women who frequently take oral contraceptives. This also includes people who lead a sedentary lifestyle and those who like to sit with their legs crossed.
Symptoms of thrombosis
The main symptom of venous thrombosis is swelling of the affected limb. The pathology begins acutely and progresses quickly. In most cases, the increase in symptoms occurs within 24 hours, much less often – within 2-3 days.
Also symptoms of thrombosis are:
- increasing pain in the affected area;
- thickening of the veins at the location of the blood clot;
- swelling, bulging of superficial veins;
- a sharp change in skin color at the location of the blood clot: first redness, and after a few hours - blue discoloration.
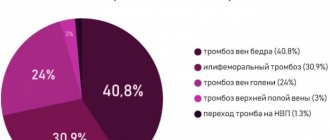
Where does thrombosis most often occur?
70% of diagnosed cases of venous thrombosis are localized in the lower extremities. The remaining 30% comes from the upper body. Let's consider the areas of the torso and upper extremities where pathology occurs most often.
Subclavian region
Thrombosis of the subclavian vein develops as a result of excessive physical activity and stress. Signs of pathology appear in influxes - sometimes intensify, sometimes disappear. This is due to the absence of serious consequences from thrombosis of the subclavian vein - blood circulation is replaced by other vessels. However, this blood is not enough to fully nourish the tissues of the upper extremities, as a result of which degenerative processes are inevitable.
The main signs of subclavian vein thrombosis are:
- pain in the arm area;
- transillumination of the venous pattern through the skin;
- swelling of the hand, the appearance of a glossy shine;
- numbness of the limb, twitching and other signs of a neurological disorder.
In the absence of correct treatment, the pathology can enter the chronic phase. Then the clinical picture of the disease becomes blurred, and the reaction of the injured limb to external stimuli is significantly reduced. The motor activity of the hand is limited, and muscle atrophy develops. Any physical activity is accompanied by acute pain. In some cases, the patient may even be assigned a disability.
Hands
The pathology has pronounced symptoms. Accompanied by redness in the area of blood clot formation, a feeling of pulsation, and pain. Neurological symptoms may also be present - twitching of the limb on the problematic side, numbness, significant limitation of motor activity. Pain in case of thrombosis can radiate to the lower back, spine, and sternum area.
Manifestations of the disease make themselves felt sharply and disappear just as quickly. Many patients confuse the symptoms of thrombosis of the veins of the arm with a pinched nerve, ignoring a trip to the doctor. However, at the first signs of circulatory problems or the appearance of acute pain, it is necessary to urgently consult a specialist.
Brachial vein
A fairly rare condition, most often occurring in young patients. It is diagnosed mainly in men. It is called Paget-Schroetter syndrome. The main signs of brachial vein thrombosis are:
- sudden pain in the shoulder area;
- feeling of warmth, burning in the affected area;
- swelling, swelling in the shoulder area;
- redness, and after 2-3 hours the skin in the problem area turns blue.
The pathology almost completely blocks the blood supply to the upper limb. Needs immediate treatment. Ignoring signs of the disease can lead to pulmonary embolism. This condition involves a blockage of the lung by a blood clot. Without emergency medical attention, this complication of thrombosis can be fatal.
Cervical veins
Jugular vein thrombosis is also diagnosed quite rarely. This is a dangerous condition - with the slightest physical exertion, a blood clot can migrate to the heart, leading to thromboembolism. The main symptoms of the pathology are:
- the appearance of edema in the jugular vein;
- tension, noticeable swelling of the vein;
- a feeling of itching and heaviness in the affected area, redness of the skin;
- weakness in the body, dizziness;
- a more pronounced manifestation of the venous pattern in the neck.
The main reasons for the development of the disease are excessive blood viscosity, problems with blood flow speed in the presence of malignant neoplasms, and concomitant cardiovascular pathologies.
Axillary area
Thrombosis of the axillary vein occurs three times more often on the right, often occurring on both sides. Pathology in this area develops as a result of repeated repeated injury to the veins due to their compression. The main symptoms of the disease are:
- swelling of the upper limb;
- intense pain syndrome, significantly intensifying after physical activity;
- in some cases, the pathology is accompanied by cyanosis of the hand;
- visual expansion of the vein, visible to the naked eye;
- redness of the skin in the affected area.
Signs of thrombosis appear suddenly and disappear just as suddenly. Ignoring the symptoms of the disease is fraught with the development of venous hypertension, detachment and migration of a blood clot under the influence of the slightest physical exertion.
Embolism.
