Protein deficiency: what is it?
Now this problem is called a little differently - protein-energy deficiency (PEM).
This pathology is characterized by a low level of biologically active elements and energy, which negatively affects the functioning of the body's systems. Signs of PEM manifest themselves clearly:
- Rapid weight loss (up to 10%);
- Nervous system disorder;
- Dry skin and paleness.
To diagnose pathology, examination and laboratory tests are necessary. This will help assess the person's condition. Instrumental methods are necessary to identify the root cause of pathology.
Treatment includes high-protein and high-calorie enteral, tube or parenteral nutrition.
Causes
A common cause of pathology is a factor associated with socio-economic conditions. People's low income does not allow them to buy food with sufficient calories and vitamins. Living in regions where natural disasters often occur or military operations are taking place is also a reason for the occurrence of PEM in people.
Of course, the following diseases also contribute to the occurrence of PEM:
- Deficiency of biologically active elements (nutrients). This is caused by strict diets for gastroenterological and metabolic diseases, switching to parenteral nutrition, anorexia, and psychosis.
- Increased metabolic breakdown of cells and tissues (catabolism). The cause of this may be thyrotoxicosis, diabetes mellitus, and oncology.
- Digestive disorders. The most common causes of the disorder are chronic gastroenteritis, pancreatic steatorrhea, and bile dysfunction.
- Intoxication. The reasons are the use of potent drugs for a long time, polypharmacy, alcoholism.
- Alzheimer's and Parkinson's diseases. This is typical for older people.
In children, congenital causes are of primary importance in the structure of PEM:
- Developmental disorders;
- Neuromuscular pathologies;
- The problems are genetic.
Protein deficiency is a painful condition of the body associated with insufficient intake and absorption of protein or with its increased breakdown. A true deficiency in protein intake from food can develop in people who have been undernourished for a long time, adhering to so-called mono-diets, or in vegetarians. Secondary protein deficiency, associated with its increased breakdown, can accompany a number of diseases, for example, severe forms of infectious diseases, burns, kidney pathologies, and hereditary metabolic disorders. Proteins are the main building material of the body, so even mild forms of protein deficiency, which are outwardly asymptomatic, affect the ability to resist infection or the rate of wound healing, slow down the growth of nails and hair, and cause dry skin. Severe protein deficiency can disrupt the normal functioning of all organs and systems. Protein deficiency in childhood is especially dangerous, as it can affect the development of mental abilities, muscle formation, and slow down the child’s growth.
Timely detection of protein deficiency and establishment of its cause is extremely important, as it allows one to avoid life-threatening complications.
Synonyms Russian
Protein deficiency, protein dystrophy, protein-energy deficiency.
English synonyms
Protein Deficiency.
Symptoms
Mild forms of protein deficiency are most often asymptomatic. An exception may be hereditarily determined deficiencies of individual amino acids (structural components of the protein molecule), the characteristic signs of which are observed in early childhood.
External manifestations of protein deficiency:
- general weakness;
- progressive weight loss;
- fragility, dullness and hair loss;
- brittle nails;
- dryness and flaking of the skin;
- swelling.
Manifestations from the nervous system:
- lethargy and increased fatigue;
- headache;
- decreased mental activity;
- unstable mood;
- insomnia.
Manifestations from the musculoskeletal system:
- pain in muscles and less often in joints;
- slow growth (in children);
- reduction in muscle mass and apparent volume;
- muscle weakness.
From the digestive organs:
- increased craving for sweets;
- nausea;
- abdominal pain and bloating;
- stool disorders (constipation followed by diarrhea);
- liver enlargement.
Who is at risk?
- Population of countries with low living standards.
- Vegetarians.
- Persons following a mono-diet or fasting in order to lose weight.
- Patients with kidney diseases.
- Patients with diseases of the digestive system.
- Persons with a hereditary predisposition to protein metabolism disorders.
- Persons with professionally caused weight deficiency: ballerinas, models, gymnasts.
- Persons over 60 years of age.
General information about the disease
Proteins are among the essential nutrients that perform the following functions in the body.
- Construction - protein is part of all cells of the human body and, in fact, is the basis for the existence of life.
- Frame – proteins are involved in the formation of hair and nails, form the protective membrane of the eye, cartilage, tendons and ligaments. Even such a property as the smoothness of the skin directly depends on the protein it contains.
