The human intestine is supported by a special tissue - the mesentery, the vessels of which supply the organ with blood. Each of these vessels (they are called mesenteric) is responsible for supplying blood to a specific area of the intestine. When blood circulation is impaired in the vessels of the mesentery, mesenteric thrombosis develops. In essence, this acute condition is an intestinal infarction and often ends in death. While myocardial infarction is easily diagnosed, intestinal thrombosis is difficult to detect, especially at the onset of the disease.
This pathology occurs mainly in middle-aged and older people, regardless of gender. Intestinal infarction most often develops with acute occlusion of the trunk or mouth of the superior mesenteric artery. The trunk is usually divided into three segments; in case of thrombosis or embolism of each of them, a certain localization of intestinal damage is observed.
When the first segment is blocked, most patients experience thrombosis of the small intestine, as well as the blind and right half of the colon.
With occlusion of the second segment, the entire ileum and part of the jejunum, rarely the ascending colon and cecum, are affected.
When the third segment is blocked, the blood circulation is usually compensated, and during a heart attack only the ileum is affected.
General information about thrombosis
Thrombosis
ー the process of intravital blood coagulation in the cavities of blood vessels and the heart. This process is also dangerous because part of the blood clot can break off and be carried by the bloodstream to other organs. For example, with thrombosis of the deep veins of the lower extremities, thromboembolism of the pulmonary artery or cerebral vessels often develops.
Mesenteric thrombosis: forms, types and stages of the disease
According to the form of the process, chronic and acute mesenteric intestinal thrombosis are distinguished. It can be localized only in the veins, only in the arteries, or have a mixed type, in which blood flow is first disrupted in the mesenteric arteries, and then in the venous vessels.
!
Medical statistics indicate that the upper sections of blood vessels suffer from blockage more often than the lower ones.
Based on the degree of disruption of collateral blood flow and main arteries, it is customary to distinguish 3 main stages of the disease:
- With compensation:
This stage is considered chronic intestinal ischemia. Blood flow in which is carried out due to unaffected vessels.
- With subcompensation:
Partial blood supply to the intestines;
- With decompensation:
An extremely difficult stage, which in most cases is characterized by irreversible consequences. The blood supply to the intestines is completely absent, which causes a heart attack. Its first phase is only no more than 120 minutes. At this time, there is still a chance for the process to be reversible. After 4 hours, the second phase begins, in which gangrenous damage to the organ rapidly develops. This stage in most cases ends in death.
Classification of thrombosis
Depending on the location of the pathological process:
Arterial:
- arteries of the brain;
- hearts;
- intestines (mesenteric thrombosis);
- liver;
- femoral artery and others.
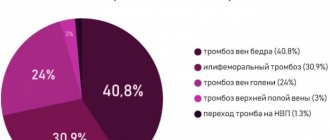
Venous (phlebothrombosis):
- veins of the lower limb;
- hemorrhoidal plexus;
- femoral and iliac veins;
- cavernous sinus (intracranial collector of venous blood);
- retinal veins.
According to the severity of the disease, acute
ー a sharp blockade of blood flow, and
a chronic
ー thrombus grows gradually, the tissues have time to adapt to this and compensate for pathological changes.
Main causes
There are three main factors for thrombus formation.
- Damage to the vessel wall
(as a result of injury, surgery and poor nutrition (cholesterol plaques form), infection, heavy lifting, childbirth, etc.). - Blood clotting disorder
(tendency to increased clotting). Changes in blood clotting may occur due to metabolic disorders or hormonal imbalances. - Stagnation of blood
. It occurs when a person remains motionless for a long time in one position (for example, in front of a computer, in an airplane seat, or chained to a bed).
The risk group also includes people with varicose veins, those who are overweight, bad habits, leading a passive lifestyle, as well as people over 60 years of age.
Mechanism of development and causes of thrombosis
There are three pathological parts in the process of intravascular thrombus formation:
- Violation of the integrity of the vascular wall. When the internal lining of blood vessels is damaged, enzyme systems are activated, which trigger the process of blood clotting.
- Slowing blood flow. This occurs when the outflow is disrupted (compression of veins, varicose veins), prolonged absence of limb movement, or heart failure.
- Blood thickening. Caused by dehydration, autoimmune diseases, chemotherapy, and oral contraceptives.
A blood clot often forms against the background of such diseases:
- atherosclerosis;
- heart failure;
- aneurysms of blood vessels and heart;
- diabetes;
- obesity;
- bone fractures;
- hormonal disorders;
- oncological diseases.
