Sign up
+7
Pericarditis is a heart disease manifested by an inflammatory process localized in the serous membrane of the organ. Acute pericarditis is an inflammatory syndrome with or without pericardial effusion (effusion). The diagnosis of subacute pericarditis is established when its duration is from 4-6 weeks to 3 months without remission. Recurrent pericarditis is diagnosed after a documented first episode of acute pericarditis and a symptom-free period of 4-6 weeks or longer (usually about 18-24 months).
Chronic pericarditis lasts longer than 3 months without remission. It can develop in various forms - asymptomatic, effusion, with lime deposits - the so-called “shell heart”, constrictive.
In whatever form the disease manifests itself - constrictive, effusion, etc. – it requires quick diagnosis and proper effective treatment.
Make an appointment with a specialist without queues, at a convenient time
Sign up
+7
Reasons for the development of the disease
This cardiac disease has a polyetiological nature:
- Infectious causes include rheumatic, tuberculous, bacterial. In addition, pericarditis can have a fungal or viral etiology, for example, with influenza.
- Aseptic reasons include allergies, diffuse connective tissue diseases, hematological diseases, malignant processes, injuries, radiation exposure, hypovitaminosis.
- Idiopathic pericarditis may also develop, the cause of which cannot be determined. It is these pathologies that are most often prone to relapse.
Prevention
Preventive measures that reduce the possibility of developing constrictive pericarditis are based on preventing the causes that most often cause the pathology. Prevention includes:
- Healthy lifestyle, giving up bad habits.
- Avoiding injury (especially to the chest).
- Timely and thorough treatment of infectious diseases.
At the first symptoms of constrictive pericarditis, you must immediately contact a medical facility, since each missed day in the future may result in more complex treatment and even result in lost years of life.
Symptoms
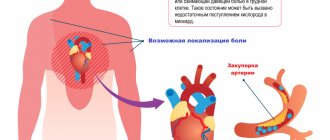
Pain syndrome in acute pericarditis can be characterized by varying intensity. This can range from a slight tingling sensation when turning or bending sharply, to severe, all-consuming pain, like a heart attack. The pain may become stronger when sneezing, coughing, or deep breathing. There may be a sensation of radiating to the shoulder, neck, or shoulder blade.
In addition to pain, accompanying symptoms are: shortness of breath, mild headache or dizziness, and a slight increase in body temperature. Despite the fact that this symptomatology is quite “common,” it is extremely important to carry out a differential diagnosis and accurately determine the presence of pericarditis. Thus, acute pericarditis can be diagnosed if at least 2 of the following 4 signs are present:
- Pericardial chest pain.
- Pericardial murmur.
- The ECG interpretation shows signs of pericarditis.
- Pericardial effusion (formed or increased compared to the previous volume).
Additional signs: signs of an inflammatory process in the pericardium during imaging methods (computed tomography - CT, magnetic resonance imaging - MRI, ultrasound examination of the heart).
- Available: doctor’s appointment from 1500 rubles
- Convenient: open daily from 8:00 to 21:00
- Quickly: we will carry out all the diagnostics at the first appointment
- Complete: has all the necessary equipment
Pericarditis
Pericarditis is an inflammatory disease of the tissue lining of the heart (pericardium), of an infectious or non-infectious nature.
The pericardium consists of outer and inner layers, between which normally there is a small amount of fluid. Fluid is needed to ease friction during contraction of the heart muscle. Pericarditis can act as an independent isolated disease or be a complication of diseases of other organs and systems.
Causes of pericarditis development
- infectious (bacteria, viruses, fungi, protozoa, etc.),
- non-infectious (allergic diseases, systemic connective tissue diseases, some blood diseases, metabolic disorders, injuries, exposure to radiation, treatment with certain hormonal drugs, cancer).
There are idiopathic pericarditis (cases of pericarditis where the cause of inflammation cannot be determined). In the development of pericarditis, changes in the composition or amount of pericardial fluid under the influence of the above factors play an important role.
Symptoms of pericarditis Symptoms of pericarditis are cardiac and general, the degree and severity of symptoms depend on the form and stage of the disease. The main cardiac symptom is heart pain, felt in 90% of cases. The pain is usually localized behind the sternum or in the left half of the chest, and can radiate to the left arm. The intensity of pain varies: from almost imperceptible to extremely acute, heart attack-like. The nature and intensity of pain varies depending on the position of the body. The pain decreases when lying on the right side with the legs pulled up to the chest, or when bending forward. This happens because in this position, when the heart contracts, the inflamed walls of the heart sac come into less contact. The pain intensifies when coughing, taking a deep breath, or lying on your back. With some types of pericarditis there may be no pain at all. Another common symptom is the appearance of circulatory failure (shortness of breath on exertion and at rest, edema). Common symptoms include:
- weakness;
- sweating;
- fatigue, lack of or decreased appetite;
- elevated temperature.