Embolism most often leads to acute arterial occlusion. Embolism refers to the entry of a foreign body into the arterial bed, leading to its blockage. Most often, emboli are pieces of an organized blood clot, accumulations of fat or gas, or other foreign bodies (plastic tubes, metal objects, bullets). Peripheral artery embolism occurs 2 times more often in women than in men, which is explained by women’s greater susceptibility to rheumatism and longer life expectancy. Emboli can occur at any age, but more often from 40 to 80 years. The main sources of peripheral arterial embolism are currently considered to be heart disease (95% of all cases). Moreover, more than half of them are due to atherosclerotic cardiopathy: atrial fibrillation, myocardial infarction, post-infarction cardiosclerosis, cardiac aneurysms. Acquired heart disease accounts for 40-43% and congenital defects 1-2%. In atherosclerotic cardiopathy, the thrombus is usually localized in the left ventricle, and in case of heart defects in the left atrium or its appendage. Following arterial embolism, acute ischemia of the limb or organ supplied by this vascular system develops. Its severity will depend on a number of factors: 1. the severity of bypass circulation, 2. continued thrombosis, 3. arterial spasm, 4. the state of central hemodynamics. A drop in intravascular pressure to a stagnation level leads to platelet aggregation and the formation of blood clots in the microcirculation system. As a result, irreversible changes in tissues occur. Later, thrombosis develops in larger arteries. Different tissues vary in their tolerance to ischemia. So in the tissues of the extremities, irreversible changes with complete ischemia occur after 6-8 hours, in the intestines after 2 hours, in the kidneys 40-50 minutes, in the brain after a few minutes.
Clinical course and symptoms of peripheral artery embolism.
The main symptom of arterial embolism is pain in the affected limb. It occurs suddenly and is very strong. Sometimes patients fall, unable to withstand this severe pain. Along with pain, patients often note a feeling of numbness in the limb. Upon examination, a change in the color of the skin of the limb is striking: from pronounced pallor to a “marble” color. In the late stage of ischemia, when thrombosis of the venous bed occurs, the color of the skin becomes cyanotic. With comparative palpation, the difference in skin temperature is noticeable, especially in the distal parts of the limb. There is also a disorder of all types of sensitivity (pain, tactile, deep). The border of sensitivity disorder does not coincide with the level of artery occlusion, but is located below, which should not mislead the diagnostician. An equally characteristic symptom is a violation of active movements in the joints of the limb, which vary in degree from limitation to complete plegia. In the late stage of severe ischemia, passive movements may also be absent due to stiffness of muscles and joints. Joint contracture is an unfavorable sign indicating the non-viability of the limb. The absence of a pulse in the arteries located distal to the level of blockage is also one of the important symptoms of embolism. With severe swelling of the limb, it is sometimes difficult to determine the pulse. Slow filling of the saphenous veins, or the “groove” symptom, also indicates poor circulation. Sometimes there is increased pulsation in the arteries located proximal to the occlusion, determined by comparative palpation. In advanced cases, severe muscle soreness on palpation, rigidity and subfascial edema are observed. Various classifications have been proposed to assess the severity of limb ischemia. The classification proposed by V.S. Savelyev and co-authors in 1978 most fully meets practical purposes. The diagnosis of great artery embolism is usually made on the basis of physical findings. Additional research methods include ultrasound, radioisotope and X-ray contrast angiography. In this case, the main purpose of their use is to establish the patency of arteries located distal to the occlusion. It should be noted that due to spasm of both main and collateral vessels, the information content of these methods is sharply reduced.
Treatment at the prehospital stage.
Pain relief is achieved by administering drugs or analgesics. An important point is the administration of anticoagulants (10 thousand units of heparin) to prevent continued thrombosis. If necessary, cardiotonic drugs are prescribed. The main method of treatment for embolism of the aorta and peripheral arteries should be surgical, aimed at restoring blood flow in all patients who do not have absolute contraindications to surgery.
Surgery.
The operation of choice is embolectomy. The best results are obtained in the early stages (6-8 hours) after the development of embolism. At later stages, irreversible tissue changes may develop. However, the timing itself does not determine the indications for surgery. Embolectomy can be successfully performed even after several days, if the limb is still viable.
Diagnosis of thrombosis
When visiting a medical facility, the doctor diagnoses the pathology and prescribes treatment. The main methods used to detect thrombosis are:
- coagulogram - blood test for clotting;
- magnetic resonance venography;
- duplex\triplex scanning of the veins of the upper extremities;
- ascending venography using a contrast agent;
- radionuclide scanning of the location of the thrombus;
- thromboelastography.