Diagnostics
Differential diagnostic methods include laboratory and instrumental tests:
Read also: Why does the stomach bloat and hurt, symptoms, methods of treatment, diagnosis, prevention and risk factors
- Blood tests. With intestinal thrombosis, an inflammatory process develops, so an increase in ESR and leukocyte count will likely be detected,
- X-ray. It is performed after the introduction of a radiopaque substance into the vascular bed. The method allows you to quickly determine the location and extent of damage to the mesenteric arteries,
- Laparoscopy. The method involves inserting an optical tube equipped with a light source and camera into the abdominal cavity through small incisions. The picture is displayed on the monitor, the doctor can thus examine the intestinal walls and assess the blood flow in the arteries,
Laparoscopy
- Laparotomy. The procedure is used when laparoscopy is not possible. The operation is performed by making a direct incision in the abdominal wall. If intestinal lesions are detected, the surgeon immediately removes the area.
Thrombosis in children
Possible causes of blood clot formation in children:
- thrombophilia - congenital deficiency of anticoagulant blood factors;
- leukemia, other oncological diseases;
- cutaneous fulminant purpura, disseminated intravascular coagulation syndrome (develops with severe intoxication, inflammatory diseases: pancreatitis, peritonitis, etc.);
- the presence of antiphospholipid antibodies, lupus anticoagulant, and other autoantibodies (antibodies to one’s own cells).
Episodes of blood clots in a child should prompt a serious examination to determine the cause.
Treatment
Treatment of thrombosis of intestinal vessels is possible only with immediate surgery. The introduction of painkillers and antispasmodics erases the clinic and delays the diagnosis.
For vein thrombosis, fibrinolytic therapy is indicated in the first 6 hours.
During the operation, the doctor must find ways to:
- in the absence of necrotic changes, restore the patency of blood flow through the vessel to relieve ischemia from the affected area of the intestine;
- remove the altered intestine or part of it and sew the upper and lower ends.
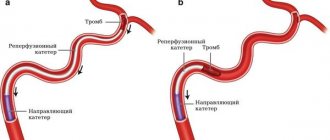
Restoring blood supply is carried out in the following way:
- squeezing out a blood clot with your fingers;
- creation of a bypass shunt between the upper and lower levels of the stenosis, bypassing the thrombosed area.
In the postoperative period, the patient is prescribed large doses of Heparin to thin the blood.
An angiogram of the intestinal arteries in an emergency is difficult because it requires patient preparation
Risk factors for thrombosis
The following factors increase the likelihood of developing the disease:
- age over 50 years;
- obesity;
- smoking, alcoholism, drug addiction;
- poor nutrition;
- sedentary lifestyle;
- injuries;
- the need for frequent intravenous injections and procedures associated with violation of the integrity of blood vessels (blood sampling, hemodialysis, installation of a venous catheter) increases the risk of developing phlebitis and inflammation of the venous wall.
What is colonic ischemia?
Ischemic colitis (synonymous with ischemic colonopathy)
– inflammatory changes and disruption of the integrity of the colon wall, caused by impaired blood supply to the intestinal wall. The main reason for insufficient supply of arterial blood to the intestinal wall in old age is atherosclerosis of the vessels supplying the colon.
Most often, ischemic disorders affect the left parts of the colon (splenic flexure in 80% of cases), which is due to the peculiarities of the blood supply to the intestine in this area. The rectum, which has an abundant blood supply, is extremely rarely susceptible to ischemic lesions. The large intestine normally has less blood supply than the small intestine and, accordingly, is more sensitive to ischemia.
In addition, it has been shown that the physiological motor activity of the colon is accompanied by a decrease in blood flow, while, for example, the blood supply to the small intestine increases during digestion and peristaltic activity.
Thus, the combination of a normally reduced blood supply and decreased blood flow during functional activity
distinguishes the colon as a unique blood flow organ.
Reduced blood flow in the colon has also been observed as a result of exposure to emotional stress
.
An additional factor
constipation
that increases intestinal ischemia in the elderly . Chronic constipation (straining) increases intraintestinal pressure and reduces blood flow in the colon wall.
The most common form of colon ischemia is reversible (transient) violations of the integrity of the intestinal wall, occurring in 60% of cases. With the progression of atherosclerosis and a critical disruption of the blood supply to the intestines, tissue necrosis occurs with the development of severe conditions requiring emergency surgical treatment.
With ischemia of the colon, the mucous membrane is primarily affected, since it is especially sensitive to hypoxic conditions.