If pericarditis has developed as a complication of another disease, symptoms of damage to other organs and systems may be present in the foreground.
Types and forms of pericarditis
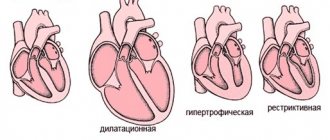
- Acute pericarditis – up to 1-2 months from the onset of the disease. Types of acute pericarditis: exudative (effusive), fibrinous (dry).
- Subacute pericarditis – from 2 to 6 months from the onset of the disease. Types of subacute pericarditis: exudative (effusion); adhesive (sticky); constrictive (squeezing).
- Chronic pericarditis – more than 6 months from the onset of the disease. Types of chronic pericarditis: exudative (effusion); adhesive (sticky); constrictive (squeezing); compressive pericarditis with calcification (“shell heart”).
Exudative pericarditis. As a result of the inflammatory process, a large amount of fluid accumulates in the pericardial cavity. The fluid may contain various cellular elements and substances, depending on their presence, exudative pericarditis is divided into several subtypes (purulent, hemorrhagic, uremic, etc.). If the effusion accumulates very quickly, the outer layer of the pericardium does not have time to stretch, compression of the heart chambers occurs, cardiac output drops sharply, and acute cardiovascular failure develops. This process is called cardiac tamponade. Cardiac tamponade is a life-threatening condition that requires emergency hospitalization and treatment. If fluid accumulates slowly in the pericardial cavity, the outer layer of the pericardium has time to stretch, without compression of the walls of the heart and disruption of its functioning. More than 1 liter of fluid can accumulate in the pericardial cavity. An enlarged cardiac sac sometimes interferes with the normal functioning of nearby organs (esophagus, trachea, lungs, recurrent nerve), which is manifested by swallowing disorders, cough, hoarseness and other symptoms.
Fibrinous pericarditis. Fluid (inflammatory effusion) containing fibrinogen forms in the pericardial cavity. Some of the fluid is sucked out through the lymphatic vessels, but fibrin fibers settle on the leaves of the cardiac sac, limiting their movement.
Adhesive pericarditis. With adhesive pericarditis, as a result of the inflammatory process, connective tissue grows on the pericardial layers, forming adhesions.
Constrictive pericarditis. With constrictive pericarditis, as a result of the inflammatory process, the entire cavity of the heart sac is filled with scar tissue, causing compression of the heart chambers and impairing the function of the heart.
Compressive pericarditis with calcification (“shell heart”). With an “armored” heart, as a result of the inflammatory process, the pericardial layers become denser, welded together, and calcium is deposited in them. A rigid and inactive cardiac sac disrupts the functioning of the heart.
Diagnosis and treatment of pericarditis Pericarditis is a very “cunning” disease, due to its non-specific, in the eyes of a layman, symptoms and “disguise” as some other diseases.
If pericarditis is suspected, consultation with a cardiologist is mandatory. With asymptomatic or minimally symptomatic pericarditis, diagnosing the disease is difficult. The key to correct and effective treatment is high-quality diagnostics. It is very important to carry out all the necessary research as quickly as possible. You may need:
- blood test (clinical, biochemical, immunological) – whether there are signs of inflammation in the blood;
- ECHO KG (ultrasound of the heart) - the amount of fluid in the pericardial cavity is visible;
- ECG;
- radiography;
- CT scan of the chest;
- in some cases, diagnostic puncture or biopsy of the pericardium.
Additional tests are often prescribed to clarify the causes of pericarditis. Only an experienced doctor can correctly interpret the examination results and develop a treatment regimen. With proper, timely treatment, the prognosis is usually favorable. Treatment methods for pericarditis are very different and depend on its nature, course, and concomitant diseases. Treatment can be either medicinal or surgical (pericardial puncture, pericardial biopsy, surgical treatment of scars).
Types of disease
The clinical picture and course of the disease depends on the underlying disease.
- Nonspecific pericarditis is often accompanied by frequent relapses. The most common cause of its occurrence is complications after viral infections or radiation. Occurs after a viral infection of the upper respiratory tract, insolation. Without timely treatment, it can develop into an exudative or constrictive form.
- With purulent pericarditis, hardware or puncture examination reveals a moderate accumulation of pus in the heart sac.
- Rheumatic pericarditis is a sign of active rheumatism and often occurs against the background of inflammation of the walls of the heart - rheumatic carditis.
- Metastatic pericarditis may be the first sign of lung or breast cancer. A primary pericardial tumor that also causes pericarditis, mesothelioma, is rare.