- Motor and contractile. Proteins are the main component of muscle tissue that ensures its functioning.
- Transport. Many proteins have the ability to bind to nutrients contained in the blood and transport them to organs and tissues. An example of a transport protein is hemoglobin, contained in red blood cells (erythrocytes) and transporting oxygen.
- Protective. The body produces specific proteins (antibodies) that provide protection against microorganisms and viruses.
- Enzymatic. Enzymes are proteins that are involved in all chemical processes occurring in the body (for example, in the digestion of food).
- Hormonal. Most of the hormones in the human body are proteins.
The implementation of these functions occurs due to protein metabolism - constantly occurring processes of protein formation (synthesis) and breakdown.
The main causes of protein deficiency:
- Severe and long-term illnesses require the body to use all its reserves. Proteins are spent to replenish energy costs and restore dead cells. In a number of diseases, significant protein loss occurs.
- Chronic kidney disease (glomerulonephritis, renal failure, nephrotic syndrome) can lead to the excretion of significant amounts of protein in the urine (proteinuria), causing a drop in protein levels and chronic protein deficiency.
- Liver cirrhosis and liver failure can cause protein deficiency, especially in the later stages of the disease, when edema develops - fluid containing large amounts of protein (ascites) can accumulate in the abdominal cavity. The liver synthesizes many proteins necessary for the body, and the digestive enzymes it produces are involved in their absorption. With cirrhosis, normal liver function is disrupted and protein deficiency may develop.
- Burns (burn disease). With thermal burns, blisters filled with protein-containing liquid may form on the skin. Protein losses when opening these bubbles can be quite significant.
- Diarrhea (diarrhea) is characterized by a significant loss of fluid and digestive juices containing proteins.
- Malignant neoplasms in late stages can lead to severe protein deficiency. The protein is spent on tumor growth, and is also lost during its decay and bleeding. Substances formed in tumor cells are foreign to the body. Once in the blood, they cause poisoning by decay products (cancer intoxication syndrome), one of the manifestations of which is a drop in protein levels.
- Diabetes mellitus can cause protein deficiency due to increased protein breakdown, as well as diabetic kidney damage and secondary proteinuria.
- Disorders of protein-amino acid metabolism. Proteins are complex substances that, like a chain, are made up of units called amino acids. The sequence of amino acids is individual for each organism, therefore the protein supplied with food during the digestion process is broken down to the level of individual links, from which its own sequence is then composed. At the same time, some amino acids can be formed in the human body, while others (they are also called essential) come only from food. The role of essential amino acids is so great that without them, protein formation becomes impossible. If any essential amino acids are missing from the diet or are not absorbed, the balance between protein breakdown and synthesis may shift toward breakdown and lead to protein malnutrition.
- Impaired digestibility of essential amino acids is a hereditary pathology. The following diseases are most significant in the development of chronic protein deficiency.
- Phenylketonuria is a metabolic disorder of the amino acid phenylanine. Phenylanine is involved in the formation of almost all proteins of the human body, primarily proteins of the nervous system. The disease is characterized by the absence or insufficient level in the liver of a special protein (enzyme) responsible for the absorption of this amino acid. As a result, its excessive accumulation in tissues occurs. Phenylketonuria is usually diagnosed in early childhood and is accompanied by various disorders of the nervous system, as well as retardation in physical development. Without treatment, it can lead to mental disability.
- Tyrosine metabolism. Tyrosine is an amino acid necessary for the formation of one of the main protein pigments of the human body - melanin, therefore one of the manifestations of impaired metabolism is albinism (pale skin, discoloration of hair and iris). Tyrosine is also required for the formation of thyroid hormones.
- Disturbances in protein synthesis can lead to insufficient protein formation or the appearance of so-called defective, or pathological, proteins that are unable to perform their functions. For example, with a hereditary disease such as sickle cell anemia, hemoglobin is detected in the blood, which is not able to carry the same amount of oxygen as normal. Acquired disorders of protein synthesis can be caused by malignant tumors or taking certain medications.
- Alimentary (digestive) protein deficiency is the most common form of protein deficiency. It can develop under the following circumstances:
- Insufficient protein intake from food. Some diets include limiting animal protein (meat), replacing it with vegetable protein, or completely eliminating proteins. Prolonged fasting can also lead to protein deficiency. In the latter case, irreversible protein breakdown may begin, which poses a threat to life.