Apparently, this is due to the high activity of metabolic processes occurring in it. As the degree of ischemia increases, damage spreads from the mucous membrane towards the submucosal and muscular layers. In severe forms, deep damage occurs, often resulting in perforation or stricture formation.
Symptoms of thrombosis
The clinical manifestations of this pathology vary depending on the location.
Symptoms of venous thrombosis
When a vein is blocked, the outflow of blood is hampered, so the tissues beyond the blockage swell and turn blue. The waste products of cells accumulate, therefore tissue intoxication develops, this is accompanied by pain, impaired sensitivity (the sensation of “crawling goosebumps”). If you do not intervene in time, the tissues begin to die.
Symptoms of venous thrombosis of the lower extremities:
- swelling of the leg, a sharp increase in size, cyanosis;
- cramps of the calf muscles;
- constant pain in the leg, which intensifies when walking;
- increased venous pattern on the thigh.
Cavernous sinus thrombosis:
The dura mater contains channels into which venous blood from the brain drains. Blockage of one of these sinuses, the cavernous sinus, is dangerous because several cranial nerves and the internal carotid artery pass through it. The most common causes of cavernous sinus thrombus formation are inflammatory diseases of the nose, sinuses, facial skin and scalp. Signs:
- headache;
- decreased visual acuity, double vision;
- confusion;
- heat, fever;
- swelling of the eyelids and periocular area;
- pain in the neck when turning or tilting the head;
- impaired facial skin sensitivity.
Among the consequences of such thrombosis: stroke, loss of vision, coma.
Hemorrhoidal thrombosis
Develops against the background of hemorrhoids. Chronic constipation, physical stress, pregnancy and childbirth, and alcohol abuse contribute to it. Signs:
- pain, burning and itching in the anal sphincter area;
- discharge of blood with feces and regardless of the act of defecation;
- prolapse of hemorrhoids.
Retinal vascular thrombosis
The pathology is a typical complication of diabetes mellitus and hypertension, but can also develop for other reasons. Symptoms:
- deterioration of vision, up to complete loss (usually one-sided);
- the appearance of spots, mesh, veils before the eyes.
Symptoms of arterial thrombosis
Blockage of the artery leads to oxygen and energy starvation of tissues, which quickly leads to their death. Arterial forms of the disease are often acute.
Thrombosis of the cerebral arteries
This process leads to necrosis of the area of the brain that the affected artery supplies blood to - ischemic stroke. Signs:
- hemiparesis ー lack of movement in the right or left half of the body (opposite affected area);
- asymmetry of the smile - one corner of the mouth is lowered, does not take part in conversation and smile;
- unclear speech;
- when the patient sticks out his tongue, it deviates to the side.
Thrombosis of the coronary arteries of the heart
Partial blockage of these vessels leads to attacks of angina pain, complete blockage leads to myocardial infarction. Symptoms:
- pressing, burning pain behind the sternum, radiating to the left shoulder blade, arm, shoulder, half of the face and neck;
- dyspnea;
- with angina pectoris, rest and nitroglycerin help, with a heart attack there is no improvement, urgent medical attention is needed.
Pulmonary artery thrombosis
It is a complication of thrombosis of the veins of the lower extremities, endocarditis, myocardial infarction. It develops rapidly and has a high mortality rate. Signs:
- sharp stabbing pain in the chest;
- swelling of the veins of the neck;
- shortness of breath, feeling of lack of air;
- hemoptysis;
- increased heart rate.
Hepatic artery thrombosis
Death (infarction) of liver tissue is a complication of endocarditis, myocardial infarction or liver transplantation and manifests itself as follows:
- severe pain under the right rib;
- nausea, vomiting, bitterness in the mouth;
- yellowness of the skin and whites of the eyes.
Femoral artery thrombosis
This form of pathology is manifested by pain when walking, coldness, and paleness of the limb. The pulse in the popliteal fossa and on the foot is palpable weakly or not detected at all.
Where do blood clots and emboli come from?
Through the arterial system, the embolus can reach the mesentery:
- from the heart in case of detachment of a parietal thrombus from the wall of a post-infarction aneurysm, during atrial fibrillation, from the inner layer (epicardium) during sepsis, destruction of valves;
- from the thoracic and abdominal aorta during vessel dissection, softening of atherosclerotic plaques;
- is formed in the mesenteric artery after traumatic damage to the inner layer.
