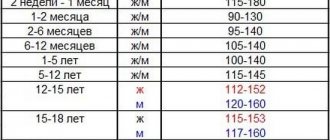
Hemoglobin levels in children vary depending on age and differ from adults.
In children from 6 months to 5 years, anemia is considered to be a decrease in hemoglobin level below 110 g/l, from 5 to 11 years - below 115 g/l; at older ages, the hemoglobin level approaches the norm for adults. Before the age of 6 months, children sometimes experience so-called physiological anemia of newborns, while the hemoglobin level can decrease to 90 g/l, and in the absence of other causes, this condition does not require treatment.
Anemia can be critical to a growing and developing child's body. With low levels of red blood cells and hemoglobin, organs and tissues receive insufficient oxygen. If this condition continues for a long time, the physical, psychomotor and mental development of the child is disrupted. That is why it is important not only timely diagnosis and treatment of anemia, but also its prevention in risk groups.
Causes of anemia
There are many reasons for a decrease in the level of red blood cells, the main ones can be divided into three groups:
- insufficient production of red blood cells;
- premature destruction of red blood cells (hemolysis);
- blood loss
Insufficient production of red blood cells
For the formation of hemoglobin and red blood cells, the body requires microelements such as iron, as well as vitamins B12 and folic acid. With a significant deficiency of these elements, the production of red blood cells decreases and iron-, B12- or folate-deficiency anemia develops. Iron deficiency is the most common cause of anemia in children, especially under 5 years of age.
Red blood cells are formed from progenitor stem cells that are found in the bone marrow. A decrease in the number of stem cells or disruption of their function can also lead to a decrease in the number of red blood cells and the occurrence of anemia. Such conditions may be congenital or acquired.
Premature destruction of red blood cells
Anemia resulting from hemolysis can be observed in children with congenital genetically determined pathologies of erythrocytes, for example, thalassemia or spherocytosis. At older ages, the causes of hemolysis can be autoimmune diseases, infections, taking certain medications, liver and kidney diseases, and a number of other diseases, such as microangiopathy.
Blood loss
Increased loss of red blood cells can be observed with obvious or hidden blood loss. In children and adolescents, among obvious blood losses, nasal and uterine bleeding (heavy menstruation) are most common. Hidden blood loss can be observed in kidney diseases, as well as inflammatory diseases of the gastrointestinal tract.
What is hemoglobin?
Hemoglobin is a very complex protein that consists of four separate proteins - subunits, the holding element of which is an iron atom (Fe). Hemoglobin is contained inside the formed elements of human blood - red blood cells, which in turn make up the main volume of circulating blood, and iron, which is part of hemoglobin, colors the blood of all mammals and humans red. The only function of hemoglobin is to bind oxygen atoms in the lungs and transport this vital element to absolutely all organs and tissues.
This, to briefly explain, is why a person cannot live without hemoglobin, and, accordingly, without the iron that is part of it.
What is the normal hemoglobin level for a child?
A child is normally born with a high hemoglobin content from 150 g/l to 200 - 240 g/l, which is partly caused by the flow of blood from mother to baby during childbirth even before cutting the umbilical cord. But most of the hemoglobin in a newborn is his own fetal hemoglobin, which must be completely replaced with “adult” type hemoglobin by the 3rd month of the child’s life. That is why, by the end of the third month of a baby’s life, the hemoglobin level decreases to 100 - 110 g/l, and this process is a physiological norm, which, as a rule, does not require drug intervention. It is enough to recommend that a nursing mother remember to eat beef or lean pork, or lamb, every day, and also continue to take special vitamins for pregnant women for at least another 3 months after giving birth.
A separate problem is that a number of babies are born premature. Since these children were born earlier than nature’s due date, they did not have time to receive the full norm of necessary vitamins and microelements from their mother, which means that children born prematurely, as well as children whose mothers had low hemoglobin before and during pregnancy, will be in group at risk for developing iron deficiency anemia. An experienced pediatrician will, of course, prescribe iron supplements in the form of drops in a prophylactic dosage to children from the groups I have listed from 2 to 3 weeks of life, without waiting for a strong decrease in hemoglobin.
Starting from the age of 6 months, the lower norm of hemoglobin in a child is 110 g/l. If after this age a child has a hemoglobin level of, for example, 100 or 95 g/l, this is already a reason not only for the earlier introduction of complementary foods, but also for the prescription of iron supplements for replacement purposes.
Low hemoglobin in a child. Prevention of iron deficiency.
In the previous paragraph, we discussed in which cases prophylaxis with iron supplements is indicated for a child.
Now let's touch on the issues of rational nutrition of a child who was born full-term, with a normal hemoglobin level, but after 3 - 4 months his hemoglobin did not exceed the level of 110 g/l.
As we know, the first complementary foods are normally introduced to a child at the age of 4 - 4.5 months with fruit and vegetable purees. If by the age of 5 months we do not see a restoration of the hemoglobin level to 120 g/l, then in order to prevent anemia, we can begin to introduce meat purees from beef, veal or horse meat, lamb into the child’s diet from 5.5 to 6 months (if the child developed an allergy to cow's milk protein).
