Why is cholesterol dangerous?
Your doctor has probably warned you about cholesterol, a fatty, waxy substance that circulates in your blood. Too much of the wrong type of cholesterol can clog your arteries and put you at risk for heart disease.
High cholesterol may be a result of your diet, especially if you eat foods high in saturated fat, such as red meat and butter. Sometimes, however, your thyroid gland may be to blame. Too much or too little thyroid hormone can cause cholesterol levels to rise or fall.
In this article, you will learn how your thyroid gland affects cholesterol.
What to eat for hypothyroidism?
So what should you eat if you have hypothyroidism? Fish is an excellent source of iodine in the diet. Most of this element contains cod (100 mcg of iodine per 100 g), salmon (50 mcg / 100 g) and mackerel (45 mcg / 100 g). Iodine is also present in mineral water, but not in all its types, so you should keep an eye on the label when looking for this element.
Table salt is also a source of iodine, as many countries have passed legislation requiring salt manufacturers to iodize table salt. Selenium, in turn, is found in grain products, meat, fish, dairy products, eggs and vegetable sprouts.
Iodized table salt
In general, the diet for hypothyroidism should be properly balanced. Healthy protein should make up 15% of your daily energy needs, complex carbohydrates 55%, and fats 30% (with 20% unsaturated fatty acids and a maximum of 10% saturated fats).
Dietary fiber should be an important part of the diet because constipation is very common in patients suffering from hypothyroidism. It is recommended to consume 25-40 grams of dietary fiber per day.
What is the thyroid gland?
Your thyroid gland is a butterfly-shaped gland in your neck. It produces hormones that control metabolism. Metabolism is the process by which your body converts food and oxygen into energy. Thyroid hormones also help the heart, brain, and other organs function normally.
At the base of the brain is the pituitary gland, which directs the activity of the thyroid gland. When your pituitary gland detects that you have low thyroid hormone levels, it releases thyroid-stimulating hormone (TSH). TSH directs the thyroid gland to produce more hormones.
Hypothyroidism and autoimmune processes are the leading link in the development of pathology
- Authors: Butolina L.N., Pshenichnaya N.K.
Thyroid diseases are one of the most common forms of human pathology.
In recent years, in many regions of Russia there has been a significant increase in the incidence of thyroid diseases, which is associated with deteriorating environmental conditions, insufficient iodine intake, negative changes in the population’s diet, and an increase in the incidence of autoimmune diseases. Hypothyroidism occupies one of the leading places in the structure of thyroid pathology in terms of frequency and social significance. Hypothyroidism occurs in approximately 2-3% of the total population and is caused by low levels of one or two thyroid hormones in the blood. Hypothyroidism may be associated with a primary lesion of the thyroid gland itself (primary hypothyroidism), a violation of the regulation of its function by the hypothalamic-pituitary system (secondary and tertiary hypothyroidism). In the vast majority of cases (90-95%), hypothyroidism is caused by a pathological process in the thyroid gland, which reduces the level of hormone production (primary hypothyroidism). One of these processes is the development of hypothyroidism due to autoimmune thyroiditis, and it is this slowly and latently developing hypothyroidism that poses the greatest problem for identification.
Other common causes of hypothyroidism (about 1/3 of cases) are operations on the thyroid gland, which can be performed for various diseases (toxic goiter, multinodular and nodular goiter, thyroid tumors, etc.), as well as therapy with radioactive iodine. The cause of hypothyroidism in these cases is obvious - in the first, the thyroid gland is surgically removed, and in the second, it is subjected to radiation destruction. In both cases, identifying hypothyroidism does not present serious difficulties, since it develops shortly after treatment and is actively monitored by doctors.
With hypothyroidism, all metabolic processes in the body are disrupted. Cardiac activity, the functioning of the nervous system, stomach, intestines, kidneys, liver and reproductive system are disrupted. Hypothyroidism can manifest itself as a disruption in the functioning of any organ and system. Common symptoms are weakness, fatigue, weight gain, chilliness (the feeling of being cold all the time), decreased appetite, swelling and fluid retention, hoarseness, muscle cramps, dry skin and the appearance of a slight jaundiced tint, increased hair fragility, anemia.
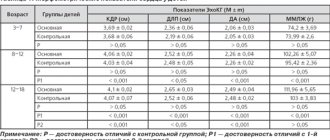
Laboratory diagnosis of hypothyroidism, according to many endocrinologists, is the determination of free thyroxine (free T4) and thyroid-stimulating hormone (TSH) in the blood serum, which is the best combination of tests for diagnosing hypothyroidism. In hypothyroidism, the basal TSH level is increased due to primary damage to the thyroid gland (primary hypothyroidism) and decreased due to primary failure of the pituitary gland (secondary hypothyroidism) or hypothalamus (tertiary hypothyroidism). An increase in TSH levels in the blood is the earliest laboratory sign of thyroid insufficiency. An increase in TSH levels predicts a decrease in free T4. When free T4 decreases by half, TSH secretion will increase 100 times. In this regard, TSH testing is a much more sensitive indicator for detecting minimal thyroid insufficiency (Table 1).