- Protein digestion disorders can develop in diseases of the gastrointestinal tract, accompanied by insufficient production of digestive juices, for example, in atrophic gastritis with reduced secretory function.
Depending on the severity, protein deficiency can lead to:
- retardation in mental and physical development;
- weakening of memory and intelligence;
- weakening of the body's defense system.
Diagnostics
Protein deficiency may be primarily suspected in patients with underweight, as well as in individuals with symptoms of diseases characterized by protein deficiency. To confirm the diagnosis, a complex of studies is carried out.
Laboratory research
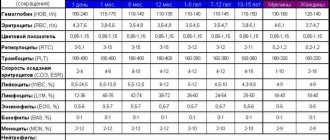
- A general blood test is one of the basic tests.
- The level of red blood cells and hemoglobin may be reduced (anemia) in patients with severe forms of protein deficiency and general exhaustion. A normal content of red blood cells with a low level of hemoglobin can be observed when it is insufficiently formed or excessively destroyed. This condition is called hypochromic anemia.
- Leukocytes. An increase in the number of leukocytes with the appearance of young cells in the leukocyte formula may indicate an infectious-inflammatory process that is the cause of protein deficiency.
- Erythrocyte sedimentation rate (ESR) is also an indicator that indicates an inflammatory process as the cause of protein deficiency.
- A general urine test is essential in excluding or confirming a renal cause of protein deficiency. Includes studying the following parameters.
- Urine color. Normally it is assessed as straw yellow. Red or brown discoloration may occur when blood enters the urine (hematuria) and indicates serious kidney problems. Dark brown urine, especially in combination with jaundice, is characteristic of liver disease.
- Transparency. Normal urine is clear. In case of kidney diseases, it becomes cloudy due to a significant content of pus (pyuria) or salts.
- The specific gravity of urine is an indicator of the efficiency of the kidneys. With protein deficiency caused by kidney damage, it can decrease significantly.
- Protein is normally absent in a urine test. If the test is positive (proteinuria), a quantitative determination of protein in the urine is carried out and its composition is necessarily examined. Albumin is the most commonly detected type of protein, but other proteins may also be detected, such as immunoglobulins, hemoglobin, myoglobin, and others. The degree of proteinuria allows us to indirectly judge the level and severity of kidney damage.
- Urine testing using special test strips is carried out to detect proteinuria - the release of protein in the urine. A positive result may be the first indication of a renal origin of protein deficiency. In this case, microscopy of the sediment is necessary. Urine sediment examination:
- Red blood cells - erythrocytes of protein deficiency caused by kidney pathology, can be present in the urine in large quantities. The presence of altered discolored red blood cells allows one to suspect glomerular damage (glomerulonephritis).
- Cylinders are formed in the renal tubules from protein, leukocytes, erythrocytes, and epithelium. Identification of casts, especially protein casts, may indicate a renal origin of protein deficiency.
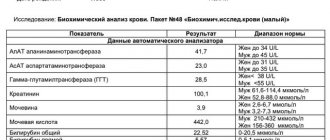
- Protein in blood serum. The study is the “gold standard” for studying protein metabolism and confirming protein deficiency. Protein levels in blood plasma and tissues are in a state of equilibrium. With the loss of tissue protein, the level of plasma proteins also decreases, which determines the significance of this parameter.
- Protein fractions of blood serum. Determination of the quantitative composition and ratio of protein types in blood serum. Total serum protein is represented by albumins and globulins, which perform various functions. The main part is albumin, the main building protein of the body. Fluctuations in its level to the greatest extent reflect the state of protein metabolism. Globulins are more specific in their purpose. These are proteins of the defense system, markers of inflammatory reactions and special transport proteins. Under various pathological conditions, the ratio and amount of proteins of one type or another can change significantly, and in some cases additional (pathological) protein fractions appear. Based on the ratio of individual fractions of the protein composition of the blood, one can to some extent judge the cause of protein deficiency. For example, if the liver and kidneys are damaged, albumin levels may decrease. Globulins increase during inflammatory processes, reflecting the activity of inflammation or the immune (protective) system. A decrease in globulin levels may indicate diseases of the renal tubules, and can also be observed with impaired liver function and when the body’s immune system is suppressed (as in severe forms of sepsis).