Ultrasonography
Ultrasound duplex scanning of veins is the “gold standard” for diagnosing thrombosis localized in the upper extremities. The technique allows you to quickly, highly informatively and non-invasively obtain information about the state of venous blood flow. The method is ideal for visualizing the veins of the extremities, neck, axillary and subclavian areas.
CT scan
Another popular method for diagnosing thrombosis. It is used mainly urgently, in case of suspected dangerous complication of deep vein thrombosis - pulmonary embolism. CT allows you to quickly assess the extent of the problem and select the most appropriate method of providing emergency medical care.
General characteristics of the disease
Venous thrombosis (deep vein thrombosis) is a disease characterized by the formation of a blood clot (thrombus) in the blood vessels. The thrombus begins to interfere with normal blood flow, and occlusion (blockage) of the vessel occurs. Over time, the size of the thrombus increases, which leads to complete closure of the venous lumen in a certain area.
Important! Deep vein thrombosis is a very dangerous disorder of the vascular system. Occurring in any deep vessel, it can lead to a number of serious complications, including death. In addition, damage (stretching) of the venous membrane by a thrombus is dangerous in itself. That is why treatment of this terrible disease must begin as soon as possible.
Request a call back Get a free consultation
Treatment of thrombosis
If you suspect thrombosis, you should consult a doctor as soon as possible. The sooner you do this, the higher the likelihood that you will be able to avoid irreversible consequences of the pathology and a significant deterioration in the quality of life.
Depending on the condition of the affected vein, treatment can be carried out using several methods.
Conservative treatment
Involves the use of blood thinning medications. Anticoagulants are available in the form of tablets and injection solutions. The minimum duration of therapy is 3 months. In some cases, anticoagulants are indicated for many months or even years. The treatment period is determined by the doctor in each case individually, depending on the size and flotation of the blood clot, and the presence of concomitant diseases.
Minimally invasive techniques
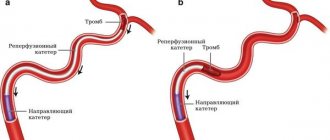
If a mobile thrombus is detected in a patient’s vein, the patient is advised to undergo strict bed rest. In this case, implantation of a vena cava filter is necessary. The operation involves inserting a catheter with an umbrella-shaped device through the femoral vein to the affected area. When the conductor reaches the desired location, the filter is opened and the catheter is removed. The device is necessary to catch pieces of a blood clot if it migrates. In this way, it is possible to prevent deadly complications of thrombosis - pulmonary embolism, thrombophilia.
The operation is performed under local anesthesia and takes a maximum of an hour. The patient can go home the very next day after the intervention. Within a week after surgery, it is necessary to carry out X-ray monitoring of the position of the vena cava filter. The patient is also advised to undergo dynamic monitoring - every six months he needs to visit a doctor to assess the current state of the cardiovascular system.
Another way to solve the problem of thrombosis is stenting. It is used in case of a small blood clot. A special guide is inserted through the femoral access, with the help of which a metal stent is delivered to the damaged area. It expands, pressing the blood clot into the wall of the vessel and thus fixing it. The stent ensures normal patency of the vessel and eliminates the blood clot. The operation is performed under local anesthesia. The patient remains in the hospital for 24 hours after the intervention, after which he can go home. Stenting is one of the most modern methods of endovascular treatment of thrombosis and atherosclerosis.
Treatment with surgery
If the blood clot threatens the patient's life, surgery is indicated. The surgical technique is selected by the doctor based on the results of a comprehensive examination. There are several ways to surgically treat thrombosis.
Bypass surgery
The operation involves removing the affected section of the vein along with the blood clot and replacing it with a natural vascular implant taken from another part of the patient’s body. In some cases, an artificial vessel prosthesis can be used. The intervention is performed through abdominal access. After the operation, the patient will have a long rehabilitation period.
Thrombectomy
It involves surgical intervention aimed at removing a blood clot from the vessels. Depending on the location of the thrombus and its size, the following may be used:
- Traditional technique. To remove the blood clot, abdominal access is provided. The patient is put into medicated sleep. The operation lasts several hours, the rehabilitation period is 3-4 weeks. This is a serious intervention that is prescribed only in extreme cases.
- Endovascular technique. It involves removing a blood clot through a femoral approach using modern instruments. It is used in case of a small blood clot.