This is a modern, scientific approach, when, if there is a threat of developing anemia (a decrease in the level of red blood cells and hemoglobin below acceptable values), the child can begin to introduce meat purees as a second type of complementary food as a source of the most easily absorbed heme iron. And thus, by the age of 7 months, our baby can already receive up to 50 grams of meat puree once a day, and after 6 months, he can begin to be introduced to special cereals fortified with iron. I think that this would be more correct than immediately feeding the child a concentrate of iron salts in the form of special drops.
I would also like to warn young mothers, in case the child has low hemoglobin, against the early introduction of chicken and quail eggs. In general, I personally recommend introducing the yolk no earlier than 6.5 - 7 months. But in our case, you need to know that egg yolk, like no other product, reduces the absorption of iron in the intestines due to its high cholesterol content. In other words, feeding your baby yolk and trying to increase iron levels at the same time means throwing good things down the drain. It will not enter the body.
Conversely, fruit complementary foods and vegetable purees such as zucchini or pumpkin significantly improve the absorption of iron. This is due to the presence of vitamins C and folic acid in their composition, which help iron maintain its correct valency and enter our body in a non-oxidized form. But carrot juice should not be given to your baby along with iron.
In addition, milk porridges, especially semolina porridge, also interfere with the absorption of iron. And the worst thing a mother can think of with an infant is to feed him whole cow’s or goat’s milk for up to a year. In this case, if not an allergy, then iron deficiency anemia is definitely guaranteed, since iron from animal milk is practically not absorbed by a human child.
Treatment of anemia in children
However, if by 6 - 8 months the hemoglobin level cannot be normalized, then what should the pediatrician do next? If the doctor is sure that this is definitely iron deficiency anemia, and this can be practically 99% determined by a detailed clinical blood test, calculating the color index, the average hemoglobin content in the erythrocyte, etc., then the only correct decision is to adequately calculate the dose of the drug containing iron, and prescribe a drug such as actiferrin or maltofer for at least 6 weeks.
If the pediatrician is not 100% sure, or if long-term treatment with iron supplements in an adequate, correctly calculated dosage does not lead to normalization of hemoglobin, then in this case I strongly recommend that you consult a pediatric hematologist to establish an accurate diagnosis and exclude hereditary (not associated with iron deficiency) forms of anemia.
Diagnosis of anemia
Anemia in a child can be suspected if there is constant lethargy, tearfulness, irritability, sleep disturbances, poor exercise tolerance, decreased memory and school performance.
On examination, pallor (and in case of hemolysis, jaundice) of the skin, as well as increased heart rate, may be noted.
Depending on the cause of anemia, additional symptoms may include brittle nails, increased hair loss, mouth ulcers, changes in taste (the child may be attracted to inedible foods, such as chalk, soil, ash), numbness in the limbs, muscle pain, enlarged liver and spleen. .
If you suspect
anemia , your doctor may:
- ask about what worries the child;
- inquire about the peculiarities of his diet;
- find out if family members have anemia;
- Conduct a physical examination of the child.
To confirm the diagnosis, the doctor will prescribe the necessary tests:
- clinical blood test,
- blood test for reticulocytes;
- blood chemistry;
- general urinalysis, stool analysis;
- test for the presence of hereditary anemia;
- bone marrow stem cell research;
- Ultrasound, endoscopic examinations.
If a malfunction of bone marrow stem cells is suspected, studies such as a myelogram, cytogenetic, and molecular biological studies of the bone marrow are performed. To obtain the material, a bone puncture is performed with a special needle. For children, this procedure is performed under general anesthesia.
Normal hemoglobin level in children
Henry Weizmann, a researcher at the French Institute of Health and Medicine, explains that hemoglobin is a complex protein molecule that contains iron. It is found in erythrocytes (red blood cells) and performs several important functions:
- transports oxygen from the lungs to all cells and tissues of the body;
- takes carbon dioxide from them and returns it to the lungs;
- participates in maintaining acid-base balance in the blood.
The amount of hemoglobin in the blood depends on the age of the person. Thus, in newborns its level is significantly increased and ranges from 145–225 g/l, but from the first day of life the figure gradually falls.
What is the normal hemoglobin level in children under one year of age? According to WHO data, the content of this protein in the blood of children of the first year of life decreases from the level of a newborn to 135 g/l by 5–6 months and from 110 g/l at the age of 1 year.
What is the normal hemoglobin level in children? The amount, according to S. A. Esakov’s textbook “Age Anatomy and Physiology,” depends on the age of the child and is measured in grams per 1 liter of blood:
Hemoglobin norm in children: NUR.KZ
If the hemoglobin level is low, there are complaints about:
- weakness;
- drowsiness;
- decreased appetite;
- dizziness;
- change in taste;
- dry skin, brittle nails and hair loss;
- the appearance of sticking in the corners of the mouth.
Why is low hemoglobin dangerous? Therapist Carol DerSarksiyan explains that the condition may indicate both poor nutrition and a sedentary lifestyle, and the presence of pathological processes (hidden blood loss, anemia, infectious and autoimmune diseases). Therefore, if a reduced level is detected, a doctor’s consultation is necessary to prescribe iron-containing drugs and correct the diet.
Hemoglobin in Children: Pexels
It is worth remembering that increased hemoglobin is no less dangerous than low one. The rate increases with some blood diseases and cancer. External manifestations resemble signs of hepatitis:
- icteric color of the skin, sclera, palate and tongue;
- skin itching;
- liver enlargement;
- cardiac dysfunction;
- pallor and thinness.
In this situation, it is necessary to consult a doctor and prescribe treatment.