- Glucose (blood sugar). Determination of glucose levels may be prescribed if protein deficiency due to diabetes is suspected. Kidney damage in diabetes mellitus (diabetic nephropathy), as well as increased protein breakdown, can cause protein deficiency.
- Urea and creatinine in blood serum. These are substances formed during the breakdown of proteins. With intensive protein destruction, their level in the blood may increase. The indicator should be assessed together with the level of urea in daily urine.
- Urea in daily urine reflects the efficiency of the kidneys. With intensive protein breakdown, it can increase significantly. A low level of urea in the urine with an increase in it in the blood is more typical of renal failure.
- Creatinine in daily urine is an indicator of impaired excretory capacity of the kidneys, which is indicated by a decrease in its level. For a more accurate assessment, creatinine clearance is calculated, which is the ratio of its levels in daily urine and blood. In renal forms of protein deficiency, this indicator can decrease significantly.
- Coprogram is a stool examination that allows you to identify possible violations of the main stages of digestion. The chemical composition of feces, their color, smell, consistency are assessed, and certain types of microorganisms (dysbacteriosis) are identified. The analysis allows you to evaluate the activity of the main enzymes of the liver, gastric and intestinal juice, and pancreas. With protein deficiency caused by impaired protein absorption, undigested muscle fibers may be found in the stool.
Additional (instrumental) research methods
The scope of diagnostic tests depends on the suspected cause of protein deficiency and should be determined by the attending physician. The main diagnostic methods include:
- Ultrasound examination of the abdominal organs. A doctor may prescribe it to rule out diseases of the liver and pancreas, as well as kidneys. it combines high information content and safety for the patient. Ultrasound passes through soft tissue to the organ being examined and, after being reflected, returns back. The resulting image is transmitted to the monitor. The study allows you to assess the size of internal organs, the structure of their tissues, identify a tumor lesion or cyst, and exclude the presence of fluid in the abdominal cavity. If necessary, the study can be supplemented with an ultrasound-guided biopsy.
- Esophagogastroduodenoscopy. It is a direct examination of the esophagus, stomach and duodenum. The patency of the upper digestive tract, the condition of the mucous membrane, the degree of its inflammation or atrophy are assessed. During the examination, a piece of tissue may be taken for analysis (biopsy). Along with ultrasound, gastroscopy is mandatory if a nutritional protein deficiency is suspected.
- Daily pH measurements. This is the study of daily fluctuations in the acidity of gastric juice. A probe with a sensor at its end is placed in the stomach, and the information coming from it is recorded by a portable device attached to the patient's belt. The main part of the protein supplied with food is digested in the stomach under the influence of hydrochloric acid and pepsin, an enzyme that breaks down protein. If the acidity of gastric juice is reduced, protein digestion may be impaired.
- Enteroscopy (intestinoscopy). Examination of the small intestine. The study is similar in its capabilities to gastroscopy, but is technically more complex, since it involves examining the entire small intestine. Allows you to assess the condition of the mucous membrane, exclude erosive lesions and take the contents for analysis to exclude an infectious process.
- Colonoscopy is an examination of the large intestine. For protein deficiency, it can be prescribed to patients with suspected intestinal tumors or ulcerative colitis, in which significant protein loss is likely.
Treatment
Treatment of protein deficiency is aimed at replenishing protein volume and normalizing protein metabolism. At the same time, the underlying disease is treated.
It may include the following items.
- Recommendations for a balanced or protein-enriched diet (with sufficient animal protein). Including meat, eggs, fish, caviar in the diet. For patients with protein deficiency caused by kidney disease, liver disease, or diabetes mellitus, the diet should be selected by the attending physician, taking into account the characteristics of the course of the underlying disease. Such a correction of the diet may be the only necessary measure in case of a mild form of protein deficiency.
- Medications:
- solutions containing a complex of amino acids or protein components of blood intended for intravenous administration; treatment with these drugs is carried out under the strict supervision of a doctor in a hospital setting;
- special nutritional mixtures can be prescribed to patients with severe forms of protein deficiency due to diseases of the gastrointestinal tract or in the postoperative period; these are special protein cocktails that are introduced into the stomach or duodenum through a tube when normal nutrition is impossible;
- Digestive enzymes are used for replacement purposes by patients who do not produce enough of them.