Table 1. Four stages of hypothyroidism development
| Stages | St. T4 | TSH (mIU/l) |
| First | Norm | Within normal limits |
| Second | Norm | High (5-10) |
| Third | Norm | High (more than 10) |
| Fourth | Short | High (more than 10) |
In diseases of the thyroid gland of autoimmune origin, the leading role in the pathological process belongs to antibodies produced by human B lymphocytes to various components (antigens) of the thyroid cell. Autoimmune aggression against the thyroid gland can be accompanied not only by a change in the functional state of thyrocytes but also by their death, leading to loss of gland tissue and the development of hypothyroidism.
The level of TSH and antibodies to thyroid peroxidase in the blood serum are indicators for assessing the manifestation of hypothyroidism, which progresses in parallel with the overproduction of TSH. The presence of an increase in only TSH or only antibodies determines a lower, but significantly increased risk of pathology.
The laboratory of the CDC "Health" is equipped with modern equipment: immunochemiluminescent machines "LIASON" (Germany) and "ARHITETECT" (USA) allow performing tests with a high degree of specificity, accuracy and reliability, such as: determining the level of thyroid-stimulating hormone and free thyroxine in the blood serum , free triiodothyronine (free T3), thyroglobulin (TG), autoantibodies to thyroglobulin (Ab to TG) and thyrocyte peroxidase (Ab to TPO), antibodies to TSH receptors.
Many clinicians recommend screening patients to identify thyroid pathology, prescribing them a test for TSH and free T4. However, our many years of experience in working as a diagnostic laboratory show that, as a rule, screening is not enough to reliably detect the presence of thyroid pathology in examined patients. First of all, because a screening examination is considered to be the examination of a large number of apparently healthy individuals who have contacted specialists regarding a particular ailment.
1072 people were examined and underwent tests of TSH, fT3, fT4, Ab to TG and Ab to TPO. For comparison, we took patients diagnosed with autoimmune thyroiditis and specified hypothyroidism, in whom the above indicators were normal, elevated and below normal (Table 2).
Table 2. Distribution of patients diagnosed with AIT and specified hypothyroidism depending on the value of the main and additional tests
| Autoimmune thyroiditis | Test values are normal | % | Test values are higher than normal | % | Test values below normal | % |
| At to TG | 288 | 74 | 99 | 25 | 2 | 0,5 |
| At to TPO | 349 | 66 | 178 | 34 | 1 | 0,2 |
| SvT3 | 198 | 87 | 22 | 9,7 | 7 | |
| SvT4 | 989 | 92 | 42 | 3,92 | 41 | 3,8 |
| TSH | 758 | 73 | 202 | 19,5 | 74 | 7,2 |
| Other specified hypothyroidisms | Test values are normal | % | Test values are higher than normal | % | Test values below normal | % |
| At to TG | 58 | 63 | 32 | 35 | 2 | 2,2 |
| At to TPO | 35 | 53 | 31 | 47 | — | — |
| SvT3 | 47 | 94 | 2 | 4 | 1 | 2 |
| SvT4 | 100 | 90 | 6 | 5,4 | 5 | 4,5 |
| TSH | 78 | 64 | 24 | 19,8 | 19 | 15,7 |
Having considered the results of examination of patients, with a diagnosis of AIT, in the group of patients with elevated levels of tests, Ab to TG and Ab to TPO, the percentage ratio was: 25% and 34% and TSH, f.T4, f.T3: 19.5%, 3. 92%, 9.7% respectively. (Table 2, Histogram 1)
Histogram 1. Structure of test distribution in percentage terms for AIT
The results of examination of patients, with a diagnosis, specified hypothyroidism in the group of patients with elevated test levels, Ab to TG and Ab to TPO: 35% and 47%, TSH, f.T4, f.T3 19.8%, 5.4%, 4%, we see a significant increase in test scores related to autoimmune pathology. Determination of antibodies to thyroglobulin and thyroid peroxidase provides more complete information for monitoring the stage of treatment of patients (histograms 1 and 2).
Histogram 2. Structure of distribution of tests in percentage terms for specified hypothyroidism
Thus, we once again confirmed the predominance of autoimmune processes underlying the development of hypothyroidism and other thyroid diseases.
Based on the above tables and histograms, we can conclude that screening alone is not enough to identify thyroid pathology. A detailed analysis including, in addition to the main tests (TSH and free T4), an additional study of antibodies to thyroglobulin and thyroid peroxidase allows us to determine the functional state and monitor the treatment of pathologies such as hypothyroidism.