The main indications for thrombectomy are:
- closure of a large vessel with a thrombus;
- During the diagnosis, a large blood clot was discovered that interfered with normal blood flow in the vessels;
- the appearance of a floating thrombus;
- pregnancy;
- a critical health condition of the patient in which a blood clot threatens the patient’s life.
It is important to understand: none of the above methods provides a guarantee that a blood clot will not form again. To avoid the recurrence of thrombosis, the patient must strictly follow all the doctor’s recommendations, as well as radically change his lifestyle.
Therapeutic tactics
When lesions of the brachiocephalic vessels are detected, specialists traditionally choose conservative treatment tactics. It involves taking certain medications (anticoagulants or antiplatelet agents), vitamin therapy, and diet therapy. The patient is given detailed recommendations regarding lifestyle and nutrition correction. He is obliged to control the level of cholesterol in the blood, as well as monitor the condition and stability of blood pressure.
Surgical intervention as a therapeutic tactic is chosen in conditions of a direct threat of stroke. If there is no immediate risk, the patient is registered and observed.
Surgical intervention happens:
- Open (resection of the affected arterial section with its immediate prosthetics or suturing);
- Endovascular (introduction of a stent into a vessel).
The category of open interventions includes endarterectomy (carotid eversion).
Stenting is a more modern, atraumatic and effective method, but it is acceptable and not indicated in every case. The later you seek professional medical help, the less likely you are to be cured using these methods.
Diseases of the brachiocephalic arteries are a serious disorder leading to unpredictable consequences. We urge you to promptly contact vascular surgeons with alarming symptoms in order to avoid the need for aggressive treatment and save your life.
Prevention
The development of venous thrombosis can be prevented. There are a number of generally accepted recommendations, adherence to which will help avoid problems with the cardiovascular system:
- Use elastic bandages as prescribed by a doctor. They help maintain blood vessels in tone and prevent congestion in the limbs.
- Quitting smoking and alcohol. Bad habits have a sharply negative impact on all body systems, being a major risk factor for the development of cardiovascular diseases.
- Rational, proper nutrition. Refusal of fatty, fried, salty, smoked, flour, and sweet foods is the key to a healthy heart and blood vessels. The diet should be complete and varied. Eat more vegetables and fruits, whole grain cereals, poultry, fish, and dairy products. Limit your pork consumption. Try to eat more greens, add natural seasonings and spices to your dishes. Avoid sausages, hot dogs, and processed foods.
- Taking vitamins and microelements. It is necessary to visit a doctor and get tested for a lack of certain vitamins in the body. Based on the results of the study, the specialist will prescribe the most suitable medications for your case.
- Optimal physical activity. Stagnation in the bloodstream should not be allowed. Doctors recommend walking for at least half an hour every day. If you have a sedentary job, you should spend 3-5 minutes exercising every hour. It is also necessary to monitor your posture and stretch regularly to restore normal blood flow.
- Adequate fluid intake. Water is vital for the body to function properly. Make it a habit to drink a glass of clean water in the morning, before bed and before every meal.
- Refusal to visit the bathhouse, sauna, or take hot baths. Exposure to high temperatures does not have the best effect on the heart and blood vessels. And if there is a genetic predisposition to varicose veins and thrombus formation, bath procedures significantly increase the likelihood of developing vascular bed pathologies.
- Normalization of weight. Obesity negatively affects the condition of the cardiovascular system. Fatty deposits in tissues and internal organs compress veins and arteries, which impairs blood circulation and significantly impairs the delivery of vital substances to the tissues.
- Timely treatment of concomitant diseases. Malignant and benign tumors, inflammatory processes in internal organs - all this negatively affects blood circulation, which can lead to blockage of blood vessels.
- Control of cholesterol and blood glucose levels. These are vital signs that need to be monitored constantly. Controlling cholesterol levels will help avoid the development of atherosclerosis, which is one of the most common causes of varicose veins. Sugar levels must be monitored in order to promptly notice negative changes that can lead to diabetes.
- Regularly undergoing comprehensive examinations. This is especially true if your closest relatives have cardiovascular pathologies. These diseases are classified as hereditary. Therefore, “keeping your finger on the pulse”, you will be able to detect in time even the slightest changes in the functioning of the heart or the condition of the blood vessels.
The state of a person’s cardiovascular system directly depends on his lifestyle. Serious pathologies can be prevented by following the above recommendations. If the problem already exists, do not put off visiting a doctor. Contact trusted, reliable specialists, undergo a comprehensive examination, consult a doctor about available treatment methods. Don't risk your health. Thrombosis is very dangerous!