Causes and risk factors
The risk of pericarditis progressing to constriction depends greatly on the cause of the disease. The risk of developing constriction is high, about 20-30%, with bacterial, especially purulent inflammation of the pericardium.
Constrictive pericarditis rarely occurs with the following pericarditis:
- viral;
- idiopathic;
- neoplastic (tumor nature);
- immune-mediated.
Risk factors
Risk factors also include certain categories of people:
- HIV-infected;
- patients with tuberculosis;
- suffered chest injuries;
- those who have undergone heart surgery;
- undergoing radiation therapy in the chest area.
Treatment
Most patients with acute pericarditis have a good long-term prognosis.
- Anti-inflammatory drugs.
- Immunosuppressive and biological therapy.
- Glucocorticoids.
- Diuretics - for large amounts of effusion.
Treatment will be different for pericarditis of different etiologies. Bacterial pericarditis is treated with antibiotics. If the pathology has a tumor cause, then cytostatics are used; uremic pericarditis requires hemodialysis. In difficult cases, surgery may be required to remove part of the pericardium.
Prices for services
| Name | Time | Price | |
| Appointment with a cardiologist, treatment and diagnostic, primary, outpatient | 1500 | ||
| Treatment and diagnostic appointment with a cardiologist, repeated, outpatient | 1000 | ||
| Preventive, outpatient appointment with a cardiologist | 550 | ||
| Holter ECG recorder with Holter data decoding | 3250 | ||
| Comprehensive consultation with a cardiologist ECG with interpretation + Echo-kg | 3650 | ||
| Call a doctor to your home (Khimki, Starbeevo, Ivakino, Naberezhnye) | 15000 | ||
| Calling a doctor to your home (Skhodnya, Podrezkovo, Novopodrezkovo, Planernaya station, Firsanovka) | 15000 | ||
| Call a doctor to your home (Kurkino, Novogorsk) | 15000 | ||
| Call a doctor to your home (Left Bank, Moscow, within the Moscow Ring Road) | 15000 | ||
| MRI of the thoracic spine. | 4500 | ||
| Medical consultation | 3300 | ||
| Extract from outpatient card | 660 | ||
| Consultation (interpretation) with analyzes from third parties | 1300 | ||
| Consultation on treatment adjustments | 550 | ||
| Repeated reception of CMN | 1600 | ||
| Initial reception of CMN | 2000 | ||
| Express test for determining the level of Troponin in the blood. | 1900 | ||
| Expand all prices | |||
Forecast
Constrictive pericarditis is a very serious complication with a rather unfavorable prognosis, which only worsens over time. Pericardiectomy is the only method of treating this pathology, however, it does not provide a complete guarantee of cure. Disappearance of symptoms is observed in only 60% of patients. And in the most advanced cases, even a complete pericardiectomy can only briefly improve the patient’s condition.
Constrictive pericarditis is one of the diseases that is best prevented. It is extremely important to consult a doctor in time, at the initial stage, when the first signs appear (fatigue, shortness of breath, swelling in the legs). Only he, in a personal meeting, will be able to correctly diagnose and prescribe the correct treatment, which will most likely prevent the development of constriction.
Sources:
- Gilyarevsky S.R. Diagnosis and treatment of pericardial diseases: modern approaches based on evidence-based information and clinical experience. Monograph, M.:Media Sfera, 2004
- European Society of Cardiology (ESC). ESC guidelines for the diagnosis and management of patients with pericardial disease. — Russian Journal of Cardiology No. 5 (133), 2021.
- Baranov A.A. (chief freelance specialist pediatrician of the Russian Ministry of Health, Academician of the Russian Academy of Sciences). Federal clinical guidelines for the provision of medical care to children with pericarditis. — 2015.
Make an appointment with a cardiologist
If you need to get advice from an experienced cardiologist, call by phone in Moscow or fill out the form on our clinic’s website. You can undergo diagnostics directly at the clinic so that the doctor has the necessary data to make a diagnosis and develop an effective treatment regimen.
Remember that the lack of timely treatment of pericarditis can lead to serious complications - the formation of calcium-salt deposits in the heart, the development of heart failure, compression of the heart cavities and the inability of normal contractions.
Diagnostics
Other tests used for diagnosis include:
- a chest x-ray, which shows the shape of the heart and possible excess fluid;
- an electrocardiogram (ECG) to check your heart rhythm and see if the voltage signal is decreasing due to excess fluid;
- an echocardiogram, which will also show the shape, size of the heart and fluid accumulation;
- MRI;
- computed tomography, which provides a detailed image of the heart and pericardium;
- right heart catheterization, which will provide information about the pressure in the heart;
- blood tests to look for inflammatory markers that indicate pericarditis.