Venous blood, having the opposite direction and a tendency to decrease speed and increase viscosity, is more susceptible to the formation of its own thrombotic masses. The formation of blood clots in the veins is caused by:
- inflammatory bowel diseases, affecting the entire wall, also involve venous vessels, local thrombophlebitis is formed;
- drop in blood pressure caused by various situations;
- portal hypertension in liver diseases;
- congestion in the underlying vessels due to portal vein thrombosis;
- any reasons that increase blood viscosity (diseases of the hematopoietic system, condition after splenectomy, long-term use of hormonal drugs to prevent pregnancy).
If the patient has a heart defect in which the right and left chambers communicate with each other (for example, patent foramen ovale), then a thrombus from the lower extremities can freely pass through the vena cava, the right atrium into the left ventricle and aorta, and then descend to the intestinal arteries .
Diagnosis and treatment of thrombosis in Medical
Specialists from the Paracelsus Medical Center will help in diagnosing and eliminating this pathology, provide support during the rehabilitation period, and give recommendations for further prevention.
Our center uses expert-class equipment from leading global manufacturers for diagnosis and treatment. The consultation is conducted by practicing phlebologist surgeons.
On the basis of "Operating Room No. 1" phlebological operations are performed for venous disease. The key advantage of the Paracelsus Medical Center network is highly qualified professional surgeons with extensive practical experience.
Drug treatment
The basis of drug therapy is anticoagulants (thin the blood, prevent the growth of a blood clot), fibrinolytics and thrombolytics (dissolve existing clots), antiatherosclerotic drugs (lower cholesterol levels). If necessary, analgesics, anti-inflammatory drugs, cardiotonic drugs, vitamins, minerals, etc. may be needed as symptomatic therapy.
Surgery
There are such methods of surgical treatment of the disease:
- thrombectomy ー removal of a blood clot;
- stenting (expansion using a frame) and shunting (creating a bypass path for blood flow) for atherosclerotic artery disease;
- arteriovenous shunting.
If the thrombus cannot be removed, a vena cava filter can be installed - the device is placed in the vein above the level of blockage to prevent it from moving and closing the lumen of the vessels of vital organs.
Prevention
Preventive actions:
- Using elastic bandages and compression garments
- To give up smoking
- Rational and proper nutrition
- Vitamin therapy
- Physical activity
- Timely treatment of concomitant diseases
- Monitor cholesterol and blood glucose levels
- Reducing body weight.
If symptoms of the disease appear, you can seek advice and examination in Moscow from specialists from the Central Clinical Hospital of the Russian Academy of Sciences. Registration is made by phone...
Disease prognosis
The outcome of thrombosis varies. Favorable ones include aseptic autolysis of a blood clot, which occurs under the influence of proteolytic enzymes of leukocytes. Small thrombi can be completely subjected to aseptic autolysis. More often, blood clots, especially large ones, are replaced by connective tissue, that is, they are organized. The ingrowth of connective tissue into a thrombus begins in the region of the head from the intimal side of the vessel, then the entire mass of the thrombus is replaced by connective tissue, in which cracks or channels lined with endothelium appear, the so-called. clot drainage. Later, the channels lined with endothelium turn into vessels containing blood; in such cases, they speak of vascularization of the thrombus, which often restores the patency of the blood vessel. However, the organization of a thrombus does not always end with its canalization and vascularization. Calcification of the thrombus and its petrification are possible; In this case, stones sometimes appear in the veins - phleboliths [3, 9, 10, 13].
Unfavorable outcomes of thrombosis include: • separation of a thrombus or part of it and transformation into a thromboembolus, which is a source of thromboembolism; • septic melting of a blood clot, which occurs when pyogenic bacteria enter the thrombotic masses, which leads to thrombobacterial embolism of the vessels of various organs and tissues (in sepsis). The prognosis for PVT is completely determined by the etiology of the disease. In adults with PVT, the 10-year survival rate is, according to various sources, 38–60% [9, 21]. Patients die mainly from complications of underlying diseases (cirrhosis, liver cancer). Mortality from bleeding from varicose veins in patients with PVT without cirrhosis does not exceed 5%, while in patients with cirrhosis this figure is 30–70% [9,21].
In conclusion, it should be noted that PVT is a serious disease that requires immediate diagnosis and intensive treatment in order to prevent complications, such as the formation of cavernous transformation and progression of PG. The survival of patients with portal thrombosis directly depends on the speed and thoroughness of diagnosis, the use of modern methods of instrumental and laboratory examination and visualization of thrombosis, and the assessment of concomitant thrombophilic conditions that increase the risk of complications. Early anticoagulant and antiplatelet therapy promotes reperfusion of thrombosed areas of the veins of the portal system and, despite the risk of gastrointestinal bleeding, is necessary for patients with PVT, as well as with diagnosed PG and cavernous transformation of VV.