Prevention
- A balanced diet with sufficient amounts of plant and animal proteins.
- Mandatory medical supervision during a diet that strictly limits the diet, or during courses of therapeutic fasting.
- Timely detection and treatment of diseases that increase the risk of developing white deficiency.
Recommended tests
- General blood analysis
- Leukocyte formula
- Erythrocyte sedimentation rate (ESR)
- General urine analysis with microscopy
- Rehberg test (endogenous creatinine clearance)
- Urea in daily urine
- Creatinine in daily urine
- Total protein in urine
- Total protein in whey
- Protein fractions in whey
- Serum creatinine
- Urea in serum
- Plasma glucose
- Coprogram
Risk factors
- Low standard of living;
- Vegetarian food;
- Following a mono-diet or fasting for the purpose of losing weight;
- Kidney diseases;
- Diseases of the digestive system;
- Hereditary factor;
- Occupation-related weight deficiency;
- Age 60+.
For children, the following risk factors should be considered:
- Prematurity;
- Intrauterine hyposkia;
- Use of alcoholic beverages and drugs by a pregnant woman.
Ascites in liver cirrhosis
Symptomatic manifestations of hypoproteinemia
A drop in protein levels is not characterized by clear specific symptoms. Somatic and external manifestations of low protein in the blood depend on the disorders and diseases that provoked changes in blood composition. With a slight loss of proteins, weakness, decreased physical capabilities, and CFS (chronic fatigue syndrome) are observed.
With a more serious decrease in indicators, the following manifestations are added:
- dysania (sleep disorder), apathy, irritability;
- unstable functioning of the digestive and urinary system;
- frequent ARVI and colds;
- labored breathing;
- suppression of libido (sexual desire);
- hypertensive symptoms (increased blood pressure, headache).
An external sign is swelling (accumulation of excess fluid in the extracellular space). Edema occurs due to a violation of the stable level of colloid-osmotic and hydrostatic pressure on the walls of blood vessels, since an insufficient number of protein molecules cannot provide the necessary compression for the passage of water from the tissue fluid into the bloodstream.
A reduced level of protein inhibits the process of formation of new cells, therefore the processes of post-traumatic skin restoration are disrupted. Trying to make up for the lack of proteins, the body begins to pull them from muscle fibers, which leads to their destruction. The symptoms are:
- arthralgia – muscle pain not caused by physical stress or inflammatory processes;
- weight loss (due to muscle mass).
Lack of nutrients affects the health of hair and nails (brittleness, dryness, etc.). Hypoproteinemia can only be determined through a laboratory blood test. To do this, you need to donate blood for a biochemical analysis. Blood sampling is carried out free of charge upon referral from a doctor. You can undergo the procedure yourself for a fee at clinical diagnostic centers.
Symptoms
If the protein deficiency is mild, then it does not manifest itself symptomatically, except in cases of hereditary deficiencies of certain amino acids, which are structural components of protein molecules.
External symptoms include:
- Continuous weight loss;
- Brittle nails;
- Brittle, dull and falling hair;
- Edema;
- Dryness, flaking of the skin;
- Weakness.
Nervous system symptoms:
- Migraine;
- Mood swings;
- Lethargy, fatigue;
- Sleep problems;
- Low mental activity.
Symptoms of the musculoskeletal system:
- Muscle weakness;
- Slow growth in children;
- Decreased muscle mass;
- Pain syndrome in muscles and joints.
Digestive organ symptoms:
- Nausea;
- Bloating, pain;
- Increased consumption of sweets;
- Problems with stool;
- Enlarged liver.
Call us
+7
Increased total protein: what does it mean?
This situation is rare, and yet it does occur. The first reason for this condition may be dehydration, but this problem is quite easy to deal with. The second reason is more serious – blood cancer. In this case, lymphocytes overproduce an abnormal amount of immunoglobulin, which no longer has a useful function, but quantitatively affects the value of the total protein.
Get tested for total blood protein in Moscow at the Meditsina clinic
A blood test for total protein is used to diagnose a huge number of diseases of almost all organs and systems. You can donate it at the Meditsina clinic, located in the Moscow ZAO area. We have our own laboratory, where a wide variety of analyzes of biological material are carried out using modern equipment.