Literature.
- I.M. Skudarnova, N.V. Soboleva, N.V. Mychka. Thyroid hormones: a manual for doctors/ /Vector Best JSC-Koltsovo: 2006 p. 17., 25., 28.
- N. U. Tits Clinical evaluation of laboratory tests: Medicine, 1986. p. 146.
- A. A. Kishkun Hormonal and genetic studies in clinical practice // Moscow 2007. p. 68
- Vetshev P.S., G.A.Melnichenko, N.S.Kuznetsov and others. Diseases of the thyroid gland. M, 1995. p. 36
About cholesterol
Cholesterol is found in every cell of your body. Your body uses it to produce hormones and substances that help digest food.
Cholesterol also circulates in your blood. It enters the bloodstream in two forms of lipoproteins:
- High-density lipoprotein (HDL) cholesterol is good for your heart. They help remove cholesterol from the body and protect against heart disease.
- Low-density lipoprotein (LDL) cholesterol is bad for your heart. If LDL cholesterol levels are too high, the cholesterol can clog arteries and contribute to heart disease, heart attacks and strokes.
Underactive or overactive thyroid
Sometimes the thyroid gland can produce too little or too much hormone.
A condition in which the thyroid gland does not work effectively is called hypothyroidism. When the thyroid gland is weakened, the entire body feels that it is working slowly. You become tired, lethargic, cold and sore.
An underactive thyroid may develop if you have the following conditions:
- Hashimoto's thyroiditis, an autoimmune disease in which the body attacks and destroys the thyroid gland
- inflammation of the thyroid gland (thyroiditis)
Other factors that can lead to underactive thyroid:
- removal of all or part of the overactive thyroid gland
- radiation for cancer or an overactive thyroid gland
- some medications such as lithium, interferon alpha, and interleukin-2
- damage to the pituitary gland from a tumor, radiation, or surgery
Hyperthyroidism is a condition that occurs when the thyroid gland is overactive. When the thyroid gland is overactive, the body begins to work faster. Your heart rate increases, and you feel nervous and trembling.
Hyperthyroidism may develop if you have:
- Graves' disease, an immune system disorder that runs in families
- toxic nodular goiter, which includes lumps or nodules on the thyroid gland
- inflammation of the thyroid gland (thyroiditis)
How does the thyroid gland cause cholesterol problems?
Your body needs thyroid hormones to make cholesterol and get rid of cholesterol it doesn't need. When thyroid hormone levels are low (hypothyroidism), the body does not break down and remove LDL cholesterol as efficiently as usual. LDL cholesterol can build up in the blood.
Thyroid hormone levels do not have to be very low to raise cholesterol levels. Even people with moderately low thyroid levels, called subclinical hypothyroidism, may have higher LDL cholesterol levels than normal. A 2012 study found that high TSH levels alone can directly increase cholesterol levels, even if thyroid hormone levels are not low.
Hyperthyroidism has the opposite effect on cholesterol levels. It causes cholesterol levels to drop to abnormally low levels.
Complexes with this research
Examination during pregnancy.
1st trimester 9,770 ₽ Composition Blood biochemistry. 19 indicators Advanced biochemical blood test 3,420 ₽ Composition
Women's check-up No. 1 38 studies for annual preventive examination 11,530 ₽ Composition
IN OTHER COMPLEXES
- Joining IVF RUB 14,350
- Preventive check-up RUB 6,530
- Examination during pregnancy. 3rd trimester 5,360 RUR
- Check-up No. 1 for children and teenagers 6,390 RUR
- Diabetes monitoring RUB 1,900
What are the symptoms?
You may have an underactive thyroid gland if you notice the following symptoms:
- weight gain
- slow heartbeat
- increased sensitivity to cold
- muscle pain and weakness
- dry skin
- constipation
- problems remembering or concentrating
An overactive thyroid gland has exactly the opposite symptoms:
- weight loss
- fast heartbeat
- increased sensitivity to heat
- increased appetite
- nervousness
- shake
- more frequent bowel movements
- sleep problems
Symptoms of hypothyroidism
The symptoms of hypothyroidism are varied because, like many endocrine diseases, it affects almost all organ systems.
Classic symptoms include
:
- drowsiness, apathy, increased fatigue
- chilliness, poor cold tolerance
- dry skin and hair (criterion for dry hair - you can not wash your hair for 2 weeks, and your hair does not seem greasy)
- constipation
- weight gain
- slow heartbeat
- elevated blood cholesterol levels
- Irregularity of the menstrual cycle and infertility in women
- sexual dysfunction in men
But not every patient necessarily has the full range of symptoms. In some cases, even manifest hypothyroidism (with corresponding changes in hormone levels) may not be felt by the patient.