In addition, our clinic employs qualified doctors who correctly interpret test results and prescribe effective treatment if necessary.
Here you will also find affordable prices for medical services - check out the price list to find out how much a particular test costs. You can make an appointment with a doctor, as well as tests, by phone or online.
Treatment
The minimum protein intake for an oncology patient should be at least one and a half grams per kilogram of body weight. For patients with renal failure - no more than 1.2 grams.
Since protein deficiency in a patient with cancer occurs due to inadequate intake or loss of proteins, for example, during the evacuation of water accumulations, it is impossible to reverse the pathological condition by increasing the volume of food.
In case of a loss of 5% of weight with an initial body mass index <20, a decrease in total plasma protein to 60 grams, globulin to 30 grams, and a balanced diet is impossible, it is urgent to start consuming specialized protein mixtures.
If the indicators are even worse or it is not possible to eat by mouth, tube or intravenous nutrition is necessary.
It is necessary to reduce the toxicity of treatment and symptomatic therapy. However, it is impossible to improve the quality of life and speed up the rehabilitation of a patient with cancer without high-quality nutritional support.
Diagnosis of protein deficiency
The simplest method for initial diagnosis is to determine in a biochemical blood test such an indicator as “total protein”.
In addition, it is necessary to establish the level
of albumin in the blood plasma
- as a rule, in conditions of insufficient supply of proteins from the outside, the liver compensatory increases the production of this fraction.
Since all enzymes, as previously mentioned, have a polypeptide basis, you can additionally rely on ALT and AST - they are often prescribed by nutritionists and doctors. However, here it is important to remember the no less dominant role in the functioning of these vitamin B6 enzymes and to be able to correctly differentiate the causes and factors of a decrease in these liver panel indicators.
An increase in the amino acid homocysteine indicates a violation of methylation processes.
in blood serum - in this case, you can suspect polymorphism in one or more genes that regulate the folate cycle and do a genetic test. A little higher, we said that these “breakdowns” are accompanied by an increase in the concentration of histamine due to a decrease in its neutralization - patients experience allergies, skin rashes and even bronchial asthma.
Low acidity is determined by pH testing
, which necessarily accompanies fibrogastroduodenoscopy with the collection of biopsy material - this is fundamentally important for establishing the stage of the process and preventing the future development of stomach cancer. The following laboratory tests will be indicative:
- Amino acids in urine (tendency to decrease).
- Reducing the concentration in the blood of metals absorbed in an acidic environment: selenium, manganese, zinc and magnesium.
Diagnosis of Helicobacter
, which is necessarily carried out in order to establish indications for the use of antibiotic therapy, consists of:
- Determination of bacterial antigens in feces.
- Breath tests with labeled urea.
- Determination of antibodies in the patient's blood.
- Biopsy during fibrogastroduodenoscopy followed by histological analysis.
To the gastropanel,
which is quite often prescribed to diagnose the condition of the gastric mucosa, includes, along with the other 3 biomarkers, such an indicator as
gastrin-17
- another stimulator of hydrochloric acid secretion, produced by the pyloric region of the stomach. Its decrease indicates a high probability of atrophic gastritis, an autoimmune disease accompanied by a decrease in the number of functioning epithelial cells.
About the condition of the gallbladder
, as a possible culprit for impaired activation of pancreatic enzymes (including proteolytic ones) is judged by:
- Coprogram.
- Biochemical blood test:
- ALT, AST.
- Gamma glutamyl transferase.
- Direct and indirect bilirubin.
- Total cholesterol.
- HDL, LDL (additionally - apoprotein B).
- alkaline phosphatase.
- Organic acids in urine (for the diagnosis of bacterial overgrowth syndrome).
An increase in the number of colonies of residents of our intestines is accompanied by an increase in the activity of fermentation processes and, as a consequence, excess gas production. This, in turn, complicates the secretion of pancreatic juice and bile due to increased pressure in the intestinal lumen.
- Ultrasound of the abdominal organs.
How to raise it?
In order for the body to function normally, the lack of protein in the blood must be replenished. First of all, you need to find out the causes of hypoproteinemia and eliminate them.
If low protein is caused by a disease, you need to see a doctor, get examined and find out the diagnosis. If treatment is effective, protein levels will return to normal.
Its content can be increased both with medications and proper nutrition. To increase it, a special diet and multivitamin complexes are prescribed.
You should know that not all proteins are broken down equally in the digestive system. Some of them are partially absorbed. Therefore, the diet should be developed by a nutritionist.
A nutritionist will help you create a nutrition plan for hypoproteinemia
How to avoid trouble?
In order to never encounter this problem (and this, unfortunately, is possible), you need to think about its prevention. That is, learn as much useful information as possible about your body and its needs for important nutrients.
Understand why it is necessary to adjust your diet based on your current state of health and metabolism, taking into account all diseases.
And not only rejoice at new knowledge, but also convey it to loved ones, create useful “word of mouth”, which, perhaps, will protect someone from a frivolous attitude to nutrition.
Causes of low blood protein
Low protein levels may be a sign of liver disease
In medical practice, such a pathology as a decrease in protein levels in the blood is called hypoproteinemia.
Its presence can signal some diseases and disorders occurring in the human body:
- hepatic cell failure, which developed against the background of acute and chronic liver pathologies
- improper and irrational nutrition in the absence of any pathologies affecting internal organs
- depletion of the human body, which is caused by long-term diseases and infectious-purulent inflammations
- various pathologies of pregnancy, for example, gestosis
- diseases of the endocrine system, that is, decreased thyroid function and hyperfunction of the adrenal glands
- HIV infection and various immunodeficiencies
- disruption of the pancreas with its enzymatic insufficiency
- diabetes mellitus with various complications
- severe form of anemia, malignant neoplasms and bleeding;
- accelerated excretion of protein from the body along with urine in severe kidney diseases and renal failure
- pathologies of the stomach and intestines in a chronic form, which are accompanied by disruption of the digestion process and absorption of protein components from food
A symptomatic decrease in the level of total protein in the human body can be expressed in the formation of tissue edema. Typically, this symptom is observed with a significant decrease in total protein, that is, below 50 g/l.
A decrease in protein concentration in the blood is always considered a dangerous signal, which indicates various pathological changes. The human body, which is in this state, becomes completely defenseless to the effects of various unfavorable factors and is not able to recover on its own.
Why is this happening?
We have found that without adequate protein in our diet, we face serious health problems. But you also need to know about the reasons why protein-energy deficiency occurs, and there are two of them.
The first reason is external, or exogenous, which is caused by systematic malnutrition (for example, if you chose a strict fasting method to lose weight). Also, an external cause may be difficulties in the functioning of the masticatory apparatus, interfering with normal food intake, or diseases in the field of neuralgia or the psyche.
The second reason is internal, or endogenous, and here problems with digestion and assimilation of food, the existing increased needs for nutrients and, accordingly, energy come to the fore (this happens with lung pathology, surgical interventions, radiation and chemotherapy). Congenital and acquired metabolic problems cannot be discounted.
Diet
Proteins necessary for the body to function normally are found in both animal and plant foods. It is known that animals are digested better due to their composition. Doctors say that a person needs both. Proteins contain amino acids, and each of them is needed by the body, so it is important to eat both animal and plant proteins.
Foods high in animal protein include:
- low-fat cottage cheese;
- cheeses;
- egg powder;
- meat (veal, beef);
- poultry meat;
- fish;
- seafood (squid, shrimp).
The diet should include foods containing not only animal, but also plant proteins.
Plant-based foods that are high in protein include:
- peanut;
- dried apricots;
- beans;
- almond;
- walnuts;
- lentils;
- cereals;
- rye;
- chocolate (cocoa 70%);
- soy;
- seaweed;
- sprouted wheat grains;
- brown rice;
- bran bread;
- pasta made from wholemeal flour.
Foods containing an average amount of protein are:
- fat meat;
- fatty cottage cheese;
- full fat milk;
- chicken eggs.
Such foods will undoubtedly increase protein in the blood
The menu should include foods that do not contain a lot of protein, but are necessary to increase its level in the blood:
- vegetables,
- berries,
- mushrooms,
- fruits.
Some categories of people need to consume twice as much protein per day. These include:
- pregnant women;
- nursing mothers;
- persons engaged in heavy physical labor;
- athletes.